Abstract
Background
The importance of the patient experience is increasingly being recognised. However, there is a dearth of studies regarding factors affecting patient-reported outcomes in emergency general surgery (EGS), including none from the Southern Hemisphere. We aim to prospectively assess factors associated with patient satisfaction in this setting.
Methods
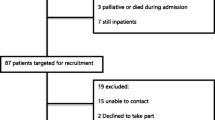
In this prospective cross-sectional study, all consecutive adult patients admitted to an acute surgical unit over four weeks were invited to complete a validated Patient-Reported Experience Measures questionnaire. These were completed either in person when discharge was imminent or by telephone <4 weeks post-discharge. Responses were used to determine factors associated with overall patient satisfaction.
Results
From 146 eligible patients, 100 (68%) completed the questionnaire, with a mean overall satisfaction score of 8.3/10. On multivariate analyses, eight factors were significantly associated with increased overall satisfaction. Five of these were similar to those previously prescribed by other like studies, being patient age >50 years, sufficient analgesia, satisfaction with the level of senior medical staff, important questions answered by nurses and confidence in decisions made about treatment. Three identified factors were new: sufficient privacy in the emergency department, sufficient notice prior to discharge and feeling well looked after in hospital.
Conclusions
Factors associated with patient satisfaction were identified at multiple points of the patient journey. While some of these have been reported in similar studies, most differed. Hospitals should assess factors valued by their EGS population prior to implementing initiatives to improve patient satisfaction.
Similar content being viewed by others
References
Jones CH, O’Neill S, McLean KA et al (2017) Patient experience and overall satisfaction after emergency abdominal surgery. BMC Surg 17(1):76
Priebe S, Golden E, McCabe R et al (2012) Patient-reported outcome data generated in a clinical intervention in community mental health care-psychometric properties. BMC Psychiatry 12:113
Varni JW, Burwinkle TM, Seid M (2005) The PedsQL as a pediatric patient-reported outcome: reliability and validity of the PedsQL measurement model in 25,000 children. Expert Rev Pharmacoecon Outcomes Res 5(6):705–719
Apers S, Kovacs AH, Luyckx K et al (2015) Assessment of Patterns of patient-reported outcomes in adults with congenital heart disease-international study (APPROACH-IS): rationale, design, and methods. Int J Cardiol 179:334–342
Dickfos M, Ibrahim H, Evans A et al (2018) Cohort study on emergency general surgery patients and an observation unit. ANZ J Surg 88(7–8):713–717
Page D, Dooreemeah D, Thiruchelvam D (2014) Acute surgical unit: the Australasian experience. ANZ J Surg 84:25–30
Bazzi ZT, Kinnear N, Bazzi CS et al (2018) Impact of an acute surgical unit on outcomes in acute cholecystitis. ANZ J Surg 88(12):E835–E839
Kinnear N, Bramwell E, Frazetto A et al (2019) The acute surgical unit improves outcomes in appendicectomy. ANZ J Surg. https://doi.org/10.1111/ans15141
Kinnear N, Britten-Jones P, Hennessey D et al (2017) Impact of an acute surgical unit on patient outcomes in South Australia. ANZ J Surg 87(10):825–829
DeGirolamo K, Murphy PB, D’Souza K et al (2017) Processes of health care delivery, education, and provider satisfaction in acute care surgery: a systematic review. Am Surg 83(12):1438–1446
Kinnear N, Tran M, Han J et al (2019) Does emergency general surgery model affect staff satisfaction, training and working hours? ANZ J Surg 90(3):262–267
Maa J, Carter JT, Gosnell JE et al (2007) The surgical hospitalist: a new model for emergency surgical care. J Am Coll Surg 205(5):704–711
Anantha RV, Parry N, Vogt K et al (2014) Implementation of an acute care emergency surgical service: a cost analysis from the surgeon’s perspective. Can J Surg 57(2):E9–E14
Schmocker RK, Cherney Stafford LM, Siy AB et al (2015) Understanding the determinants of patient satisfaction with surgical care using the Consumer Assessment of Healthcare Providers and Systems surgical care survey (S-CAHPS). Surgery (United States) 158(6):1724–1733
Kahn SA, Iannuzzi JC, Stassen NA et al (2015) Measuring satisfaction: factors that drive hospital consumer assessment of healthcare providers and systems survey responses in a trauma and acute care surgery population. Am Surg 81(5):537–543
Hommel G (1988) A stagewise rejective multiple test procedure based on a modified Bonferroni test. Biometrika 75(2):383–386
R Core Team (2017) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna. https://www.R-project.org/
Forrestal B, Hynes T, Clarke-Moloney M et al (2013) Patient satisfaction following emergency admission via a surgical assessment unit and an emergency department. Ir J Med Sci 182(2):261–266
Kwong E, Neuburger J, Murray D et al (2018) Feasibility of collecting and assessing patient-reported outcomes for emergency admissions: laparotomy for gastrointestinal conditions. BMJ Open Gastroenterol 5(1):e000238
Navarro AP, Hardy E, Oakley B et al (2017) The front-line general surgery consultant as a new model of emergency care. Ann R Coll Surg Engl 99(7):550–554
