Abstract
Background
Needle tract implantation (NTI) can occur after thyroid fine-needle aspiration cytology (FNAC). To date, no studies enrolling a large number of patients and studying the cumulative incidence (CI) of NTI have been published. This study analyzed the clinicopathological features of NTI and calculated the CI.
Methods
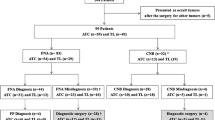
A total of 11,745 patients who underwent first FNAC, resection for thyroid carcinomas and related lymph node metastases, and postoperative ultrasonography in Kuma Hospital between 2006 and 2017 were evaluated. NTI was defined as macroscopically visible and/or sonographically detected recurrent tumors at the sites of the previous aspiration. Lymphovascular invasion and/or nodal metastasis were excluded.
Results
We found 22 NTI-THY (originated from aspiration of thyroid tumors) and 8 NTI-LN (originating from lymph nodes) cases with CI of 0.15% and 0.37%, and 0.37% and 0.58% at 5 and 10 years after FNAC, respectively. A large percentage (53%) of cases are presented as more aggressive histologic subtypes than their original tumors. Of these NTI patients, 4 (12.1%) died of disease and 10 (33.3%) developed distant metastases but remained alive with stable disease, three (9.1%) developed local recurrences, and the remaining 15 (10%) were free of recurrence.
Conclusions
We demonstrated for the first time the CI and detailed clinicopathological features of thyroid NTI associated with possible histological transformation. Despite the low CI, the risk of death and distant metastases increase manifold in NTI patients than that in patients without recurrence. Therefore, NTI could be an important prognostic variable and impact patient survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thyroid carcinoma has various histological types such as papillary (PTC), follicular (FTC), poorly differentiated (PDTC), anaplastic (ATC), and medullary thyroid carcinomas (MTC) having different clinicopathological features and prognoses. For the preoperative diagnosis of histological types and proper management of thyroid carcinoma, fine-needle aspiration cytology (FNAC) is mandatory. This technique is generally safe, but some complications might occasionally occur, and needle tract implantation (NTI) is one of them [1,2,3]. NTI occurs when cancer cells aspirated by the needle are disseminated in the tissues along the needle tracts. To date, several studies have been published regarding this issue [4,5,6,7,8,9,10,11,12,13,14]. Ito et al. demonstrated that the incidence of NTI was 0.14% in PTC patients who underwent FNAC. They also showed that NTI was likely to occur within a short interval after FNAC in PTCs with aggressive characteristics, such as having poorly differentiated lesions and extrathyroid extension. Salvage surgery is adequate for the local control of NTI lesions. However, a previous study showed that 45% of PTC patients with NTI also showed distant recurrence simultaneously or intertemporally [5], indicating that patients showing NTI should undergo careful follow-up.
To the best of our knowledge, no studies enrolling a large number of patients who underwent FNAC for various histological types of thyroid carcinoma and studying the cumulative incidence (CI) of the occurrence of NTI have been published. Thus, in this study, we aimed to analyze the clinicopathological features of patients with thyroid carcinomas who developed NTI and calculated the CI of NTI using the Kaplan–Meier method.
Material and methods
Between 2006 and 2017, a total of 13,176 patients with thyroid cancer underwent initial surgery at Kuma Hospital, Kobe, Japan. Written informed consent for FNAC and surgery was obtained from the patients before the procedures. The inclusion criteria were as follows: initial FNAC for primary thyroid cancer and metastatic lymph nodes before surgery within the same period, diagnosis confirmed by histology, and followed by postoperative ultrasonography at Kuma Hospital. We enrolled 11,745 patients who met the inclusion criteria. They consisted of 11,076 PTC (93.7%), 418 FTC (3.5%), 70 MTC (0.6%), 121 PDTC (1%), and 60 ATC (0.5%). NTI cases were defined following strict clinicopathological criteria and the anatomical relationship between the lesion of the recurrent tumor and the site of fine-needle aspiration as patients with macroscopically visible and/or sonographically detected recurrent tumors at the sites of the previous aspiration. Cases with tumor cells within lymphoid or vascular tissue consistent with lymphovascular invasion and/or nodal metastasis, cases with findings suggestive of growth of residual tumor following incomplete resection, and cases with findings suggestive of intraoperative tumor disruption and spillage at the initial operation were excluded. Finally, we found 30 cases of NTI that fulfilled the above inclusion criteria.
