Abstract
Background
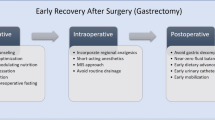
Enhanced Recovery After Surgery (ERAS) perioperative pathways are safe and effective for patients undergoing gastrectomy. However, adherence to these protocols varies and is generally underreported. This retrospective study aimed to assess whether perioperative variables or deviation from ERAS items is associated with delayed discharge after gastrectomy.
Methods
All patients undergoing gastrectomy at our institution were managed with a standardised perioperative pathway according to ERAS principles. The target length of stay was set as the ninth post-operative day (POD). All significant variables were derived from a bivariate analysis and were entered into a logistic regression to confirm their statistical value.
Results
The study included 180 patients. Multivariate regression analysis revealed that incomplete immunonutrition, failure to extubate the patient at the end of surgery, intraoperative crystalloids >2150 ml and blood transfusion >268 ml, surgery duration >195 min, and failure to mobilise patients within 24 h from surgery were associated with delayed discharge. The logistic regression model was statistically significant (p < 0.001) and correctly classified 73.6% of cases. Sensitivity and specificity were 74.1% and 73.2%, respectively.
Conclusions
These results seem clinically significant and consistent with those of previous studies. The reported perioperative variables showed a strong relationship with the length of hospital stay.

Similar content being viewed by others
References
Ferlay J et al (2015) Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 136:E359–E386. https://doi.org/10.1002/ijc.29210
Ding J et al (2017) The application of enhanced recovery after surgery (ERAS)/fast-track surgery in gastrectomy for gastric cancer: a systematic review and meta-analysis. Oncotarget 8:75699–75711. https://doi.org/10.18632/oncotarget.18581
Pisarska M et al (2017) Laparoscopic gastrectomy with enhanced recovery after surgery protocol: single-center experience. Med Sci Monit 23:1421–1427
Wilmore DW, Kehlet H (2001) Management of patients in fast track surgery. BMJ 322:473–476
Kehlet H, Wilmore DW (2002) Multimodal strategies to improve surgical outcome. Am J Surg 183:630–641
Schwenk W, Neudecker J, Raue W et al (2006) “Fast-track” rehabilitation after rectal cancer resection. Int J Colorectal Dis 21:547–553. https://doi.org/10.1007/s00384-005-0056-7
Polle SW et al (2007) Implementation of a fast-track perioperative care program: what are the difficulties? Dig Surg 24:441–449. https://doi.org/10.1159/000108327
Zhuang CL, Ye XZ, Zhang XD et al (2013) Enhanced recovery after surgery programs versus traditional care for colorectal surgery: a meta-analysis of randomized controlled trials. Dis Colon Rectum 56:667–678. https://doi.org/10.1097/DCR.0b013e3182812842
Pruthi RS et al (2010) Fast track program in patients undergoing radical cystectomy: results in 362 consecutive patients. J Am Coll Surg 210:93–99. https://doi.org/10.1016/j.jamcollsurg.2009.09.026
Barletta JF, Miedema SL, Wiseman D et al (2009) Impact of dexmedetomidine on analgesic requirements in patients after cardiac surgery in a fast-track recovery room setting. Pharmacotherapy 29:1427–1432. https://doi.org/10.1592/phco.29.12.1427
Kroon UB, Radstrom M, Hjelthe C et al (2010) Fast-track hysterectomy: a randomised, controlled study. Eur J Obstet Gynecol Reprod Biol 151:203–207. https://doi.org/10.1016/j.ejogrb.2010.04.001
Andersen LO et al (2009) Subacute pain and function after fast-track hip and knee arthroplasty. Anaesthesia 64:508–513. https://doi.org/10.1111/j.1365-2044.2008.05831.x
Das-Neves-Pereira JC et al (2009) Fast-track rehabilitation for lung cancer lobectomy: a five-year experience. Eur J Cardio-Thorac Surg 36(2):383–392. https://doi.org/10.1016/j.ejcts.2009.02.020
Li YJ et al (2014) Meta-analysis of efficacy and safety of fast-track surgery in gastrectomy for gastric cancer. World J Surg 38:3142–3151. https://doi.org/10.1007/s00268-014-2690-0
Mortensen K et al (2014) Consensus guidelines for enhanced recovery after gastrectomy: Enhanced Recovery After Surgery (ERAS(R)) Society recommendations. Br J Surg 101:1209–1229. https://doi.org/10.1002/bjs.9582
