Abstract
Background
Intraoperative hypothermia is a common adverse event. For avoiding the complication due to hypothermia, many warming devices and methods have been used in perioperative period. It has been reported that more patients undergoing laparoscopic surgery tend to have hypothermia than with open surgery. To avoid intraoperative hypothermia, many kinds of warming tools have been used. But, it was also reported that some warming methods increased perceptions of distraction and physical demand.
Methods
To achieve both patients’ normothermia and surgeons’ comfort, new air conditioning (AC) system was designed with considering the characteristics of laparoscopic surgery. The temperature of the airflows to the patient and to the surgeons can be adjusted independently in this new system. The new system has two parts. One controls the temperature of the central area over the operation table. The air from this part falls on the patients. The other part is the lateral area beside the operating table; the air from this part falls on the surgeons. The subjects of this study were 160 gastric cancer patients and 316 colorectal cancer patients undergoing laparoscopic surgery. The temperature of the central flow was set 23.5 °C, and the temperature of the lateral flow was set 22 °C just after the anesthesia. The number of timepoints the patient spent in hypothermic state, defined as a temperature cooler by 0.5 °C or more than that at the starting point of surgery, was determined in each patient.
Results
In the results, the rate of hypothermic state in old operation rooms was 23.8% and that in new operation rooms was 2.7% in male gastric cancer patients (p < 0.01). And those were 37.1% in old operation rooms and 0.9% in new operation rooms in female gastric cancer patients (p < 0.01). The rate of hypothermic state in old operation rooms was 30.0% and that in new operation rooms was 9.5% in male colorectal cancer patients (p < 0.01). And those were 41.6% in old operation rooms and 8.9% in new operation rooms in female colorectal cancer patients (p < 0.01). The similar results were showed in the study, which subjects were limited the patients undergoing surgery in 2015 and 2016; which were the last year the old operation rooms were used and the first year the new operation rooms were used.
Conclusions
Thus, the usefulness of the new air conditioning system for achieving both patients’ normothermia and comfort of surgeons could be verified in this study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intraoperative hypothermia is a common adverse event. It was reported that more patients tended to have hypothermia among those undergoing laparoscopic surgery compared to those undergoing open surgery [1,2,3]. In laparoscopic surgery, a large area of the patient’s skin is exposed to the room air, and it is difficult to warm the patient’s body. The cold and dry carbon dioxide gas used to induce pneumoperitoneum is another likely cause of hypothermia [1, 2]. One of the most important and overlooked problems, which is common with open surgery, is that there is often a discrepancy between the most comfortable temperature for the patient and that for the surgeons. During many surgeries, the patient is mostly naked and lying on an unheated operative table. A surgeon wears a surgical gown and faces rigorous mental and physical challenges involved in surgery. The temperature that is comfortable for the patient is often too hot for the surgeon, and thus, the surgeon may ask that the operating room (OR) temperature be lowered. This easily leads to hypothermia in patients, whose blood vessels are dilated by anesthetics.
For the precise control of patients’ body temperatures while maintaining surgeons’ comfort, a new concept air conditioning (AC) system was adopted in the newly constructed ORs at Kagawa University Hospital. In the present study, the body temperatures and the amount of bleeding of patients undergoing laparoscopic surgery in the new ORs with the AC system were compared with those of patients undergoing laparoscopic surgery in the ‘old’ ORs without the AC system in order to evaluate the effects and utility of the new AC system. OR nurses were interviewed about the surgeon’s reports concerning the AC, as an evaluation of the surgeons’ comfort.
Patients and methods
Patients
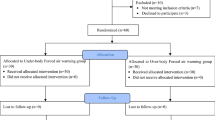
The subjects of this study were 160 gastric cancer (GC) patients and 316 colorectal cancer (CC) patients who underwent laparoscopic surgery in an OR at Kagawa University Hospital during the >7-year period from January 2011 to February 2018. The hospital’s new ORs were completed at the end of December 2015. The patients who underwent surgery in either an old or new OR were the subjects of the first part of this study (Table 1).