All pathology specimens of both resected primary tumors and their corresponding NTIs were reviewed based on World Health Organization criteria for histological typing of endocrine tumors [15]. In this study, medical records were retrieved from electronic patient records. Available records were reviewed for clinical presentation, treatment, and clinical outcome. All 30 NTI patients were followed until their death or through February 2019, with a median length of follow-up after NTI resection of 5.50 (0.08–12.92) years.
To calculate the CI of NTI following FNAC, we selected 11,745 patients for calculation of CI of NTI-THY and 2191 patients for calculation of NTI-LN.
Statistics
We examined the association between clinical and pathological variables. Categorical variables were compared by Fisher’s exact test and nonparametric test by Mann–Whitney U test. The Kaplan–Meier method was used to calculate the CI of NTI following FNAC. Statistical analysis was performed using STATFLEX version 6 (Artech Co., Ltd., Osaka, Japan) and the Mann–Whitney test calculator (https://astatsa.com/WilcoxonTest/). P values < 0.05 were considered statistically significant.
Results
Table 1 shows the clinical features of patients who developed NTI. This study included 22 NTI cases that originated from the aspiration of thyroid tumors (NTI-THY) and eight NTI cases that originated from the aspiration of metastatic lymph nodes (NTI-LN). NTI occurred in 25 female and 5 male patients (20 female and 2 male patients with NTI-THY and 5 female and 3 male patients with NTI-LN). Patients’ age at the first presentation of NTI ranged from 43 to 91 years (43 to 91 years with median of 70.6 years for NTI-THY and 58 to 74 years with median of 64.8 years for NTI-LN). The interval between the initial aspiration and appearance of NTI ranged between 0.5 and 9.5 years (median 5 years for NTI-THY and 2.5 years for NTI-LN). Salvage surgery was performed with complete removal of NTI, and no local recurrence for all NTI cases was noted at follow-up. Long-term follow-up of the clinical outcome showed that of the 22 patients with NTI-THY, 4 (18.2%) died of the disease and 9 (40.9%) had distant metastases. Of the eight patients with NTI-LN, 1 (12.5%) developed distant metastasis, and no death related to disease was noted. The 10 patients who developed distant metastases (lung n = 8; bone and lung n = 2) remained alive with stable disease at the last follow-up after radioactive iodine treatment or external beam radiotherapy. Three patients developed local structural recurrence related to primary tumor (NTI-THY n = 2; NTI-LN = 1). The remaining 13 patients were alive and free of structural recurrence at the last follow-up (NTI-THY n = 7; NTI-LN = 6). Statistically significant differences were identified between the two NTI groups with respect to patients’ age at the first presentation (p = 0.027080), but no statistically significant differences in other parameters, such as the number of cases, sex, interval between the initial aspiration and the appearance of NTI, and clinical outcomes were noted.
The CIs of NTI-THY were 0.37% and 0.58% at 5 and 10 years, respectively (Fig. 1a). The CIs of NTI-LN were 0.61% and 0.94% at 5 and 10 years, respectively (Fig. 1b). In the NTI-THY group, the CIs of PTC, FTC, and ATC were 0.1% and 0.3%, 1.32% and 2.33%, and 3.03% and 3.03% at 5 and 10 years after FNAC, respectively (Fig. 1c). In the NTI-LN group, the CIs of PTC and PDTC were 0. 25% and 0.47%, and 12.7% and 12.7% at 5 and 10 years after FNAC, respectively (Fig. 1d). The CIs of PDTC in the NTI-THY group and FTC and ATC in the NTI-LN group were not calculated because no such cases were identified.
