Abstract
Background
Catecholamine excess in patients with pheochromocytomas or paragangliomas (PPGLs) can lead to hypertension, diabetes and hyperlipidemia. The aim was to investigate the prevalence of hyperlipidemia and the effect of surgical resection.
Methods
One hundred and thirty-two patients with PPGLs underwent an operation at the National Institutes of Health from 2009 to 2016, of which 54 patients met the inclusion criteria. Clinical demographics, BMI, genetic mutations, tumor size, perioperative catecholamine levels and perioperative lipid panels were retrospectively reviewed. Spearman correlation between catecholamines and lipid levels was evaluated. Paired Wilcoxon and paired t test were used to analyze differences in pre- and postoperative lipid levels.
Results
Preoperatively, 51 patients (94.4%) had elevated catecholamines, thirteen (24.1%) had elevated total cholesterol (TC) (>200 mg/dL), nine (16.6%) had elevated LDL (>130 mg/dL) and ten (18.5%) had elevated triglycerides (>150 mg/dL). Serum and urinary metanephrine levels were positively associated with TC (r = 0.2792, p = 0.0372 and r = 0.4146, p = 0.0031, respectively) and LDL levels (r = 0.2977, p = 0.0259 and r = 0.4434, p = 0.0014, respectively). Mean TC decreased from 176.4 to 166.3 mg/dL (p = 0.0064) and mean HDL decreased from 56.7 to 53.2 mg/dL (p = 0.0253) after PPGL resection (median 3.1 months (range 1.3–50.2) between lipid panels). Most patients with elevated TC (76.9%) had improvement with mean TC decreasing from 225 to 200.2 mg/dL (p = 0.0230). Of patients with elevated LDL, 66.7% had improvement with mean LDL decreasing from 149 to 131.1 mg/dL (p = 0.0313).
Conclusions
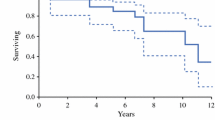
The prevalence of hyperlipidemia in patients with PPGLs is 46%. Future prospective studies are needed to determine whether surgical resection improves TC and/or LDL levels.


Similar content being viewed by others
References
Kiernan CM, Solorzano CC (2016) Pheochromocytoma and paraganglioma: diagnosis, genetics, and treatment. Surg Oncol Clin N Am 25(1):119–138. https://doi.org/10.1016/j.soc.2015.08.006
Benn DE, Robinson BG (2006) Genetic basis of phaeochromocytoma and paraganglioma. Best Pract Res Clin Endocrinol Metab 20(3):435–450. https://doi.org/10.1016/j.beem.2006.07.005
Fishbein L, Merrill S, Fraker DL, Cohen DL, Nathanson KL (2013) Inherited mutations in pheochromocytoma and paraganglioma: why all patients should be offered genetic testing. Ann Surg Oncol 20(5):1444–1450. https://doi.org/10.1245/s10434-013-2942-5
Gimenez-Roqueplo AP et al (2003) Mutations in the SDHB gene are associated with extra-adrenal and/or malignant phaeochromocytomas. Cancer Res 63(17):5615–5621
Pacak K (2007) Preoperative management of the pheochromocytoma patient. J Clin Endocrinol Metab 92(11):4069–4079. https://doi.org/10.1210/jc.2007-1720
Chen H et al (2010) The North American Neuroendocrine Tumor Society consensus guideline for the diagnosis and management of neuroendocrine tumors: pheochromocytoma, paraganglioma, and medullary thyroid cancer. Pancreas 39(6):775–783. https://doi.org/10.1097/MPA.0b013e3181ebb4f0
Manger WM (2006) An overview of pheochromocytoma: history, current concepts, vagaries, and diagnostic challenges. Ann N Y Acad Sci 1073:1–20. https://doi.org/10.1196/annals.1353.001
Bernini G et al (2006) Carotid vascular remodeling in patients with pheochromocytoma. J Clin Endocrinol Metab 91(5):1754–1760. https://doi.org/10.1210/jc.2005-2199
Zhang R, Gupta D, Albert SG (2017) Pheochromocytoma as a reversible cause of cardiomyopathy: analysis and review of the literature. Int J Cardiol 249:319–323. https://doi.org/10.1016/j.ijcard.2017.07.014
Beninato T et al (2017) Resection of pheochromocytoma improves diabetes mellitus in the majority of patients. Ann Surg Oncol 24(5):1208–1213. https://doi.org/10.1245/s10434-016-5701-6