In the second part of the study, the cases of only the patients who underwent laparoscopic surgery in 2015 (the last year of the old ORs) or 2016 (the first year of the new ORs) were examined. This more limited population was selected to keep the surgical staff as consistent as possible (Table 2). This study was approved by the ethics committee of Kagawa University (approval no. 2017-014), and the requirement for informed consent was waived for this retrospective analysis.
Patient position and warming tools
All patients underwent the surgeries in the lithotomy position. Their chest and upper limbs were warmed using devices with warmed air bags. The backs of the GC patients were also warmed by a warm blanket, but the backs of the CC patients could not be warmed due to the use of a body-fixing device for maintaining the Trendelenburg position during surgery. The intravenous fluid was not warmed [4]. No amino acid administrations were used on our patients [5,6,7]. The carbon dioxide gas for pneumoperitoneum was neither humidified nor warmed [8, 9].
The new air conditioning system
Each of the new AC systems set into the ceiling of the hospital’s new ORs has a high-efficiency particulate air filter (HEPA filter) for infection control, as is common in ORs [10]. However, there is a key difference from previous operating room AC systems. The new system has two parts. One controls the temperature of the central area over the operation table; the airflow from this part of the AC falls on the patient. The other part is the lateral area beside the operating table; the AC’s airflow for this falls on the surgeon(s). The temperatures of the airflow to the patient and the airflow to the surgeon can be adjusted independently. Thus, the patient on the operation table can be warmed by the central airflow and the surgeon can be cooled by the lateral airflow. The cost of the new AC system was 6.7% higher than that of the previous AC system used in the old ORs.
Control of the airflows temperatures
In the old ORs, the temperature of the airflow of the single AC system was controlled at 25 °C before the patients were brought into the OR. After anesthesia was administered, the temperature was set at the temperature preferred by the surgeons. In the new ORs, the temperature of the airflows of both the central and lateral AC system was kept at 25 °C before the patients were brought into the ORs. Immediately after the induction of anesthesia, the temperature of the central flow was changed to 23.5 °C, and the temperature of the lateral flow was changed to 22 °C. After that, the temperature of both airflows was controlled as directed by the surgeon.
Sampling and computation of measured temperatures
The body temperature of each patient was measured continuously by a sensor that was inserted into the bladder. The temperatures were archived in the anesthetic record automatically. The patient’s body temperature just before the surgery and the body temperature every 10 min from 10 to 100 min after the start of surgery were recorded. The differences between the body temperature at the starting point of surgery and the body temperature at each 10-min checkpoint were calculated. The number of timepoints the patient spent in a hypothermic state, defined as a temperature cooler by ≥0.5 °C more than that at the starting point of surgery, was determined in each patient.
Evaluation of body temperature
The frequencies of the hypothermic state in the patients undergoing surgery in the old ORs (the ‘old OR group’) were compared with the frequencies in the new ORs (the ‘new OR group’). The data of the patients who underwent surgery during the years from 2011 to 2015 were compared with those of the patients who underwent surgery from the beginning of 2016 to February 2018. The data of the patients who underwent surgery in 2015 (in the old ORs) were compared with the data of the patients who underwent surgery in 2016 (in the new ORs). Separate evaluations were performed for the male and female patients with either type of cancer (GC or CC).
Bleeding
The amount of bleeding in the operation period of all patients was extracted from the anesthetic records. The bleeding amounts of the old OR group were compared with those of the new OR group. The rate of patients receiving a blood transfusion was compared between the old and new OR groups.
Interview regarding surgeons’ assessments of the new AC system
There were 46 nurses in the hospital’s operative theater during the study period. For the present study, the chief nurse interviewed the OR nurses. She asked the nurses whether or not a surgeon had expressed any concerns or problems regarding the new AC system, during or after a surgery. The interview results were reported by the chief nurse to the study investigator.
Statistical analysis
The Chi-square test and Student’s t test were used to compare differences between patient groups and interview results.