Bursac Z, Gauss CH, Williams DK et al (2008) Purposeful selection of variables in logistic regression. Source Code Biol Med 3:17. https://doi.org/10.1186/1751-0473-3-17
Braga M, Gianotti L, Vignali A et al (1998) Immunonutrition in gastric cancer surgical patients. Nutrition 14:831–835
Braga M et al (1999) Perioperative immunonutrition in patients undergoing cancer surgery: results of a randomized double-blind phase 3 trial. Arch Surg 134:428–433
August DA, Huhmann MB, American Society for Pareteral and Enteral Nutrition (A.S.P.E.N.) (2009) Clinical guidelines: nutrition support therapy during adult anticancer treatment and in hematopoietic cell transplantation. JPEN J Parenter Enteral Nutr 33:472–500. https://doi.org/10.1177/0148607109341804
Arends J et al (2017) ESPEN guidelines on nutrition in cancer patients. Clin Nutr 36:11–48. https://doi.org/10.1016/j.clnu.2016.07.015
Fujitani K, Tsujinaka T, Fujita J, Miyashiro I, Imamura H, Kimura Y, Kobayashi K, Kurokawa Y, Shimokawa T, Furukawa H, Osaka Gastrointestinal Cancer Chemotherapy Study Group (2012) Prospective randomized trial of preoperative enteral immunonutrition followed by elective total gastrectomy for gastric cancer. Br J Surg 99(5):621–629. https://doi.org/10.1002/bjs.8706
Ramagem CA et al (2015) Comparison of laparoscopic total gastrectomy and laparotomic total gastrectomy for gastric cancer. Arq Bras Cir Dig 28:65–69. https://doi.org/10.1590/S0102-67202015000100017
Fuchs KH (2002) Minimally invasive surgery. Endoscopy 34:154–159. https://doi.org/10.1055/s-2002-19857
Quan Y et al (2016) Comparison of laparoscopic versus open gastrectomy for advanced gastric cancer: an updated meta-analysis. Gastric Cancer 19:939–950. https://doi.org/10.1007/s10120-015-0516-x
Jiang ZW et al (2015) Single-incision laparoscopic distal gastrectomy for early gastric cancer through a homemade single port access device. Hepatogastroenterology 62:518–523
Chen S, Zou Z, Chen F et al (2015) Meta-analysis of fast track surgery for patients with gastric cancer undergoing gastrectomy. Ann R Coll Surg Engl 97:3–10. https://doi.org/10.1308/rcsann.2015.97.1.3
Aoyama T et al (2014) Randomized comparison of surgical stress and the nutritional status between laparoscopy-assisted and open distal gastrectomy for gastric cancer. Ann Surg Oncol 21:1983–1990. https://doi.org/10.1245/s10434-014-3509-9
Schmidt HM, El Lakis MA, Markar SR et al (2016) Accelerated recovery within standardized recovery pathways after esophagectomy: a prospective cohort study assessing the effects of early discharge on outcomes, readmissions, patient satisfaction, and costs. Ann Thorac Surg 102:931–939. https://doi.org/10.1016/j.athoracsur.2016.04.005
Dorcaratto D, Grande L, Pera M (2013) Enhanced recovery in gastrointestinal surgery: upper gastrointestinal surgery. Dig Surg 30:70–78. https://doi.org/10.1159/000350701
Jeong Oh, Park Young Kyu, Jung Mi Ran et al (2017) Compliance with guidelines of enhanced recovery after surgery in elderly patients undergoing gastrectomy. World J Surg 41:1040–1046. https://doi.org/10.1007/s00268-016-3845-y
Smart NJ et al (2012) Deviation and failure of enhanced recovery after surgery following laparoscopic colorectal surgery: early prediction model. Colorectal Dis 14:e727–e734. https://doi.org/10.1111/j.1463-1318.2012.03096.x
Sun CF, Hsieh YY, Ngan KW et al (2001) Search for immunomodulatory effects of blood transfusion in gastric cancer patients: flow cytometry of Th1/Th2 cells in peripheral blood. Ann Clin Lab Sci 31:171–178
Jackson KL et al (2013) Does travel distance influence length of stay in elective colorectal surgery? Dis Colon Rectum 56:367–373. https://doi.org/10.1097/DCR.0b013e31827e939e
Jackson KL et al (2014) Does travel distance influence length of stay in elective pancreatic surgery? HPB (Oxford) 16:543–549. https://doi.org/10.1111/hpb.12180
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
This study was conducted according to the Declaration of Helsinki, and all patients provided written informed consent.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Parise, P., Cinelli, L., Ferrari, C. et al. Early Red Flags Associated with Delayed Discharge in Patients Undergoing Gastrectomy: Analysis of Perioperative Variables and ERAS Protocol Items. World J Surg 44, 223–231 (2020). https://doi.org/10.1007/s00268-019-05223-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-019-05223-4