Cumulative incidence of the development of needle tract implantation following fine-needle aspiration. a On thyroid cancer, b on lymph node metastatic lesions (NTI-LN), c on papillary thyroid carcinoma (PTC), follicular thyroid carcinoma (FTC), and anaplastic thyroid carcinoma (ATC) in the thyroid group (NTI-THY), and d on papillary thyroid carcinoma and poorly differentiated thyroid carcinoma in the lymph node metastatic lesion group (NTI-LN)
Table 2 shows the histopathological features of 22 NTI-THY cases. The incidences were as follows: PTC at 0.1% ((n = 16), FTC at 1.2% (n = 5), PDTC at 0% (n = 0), ATC at 1.6% (n = 1), and MTC at 0% (n = 0). Moreover, 13 (59.1%) NTI cases formed a single nodule (Fig. 2a), while the remaining 9 (40.9%) NTI cases formed multiple rounded nodules (Fig. 2b). With regard to the location of lesions, 30 of all 40 lesions (75%) were located in subcutaneous tissues, while 5 (12.5%) were located in the muscle layer or deeper structures and 5 (12.5%) were located in the dermis.
Figure 3 indicates the histological evolution implicated in NTI. Among the initial 18 NTI cases of conventional PTC in the resected specimen of the aspiration sites (Fig. 4a), nine NTI cases with conventional PTC with focal tall cell component (<30%) absent at the aspiration sites, one case of hobnail variant (PTC with more than 30% of hobnail pattern) (Fig. 4b), two cases of follicular variant of PTC, and two cases of PDTC were identified. Among the three cases of tall cell variant in the resected specimen of the aspiration sites, one case of NTI showed hobnail variant PTC and one case showed ATC. The histology was identical between resected specimens from the aspiration sites and NTI in the remaining 14 cases.
Discussion
The current understanding and knowledge about thyroid NTI are extremely poor and primarily based on case reports and retrospective reviews of literature without a systematic and comprehensive evaluation so far [3,4,5,6,7,8,9,10,11,12,13]. To the best of our knowledge, this study is the first to enroll a large number of patients with thyroid carcinomas of different histological types who developed NTI following FNAC for primary thyroid cancer and related metastatic lymph nodes, to calculate the CI, and to identify the clinicopathological features of NTI with long-term follow-up and clinical outcomes. NTI is a rare occurrence and often develops slowly. In fact, most surgeons and general pathologists are unaware of NTI, and it may then be confused with skin metastasis of thyroid cancer and make the true incidence of NTI unclear. The recurrence in the neck of thyroid cancer may occur as lymph node metastasis, growth of residual tumor following incomplete resection, spillage of cancer cells during surgery, or needle tract implantation. The spatial locations of the present cases were not consistent with nodal metastasis or growth of residual tumors. Regarding the possibility of spillage of cancer cells, our standard surgical procedures were en bloc resection of the thyroid cancer without exposing the surface of the tumor of thyroid cancer. The surface of the thyroid cancer may be exposed only if cancer invades the recurrent laryngeal nerve, trachea, and/or larynx. Our present cases were not such cases. In addition, in the cases of intraoperative spillage, the recurrent lesions should likely be widely dispersed, which was different from our study cohort. All our cases reported in the present paper occurred on the previous insertion site of fine-needle aspiration or the line of needle tract.
The CIs of NTI-THY and NTI-LN were 0.15% and 0.37% and 0.37% and 0.58% at 5 and 10 years after FNAC, respectively. Our study suggested that the risk for the development of NTI is low but not completely nonexistent. With regard to the CI of the different histological types, we observed that FTC and ATC had a higher CI (1.32% and 2.33% and 3.03% and 3.03% at 5 and 10 years after FNAC, respectively) compared to that of PTC (0.1% and 0.3% at 5 and 10 years after FNAC, respectively) in NTI-THY. Furthermore, PDTC had a higher CI (12.7% and 12.7% at 5 and 10 years after FNAC, respectively) compared to that of PTC (0.25% and 0.47 at 5 and 10 years after FNAC, respectively) in NTI-LN. Generally, we found higher CIs in NTI-LN lesions than NTI-THY lesions and associated with more aggressive histological types.