Results
The patients body temperature
Gastric cancer
-
(1)
The male GC patients
Ten timepoints per patient were used for the evaluation. However, in two patients who underwent surgery in an old OR, the laparoscopic procedure was finished only 80 min after the start of the surgery. Thus, there were 726 timepoints of the 73 male patients who underwent surgery for GC in the old ORs and 300 timepoints of the 30 male patients in the new ORs; for each timepoint, it was determined whether or not the patient’s body temperature revealed that he was in a hypothermic state. The rate of hypothermic states among the male GC patients was 23.8% in the old OR group and significantly lower at 2.7% in the new OR group (p < 0.01) (Fig. 1).
- (2)
The female GC patients
There were 340 timepoints for the 34 female GC patients who underwent surgery in the old ORs and 230 timepoints for the 23 female GC patients in the new ORs. The rate of hypothermic state was 37.1% in the old OR group and significantly lower at 0.9% in the new OR group (p < 0.01) (Fig. 1).
Colorectal cancer
- (1)
The male CC patients
In four of the male patients whose surgery for CC was performed in an old OR, the laparoscopic procedure lasted only 40, 60, 60 and 70 min; among those whose surgery was in a new OR, there was one patient whose surgery lasted only 70 min. Thus, there were 1133 timepoints of the 115 patients who underwent surgery in the old ORs and 717 timepoints of the 72 patients in the new ORs. The rate of hypothermic states was 30.0% in the old OR group and significantly lower at 9.5% in the new OR group (p < 0.01) (Fig. 2).
- (2)
The female CC patients
In five of the female patients whose laparoscopic surgery for CC was conducted in an old OR, the procedure ended only 40, 60, 60, 60 and 90 min after the start of the surgery. Thus, there were 891 timepoints of the 91 female patients in the old ORs and 380 timepoints of the 38 patients in the new ORs. The rate of hypothermic states was high at 41.6% in the old OR group and significantly lower at 8.9% in the new OR group (p < 0.01) (Fig. 2).
The patients’ body temperatures in 2015 versus 2016
The analyses of only the patients who underwent surgery in 2015 or 2016 revealed the following findings.
Gastric cancer cases in 2015 (‘old ORs’) versus 2016 (‘new ORs’)
- (1)
The male GC patients
There were 140 timepoints of the male GC patients in the old ORs (i.e., those used in 2015) and 140 timepoints of those in the new ORs (used in 2016). The rate of hypothermic states was 23.6% in the old OR group and significantly lower at 4.3% in the new OR group (p < 0.01) (Fig. 3).
- (2)
The female GC patients
There were 90 timepoints of the female GC patients who underwent surgery in the old ORs and 120 timepoints of those in the new ORs. The rate of hypothermic states was 27.8% in the old OR group and 1.7% in the new OR group (p < 0.01) (Fig. 3).
Colorectal cancer
- (1)
The male CC patients
There was one new OR patient whose laparoscopic surgery was finished only 70 min after the start of the surgery. There were thus 310 timepoints of 31 male CC patients undergoing surgery in the old ORs and 347 timepoints of 35 patients in the new ORs. The rate of hypothermic states was 25.2% in the old OR group and significantly lower at 10.4% in the new OR group (p < 0.01) (Fig. 4).
- (2)
The female CC patients
There were 180 timepoints of female CC patients who underwent surgery in old ORs and 210 timepoints of patients in the new ORs. The hypothermic rate was 20.6% in the old OR group and significantly lower at 11.0% in the new OR group (p < 0.01) (Fig. 4).
Bleeding amounts
Gastric cancer
The amount of bleeding of all of the old OR patients with GC was 100.5 ± 122.3 g and that of the all of the new OR patients was significantly lower at 55.4 ± 91.8 g (p = 0.02). There were three patients who received a blood transfusion in the old OR group, and none in the new OR group.
Colorectal cancer
The amount of bleeding of all of the old OR patients with CC was 137.2 ± 329.0 g, and that of all the new OR patients was 133.7 ± 343.1 g. This difference was not significant. Eight old OR patients and one new OR patient received a blood transfusion.
Surgeons comfort
None of the surgical nurses reported hearing any type of grievance from a surgeon regarding the new AC system for the ORs.