Ali TF, Warkentin LM, Gazala S et al (2015) Self-reported outcomes in individuals aged 65 and older admitted for treatment to an acute care surgical service: a 6-month prospective cohort study. J Am Geriatr Soc 63(11):2388–2394
Eijsvoogel CF, Peters RW, Budding AJ et al (2014) Implementation of an acute surgical admission ward. Br J Surg 101(11):1434–1438
Ullah MF, Fleming C, Fox C et al (2019) Patient experience in a surgical assessment unit following a closed-loop audit using a Kaizen Lean system. Ir J Med Sci 189(2):641–647
Johnstone C, Harwood R, Gilliam A et al (2015) A clinical decisions unit improves emergency general surgery care delivery. Clin Gov Int J 20(4):191–198
National Health Service (2010) Equity and excellence: liberating the NHS. Department of Health [Internet]. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/213823/dh_117794.pdf. Accessed 25 Nov 2019
Nilsson E, Orwelius L, Kristenson M (2016) Patient-reported outcomes in the Swedish National Quality Registers. J Intern Med 279(2):141–153
US Dept of Health and Human Services, Food and Drug Administration USA (2006) Guidance for industry: patient-reported outcome measures: use in medical product development to support labeling claims: draft guidance. Health Qual Life Outcomes 4:79
Williams K, Sansoni J, Morris D et al (2016) Patient-reported outcome measures: literature review. ACSQHC [Internet]. https://www.safetyandquality.gov.au/sites/default/files/migrated/PROMs-Literature-Review-December-2016.pdf. Accessed 25 Nov 2019
Waljee JF, Ghaferi A, Cassidy R et al (2016) Are patient-reported outcomes correlated with clinical outcomes after surgery? A population-based study. Ann Surg 264(4):682–689
Schlesinger M, Grob R, Shaller D (2015) Using patient-reported information to improve clinical practice. Health Serv Res 50(Suppl 2):2116–2154
Allcock C (2015) Outcomes-based commissioning—much promise, but is it something that CCGs can actually deliver on? The Health Foundation, London. http://www.health.org.uk/blog/outcomes-based-commissioning-much-promise-it-something-ccgs-can-actually-deliver. Accessed 01 Dec 2019
Australian Commission on Safety and Quality in Health Care and Australian Institute of Health and Welfare (2010) Australian safety and quality framework for health care. ACSQHC, Sydney. https://www.safetyandquality.gov.au/sites/default/files/migrated/Australian-SandQ-Framework1.pdf. Accessed 01 Dec 2019
Bennett AV, Jensen RE, Basch E (2012) Electronic patient-reported outcome systems in oncology clinical practice. CA Cancer J Clin 62(5):337–347
Weldring T, Smith SM (2013) Patient-reported outcomes (PROs) and Patient-reported outcome measures (PROMs). Health Serv Insights 6:61–68
Cella D, Yount S, Rothrock N et al (2007) The Patient-reported outcomes measurement information system (PROMIS): progress of an NIH roadmap cooperative group during its first two years. Med Care 45(5 Suppl 1):S3–S11
Bradley M, Braverman J, Harrington M et al (2016) Patients’ motivations and interest in research: characteristics of volunteers for patient-led projects on PatientsLikeMe. Res Involv Engagem 2:33
Bennett AV, Dueck AC, Mitchell SA et al (2016) Mode equivalence and acceptability of tablet computer-, interactive voice response system-, and paper-based administration of the U.S. National Cancer Institute’s Patient-Reported Outcomes version of the Common Terminology Criteria for Adverse Events (PRO-CTCAE). Health Qual Life Outcomes 14:24
Acknowledgements
This research was supported by funding from the University of Adelaide and its Adelaide Graduate Centre, as well as the Hospital Research Foundation, National Health and Medical Research Council postgraduate scholarship and the Royal Australasian College of Surgeons. No preregistration exists for this study. Requests to access the dataset from qualified researchers trained in human subject confidentiality protocols may be sent to Ned Kinnear at Ned.Kinnear@adelaide.edu.au.
Funding
In relation to this work, Ned Kinnear received a University of Adelaide Research Training Program Scholarship, a Hospital Research Foundation postgraduate scholarship, a National Health and Medical Research Council postgraduate scholarship and the Brendan Dooley and Gordon Trinca Trauma Research Scholarship from the Royal Australasian College of Surgeons. However, no funders influenced the study, nor had access to the manuscript prior to publication. For the remaining authors, no relevant sources of funding were declared.
Author information
Authors and Affiliations
Contributions
NK created the report concept, performed data analysis and wrote the initial manuscript. MH, SJ, JH, MT and DP performed data collection. NK and SJ performed literature review. MH, SJ, DP, DH, CD, TS and JM guided the scope and approach of the study and refined the manuscript. MOC performed statistical analyses. All authors refined the final manuscript and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kinnear, N., Herath, M., Jolly, S. et al. Patient Satisfaction in Emergency General Surgery: A Prospective Cross-Sectional Study. World J Surg 44, 2950–2958 (2020). https://doi.org/10.1007/s00268-020-05561-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05561-8