In this study, although we did not observe NTI in our MTC cohort, NTI from MTC has been observed in our file of pathology (our unpublished observation). We demonstrated that NTI can develop in any type of thyroid carcinoma. Following the histological evolution implicated in NTI, although the histology was identical between the resected specimen of the aspirated site and NTI in 14 (46.7%) NTI cases, the occurrence of the more aggressive component (i.e., tall cell or hobnail component) in NTI, but absence at initial aspirated sites, and histological transformation to a more aggressive histological type were identified in the remaining 16 (53.3%) cases. Therefore, the microscopic findings of NTI may show a more aggressive form than its corresponding primary aspiration site. The mechanism of the histological transformation in NTI is still unknown, and to the best of our knowledge, this paper is the first comprehensive study to describe the histological transformation in NTI after FNAC of thyroid tumor and related metastatic LN. Our proposed hypothesis is that histological transformation may occur spontaneously or be induced by the tumor–host microenvironment interaction after implantation of tumor cells in the dermis, subcutaneous adipose tissue, muscle, or deeper structures. Another possible explanation is that the tumor cells from a more aggressive subpopulation may have the potential and higher possibility to survive along the needle tract and lead to NTI of a histological type different from that of the aspirated sites. To further explore this event, we calculated the incidence of NTI-THY and NTI-LN from the corresponding resected specimens of the initial aspirated site. The incidence of NTI-LN was higher than that of NTI-THY (0.37% and 0.15%, respectively), although the difference was not statistically significant. Although PTC remains the most common histological type for NTI-THY, FTC and ATC occur much more frequently than PTC in NTI-THY (1.2%, 1.7%, 0.1%, respectively). The incidence of NTI-LN for other histological types, except for PTC, was not calculated in the same way because of the overwhelming predominance of PTC. Overall, NTI-THYs appear more frequently in more aggressive histological types. Therefore, for the development of NTI and possible histological transformation in NTI, the difference in the incidence of histological types may depend on tumor aggressiveness.
In all our NTI cases, salvage surgical resection was successful in removing NTI lesions. Neither further local seeding nor death directly related to NTI was identified during the follow-up period. These results suggested that a surgical approach is effective in removing NTI. However, notably, the high incidence of cancer-related death and distant metastasis rate in our study group are comparable to the result of a previous series for PTC in NTI-THY from our institution (distant metastasis in 33.3% vs. 45% and cancer-related death in 12.1% vs. 10% of NTI patients, respectively) [5]. In contrast, most differentiated thyroid cancers follow generally an indolent course. Ito et al. reported that 2% of PTC cases metastasize to distant organs, such as the lungs, bone, and brain [16]. After a long follow-up period, only 2% of the patients died due to PTC. In this study, there were 4 (12.1%) cancer-related deaths, and 10 (33.3%) patients developed distant metastases during the follow-up period of 13 years. Therefore, despite the low CI, the risk of death and distant metastases increases in NTI patients compared to that in patients with no recurrence as previously reported from our institution [16]. Postoperative close follow-up and adjuvant therapy, if needed for NTI of aggressive histological type, could be useful to improve survival and disease control.
The principal strength of the present study is the enrollment of a large number of patients with NTI-THY and NTI-LN of different histological types with long-term follow-up and CI. Our findings will provide strong implications and contribute to the field at large particularly for clinical management of NTI. The limitations of the present study include that it is a retrospective study performed at a single institution specialized in thyroid care, which means that the possibility of generalizing the results might be low. Despite these limitations, the study in a single institution could minimize the possibility of inconsistency of clinical data, pathological diagnosis, management policy. Further multicenter, prospective studies are required to clarify the clinicopathological features of NTI.