Discussion
Intraoperative hypothermia causes many complications. Patients with hypothermia tend to have delayed awakening from anesthesia [11]. The body’s serum adrenalin level rises in the hypothermic state, and this causes a peripheral circulatory insufficiency and increases the risk of myocardial ischemia [12]. The hypothermic state augments blood loss and the transfusion requirement [13, 14]. Hypothermia was also reported to cause immunosuppression [15, 16] and to influence tumor growth and worsen the prognosis of cancer patients [3, 16]. Moreover, patients with intraoperative hypothermia tend to have more surgical site infections [17, 18], and the hypothermia affects patients’ outcomes [5, 6, 17]. Thus, the 2017 US Centers for Disease Control (CDC) guidelines highly recommend that the intraoperative body temperatures of patients are adequately controlled [19].
Many approaches have been used in attempts to avoid patients’ intraoperative hypothermia. The effectiveness of warmed intravenous fluid [4] and the usefulness of amino acid administration [5,6,7] have been described. The utility of patient prewarming before surgery has been studied [20, 21], and many types of warming tools have been used intraoperatively [22,23,24]. However, the area of skin surface warmed by such tools is much narrower in laparoscopic surgery than in open surgery, and warming tools are therefore not always effective for patients undergoing laparoscopic surgery. It was also reported that the warming tools did not influence surgeons’ technical performance in short operative tasks, but the tools increased surgeons’ perceptions of distraction and might influence their performance in long-duration operations [25]. The surgeons’ comfort should thus be considered when testing warming tools and AC systems.
For the prevention of intraoperative hypothermia in patients while maintaining the surgeons’ comfort, a new countermeasure was implemented at our hospital, i.e., a new AC system was installed in every OR after an initial investigation in an experimental room. To verify the merits of the new system, the present study determined the frequencies of the hypothermic state in patients undergoing laparoscopic surgery in the old and new ORs. Hypothermia has been defined as a body temperature ‘lower than 36 °C’ [26]. In the present patient series, the body temperatures of the GC patients before surgery showed a 2.0 °C difference (35.3–37.3 °C) and that of the CC patients showed a 2.8 °C difference (35–37.8 °C). Thus, the precise effect of the AC system cannot be evaluated by using the absolute value of body temperature, and the hypothermic state was defined herein as a temperature cooler by ≥0.5 °C compared to that at the starting point of surgery.
An earlier study at our hospital demonstrated that the patient’s gender affects the body temperature of patients undergoing laparoscopic surgery [27, 28]. The reason for this phenomenon is that male patients have rich visceral adipose tissue protecting the mesenteric vessels from the cold carbon dioxide gas, whereas the visceral adipose tissue of female patients is much thinner. The frequencies of the hypothermic state of the males and females were thus evaluated separately in the present analyses.
The first part of this study revealed significant reductions in the frequency of the hypothermic state in the new ORs compared to the frequencies observed in the old ORs, suggesting the effectiveness of the new AC system. However, anesthesiologists and nurses in operation theaters often switch hospitals or change assignments within the hospital. It is undeniable that within the approximately 7-year study period, these changes could introduce significant differences in techniques that would affect the patients and the rate of hypothermia. Thus, only the GC and CC patients operated on in 2015 and 2016 at our hospital were selected for the second analysis, to exclude the influence of the turnover of staff in the operative theater to the greatest extent possible.
The difference in the amount of bleeding between the old OR and new OR groups among GC patients and the blood transfusion results may reflect the effect of the new AC system, but some surgeons switched hospitals during the study period. It thus cannot be declared that the new AC system is able to decrease the perioperative complication of hypothermia. Other complications such as anastomotic leakage were not examined, because these complications are more influenced by the technique of each surgeon, some of whom left the hospital.