Timmers HJ et al (2008) Metastases but not cardiovascular mortality reduces life expectancy following surgical resection of apparently benign pheochromocytoma. Endocr Relat Cancer 15(4):1127–1133. https://doi.org/10.1677/ERC-08-0049
Colwell JA (1969) Inhibition of insulin secretion by catecholamines in pheochromocytoma. Ann Intern Med 71(2):251–256
Okamura T et al (2015) Changes in visceral and subcutaneous fat mass in patients with pheochromocytoma. Metabolism 64(6):706–712. https://doi.org/10.1016/j.metabol.2015.03.004
Khorram-Manesh A et al (2005) Long-term outcome of a large series of patients surgically treated for pheochromocytoma. J Intern Med 258(1):55–66. https://doi.org/10.1111/j.1365-2796.2005.01504.x
Berent H et al (1987) Lipids and beta-thromboglobulin in patients with pheochromocytoma. J Clin Hypertens 3(4):389–396
Maduka IC, Neboh EE, Ufelle SA (2015) The relationship between serum cortisol, adrenaline, blood glucose and lipid profile of undergraduate students under examination stress. Afr Health Sci 15(1):131–136. https://doi.org/10.4314/ahs.v15i1.18
American Heart Association, Cholesterol medications, https://www.heart.org/en/health-topics/cholesterol/prevention-and-treatment-of-high-cholesterol-hyperlipidemia/cholesterol-medications. 10 Nov 2018
Chaudhary R, Garg J, Shah N, Sumner A (2017) PCSK9 inhibitors: a new era of lipid lowering therapy. World J Cardiol 9(2):76–91. https://doi.org/10.4330/wjc.v9.i2.76
National Heart Lung and Blood Institute. High cholesterol what you need to know, https://www.nhlbi.nih.gov/files/docs/public/heart/wyntk.pdf. June 2005
Kopin L, Lowenstein C (2017) Dyslipidemia. Ann Intern Med. 167(11):ITC81–ITC96. https://doi.org/10.7326/aitc201712050
Centers for Disease Control and Prevention. Total and high-density lipoprotein cholesterol in adults: United States, 2015–2016, https://www.cdc.gov/nchs/products/databriefs/db290.htm. 26 Oct 2017
O’Meara JG et al (2004) Ethnic and sex differences in the prevalence, treatment, and control of dyslipidemia among hypertensive adults in the GENOA study. Arch Intern Med 164(12):1313–1318. https://doi.org/10.1001/archinte.164.12.1313
Goff DC Jr et al (2006) Dyslipidemia prevalence, treatment, and control in the Multi-Ethnic Study of Atherosclerosis (MESA): gender, ethnicity, and coronary artery calcium. Circulation 113(5):647–656. https://doi.org/10.1161/CIRCULATIONAHA.105.552737
La Batide-Alanore A, Chatellier G, Plouin PF (2003) Diabetes as a marker of pheochromocytoma in hypertensive patients. J Hypertens 21(9):1703–1707. https://doi.org/10.1097/01.hjh.0000084729.53355.ce
Bai S et al (2019) Risk factors for postoperative cardiovascular morbidity after pheochromocytoma surgery: a large single center retrospective analysis. Endocr J 66(2):165–173. https://doi.org/10.1507/endocrj.EJ18-0402
Funding
This research was supported by the Intramural Research Program of NIH.
Author information
Authors and Affiliations
Contributions
DP and MLG conceptualized and designed the study. KP, NN, EK and DP identified, consented and treated the patients, including operative and perioperative care and acquisition of patient data. MLG, PM, SMR, SG, AC and DP assembled the patient data. MLG, PM, SMR and DP analyzed and interpreted the patient data. MLG, PM, SMR, SG, AC and DP contributed to writing the manuscript. All co-authors participated in revising the text and all co-authors reviewed and gave approval for the current form of the manuscript to be submitted.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Good, M.L., Malekzadeh, P., Ruff, S.M. et al. Surgical Resection of Pheochromocytomas and Paragangliomas is Associated with Lower Cholesterol Levels. World J Surg 44, 552–560 (2020). https://doi.org/10.1007/s00268-019-05175-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-019-05175-9