In conclusion, this study demonstrated for the first time the CI and detailed clinicopathological features of thyroid NTI. Despite the low CI, the risk of death, and that distant metastases increase manifold in NTI patients compared to that in patients without recurrence. NTI in a previous aspiration site may transform into a more aggressive histological variant. NTI could be an important prognostic variable and impact the patient survival.
References
Polyzos SA, Anastasilakis AD (2009) Clinical complications following thyroid fine-needle biopsy: a systematic review. Clin Endocrinol (Oxford) 71:157–165
Tyagi R, Dey P (2014) Needle tract seeding: an avoidable complication. Diagn Cytopathol 42:636–640
Chang S, Kim SH, Lim HK et al (2005) Needle tract implantation after sonographically guided percutaneous biopsy of hepatocellular carcinoma: evaluation of doubling time, frequency, and features on CT. AJR Am J Roentgenol 185:400–405
Ito Y, Tomoda C, Uruno T et al (2005) Needle tract implantation of papillary thyroid carcinoma after fine-needle aspiration biopsy. World J Surg 29:1544–1549https://doi.org/10.1007/s00268-005-0086-x
Ito Y, Hirokawa M, Higashiyama T et al (2012) Clinical significance and prognostic impact of subcutaneous or intrastrap muscular recurrence of papillary thyroid carcinoma. J Thyroid Res 2012:819797
Mighell AJ, High AS (1998) Histological identification of carcinoma in 21 gauge needle tracks after fine needle aspiration biopsy of head and neck carcinoma. J Clin Pathol 51:241–243
Tamiolakis D, Antoniou C, Venizelos J et al (2006) Papillary thyroid carcinoma metastasis most probably due to fine needle aspiration biopsy. A case report. Acta Dermatovenerol Alp Pannonica Adriat 15:169–172
Hales MS, Hsu FS (1990) Needle tract implantation of papillary carcinoma of the thyroid following aspiration biopsy. Acta Cytol 34:801–804
Abelardo E, Jaramillo M, Sheffield E et al (2007) Anaplastic thyroid carcinoma implantation after fine needle aspiration cytology. J Laryngol Otol 121:268–270
Ito Y, Asahi S, Matsuzuka F et al (2006) Needle tract implantation of follicular neoplasm after fine-needle aspiration biopsy: report of a case. Thyroid 16:1059–1062
Polyzos SA, Anastasilakis AD (2010) A systematic review of cases reporting needle tract seeding following thyroid fine needle biopsy. World J Surg 34:844–851https://doi.org/10.1007/s00268-009-0362-2
Basu A, Sistla SC, Siddaraju N et al (2008) Needle tract sinus following aspiration biopsy of papillary thyroid carcinoma: a case report. Acta Cytol 52:211–214
Karwowski JK, Nowels KW, McDougall IR et al (2002) Needle track seeding of papillary thyroid carcinoma from fine needle aspiration biopsy. A case report Acta Cytol 46:591–595
Siddiqi MA, Kim HS, Jede F et al (2017) Association of core needle biopsy tract: resection with local recurrence in extremity soft tissue sarcoma. Skeletal Radiol 46:507–512
DeLellis RA, Lloyd RV, Heitz H et al (2003) WHO classification of tumours of endocrine organs. IARC Press, Lyon, pp 49–123
Ito Y, Miyauchi A, Kihara M et al (2018) Overall survival of papillary thyroid carcinoma patients: a single-institution long-term follow-up of 5897 patients. World J Surg 42:615–622https://doi.org/10.1007/s00268-018-4479-z
Acknowledgements
The authors wish to acknowledge Ms. Ayana Suzuki, Ms. Risa Kanematsu, and Ms. Izumi Otsuka for their invaluable assistance in retrieving the records and materials used in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Hayashi, T., Hirokawa, M., Higuchi, M. et al. Needle Tract Implantation Following Fine-Needle Aspiration of Thyroid Cancer. World J Surg 44, 378–384 (2020). https://doi.org/10.1007/s00268-019-05161-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-019-05161-1