The present results indicate that the new two-airflow AC system is useful for maintaining the body temperature of patients undergoing laparoscopic surgery. The effect of this system seems to be derived not only from the warm airflow for the patients but also from the cool airflow for the surgeons. The results of the nurse interviews revealed that none of the surgeons were dissatisfied with the new AC system. The reason for this result may be that with the new AC system, the surgeons can control the temperature of both airflows freely if they become uncomfortable. In other words, the surgeons were satisfied with the AC system by receiving the cool airflow, and lowering the temperature of the airflow on them will not lower the body temperature of the patients. Alternatively, even if the surgeons become too hot and lower the temperature of the ‘surgeons’ airflow,’ the warm airflow for the patients prevents the patients’ hypothermia. There was no instance of lowering the temperature of both airflows which would affect the patient’s body temperature. The new AC system seems to be effective at keeping surgeons comfortable. The surgeons tended not to dictate the lowering of the temperature of the airflow to the patients. The concept of the new AC system in an OR has been to cool the surgeons rather than warm the patient. This is the most important point. The new two-airflow AC system provides a completely new method for warming patients in the OR.
In addition, the new AC system has some merits that are particular to laparoscopic surgery. In terms of the surgeons’ posture during an operation, they stand erect in laparoscopic surgery so that only the laterally flowing cool airflow falls on them, whereas they tend to take a somewhat stooped or bent-over posture in open surgery such that some of the warm airflow would blow on their heads. In laparoscopic surgery, the surgeons are not influenced by the warm air falling on the patient, and they can maintain their comfort. The warm air falling on the patient is not obstructed by the surgeon’s head. There is no need to use a surgical light in laparoscopic surgery, and thus, the warm air can fall on the patient’s body directly.
Laparoscopic surgery has some demerits related to maintaining adequate patient body temperatures, including the patient’s position for the surgery, the area of skin surface able to be warmed and the use of cold carbon dioxide gas [1, 2]. However, laparoscopic surgery has some merits for the patients such as a surgeon’s posture, the lack of the need for a surgical light and the warm airflow falling directly on the patient (when the new AC system is used). The number of laparoscopic surgeries is increasing dramatically, and the cost of the new AC system is not very high considering that it has clear benefits for both patients and surgeons and that its cost is a one-time investment at construction. Such AC systems should be introduced into all ORs used for laparoscopic surgeries.
There are several limitations to this study. The old ORs at our hospital were closed for reconstruction just after the completion of the new ORs, and thus, a randomized study could not be performed. The anesthesiologists and staff nurses in the new ORs were not exactly the same as those in the old ORs, even for the second part of the study. However, the occurrence of hypothermic states was greatly reduced in the new ORs. The usefulness of the new AC system was verified in this study.
References
Huntington TR, LeMaster CB (1997) Laparoscopic hypothermia: heat loss from insufflation gas flow. Surg Laparosc Endosc 7:153–155
Kaynan AM, Winfield HN (2002) Thermostasis during laparoscopic urologic surgery. J Endourol 16:465–470
Nduka CC, Puttick M, Coates P et al (2002) Intraperitoneal hypothermia during surgery enhances postoperative tumor growth. Surg Endosc 16:611–615
Campbell G, Alderson P, Smith AF et al (2015) Warming of intravenous and irrigation fluids for preventing inadvertent perioperative hypothermia. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD009891.pub2
Sellden E, Lindahl SG (1999) Amino acid-induced thermogenesis reduces hypothermia during anesthesia and shortens hospital stay. Anesth Analg 89:1551–1556
Umenai T, Nakajima Y, Sessler DI et al (2006) Perioperative amino acid infusion improves recovery and shortens the duration of hospitalization after off-pump coronary artery bypass grafting. Anesth Analg 103:1386–1393
Fujita T, Okada N, Kanamori J et al (2017) Thermogenesis induced by amino acid administration prevents intraoperative hypothermia and reduces postoperative infectious complications after thoracoscopic esophagectomy. Dis Esophagus 30:1–7
Bashirov E, Cetiner S, Emre M et al (2007) A randomized controlled study evaluating the effects of the temperature of insufflated CO2 on core body temperature and blood gases (an experimental study). Surg Endosc 21:1820–1825
Dean M, Ramsay R, Heriot A et al (2017) Warmed, humidified CO2 insufflation benefits intraoperative core temperature during laparoscopic surgery: a meta-analysis. Asian J Endosc Surg 10:128–136
Miller-Leiden S, Lobascio C, Nazaroff WW et al (1996) Effectiveness of in-room air filtration and dilution ventilation for tuberculosis infection control. J Air Waste Manag Assoc (1995) 46:869–882
Leslie K, Sessler DI, Bjorksten AR et al (1995) Mild hypothermia alters propofol pharmacokinetics and increases the duration of action of atracurium. Anesth Analg 80:1007–1014
Hannan EL, Samadashvili Z, Wechsler A et al (2010) The relationship between perioperative temperature and adverse outcomes after off-pump coronary artery bypass graft surgery. J Thorac Cardiovasc Surg 139:1568–1575
Schmied H, Kurz A, Sessler DI et al (1996) Mild hypothermia increases blood loss and transfusion requirements during total hip arthroplasty. Lancet 347:289–292
Winkler M, Akca O, Birkenberg B et al (2000) Aggressive warming reduces blood loss during hip arthroplasty. Anesth Analg 91:978–984
Beilin B, Shavit Y, Razumovsky J et al (1998) Effects of mild perioperative hypothermia on cellular immune responses. Anesthesiology 89:1133–1140
Ben-Eliyahu S, Shakhar G, Rosenne E et al (1999) Hypothermia in barbiturate-anesthetized rats suppresses natural killer cell activity and compromises resistance to tumor metastasis: a role for adrenergic mechanisms. Anesthesiology 91:732–740
Kurz A, Sessler DI, Lenhardt R (1996) Perioperative normothermia to reduce the incidence of surgical-wound infection and shorten hospitalization. Study of wound infection and temperature group. N Engl J Med 334:1209–1215
Kurz A (2008) Thermal care in the perioperative period. Best Pract Res Clin Anaesthesiol 22:39–62
Berrios-Torres SI, Umscheid CA, Bratzler DW et al (2017) Centers for disease control and prevention guideline for the prevention of surgical site infection, 2017. JAMA Surg 152:784–791
Wong PF, Kumar S, Bohra A et al (2007) Randomized clinical trial of perioperative systemic warming in major elective abdominal surgery. Br J Surg 94:421–426
Erdling A, Johansson A (2015) Core temperature—the intraoperative difference between esophageal versus nasopharyngeal temperatures and the impact of prewarming, age, and weight: a randomized clinical trial. AANA J 83:99–105
Brandes IF, Muller C, Perl T et al (2013) Efficacy of a novel warming blanket: prospective randomized trial. Der Anaesthesist 62:137–142
Madrid E, Urrutia G, Roque i Figuls M et al (2016) Active body surface warming systems for preventing complications caused by inadvertent perioperative hypothermia in adults. Cochrane Database Syst Rev 4:Cd009016
Su SF, Nieh HC (2018) Efficacy of forced-air warming for preventing perioperative hypothermia and related complications in patients undergoing laparoscopic surgery: a randomized controlled trial. Int J Nurs Pract 24:e12660
Berg RJ, Inaba K, Sullivan M et al (2015) The impact of heat stress on operative performance and cognitive function during simulated laparoscopic operative tasks. Surgery 157:87–95
National Collaborating Centre for N, Supportive C, National Institute for Health and Clinical Excellence: Guidance (2008). In: The management of inadvertent perioperative hypothermia in adults. Royal College of Nursing (UK) National Collaborating Centre for Nursing and Supportive Care, London
Usuki H, Koizumi M (2017) The body temperature in laparoscopic surgery and the countermeasure in the construction of operative center. Jpn J Oper Med 38:100-106
Usuki H, Asano E, Oshima M et al (2018) Operating room: which temperature is comfortable for both patients and surgeons? Thermol Int 28:3
Acknowledgements
This work was supported by the JSPS KAKENHI, Grant No. 15K06323.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflicts of interests or disclosures
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Usuki, H., Kitamura, H., Ando, Y. et al. New Concept Air Conditioning System for the Operating Room to Minimize Patient Cooling and Surgeon Heating: A Historical Control Cohort Study. World J Surg 44, 45–52 (2020). https://doi.org/10.1007/s00268-019-05203-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-019-05203-8