Abstract
Background
Thyroidectomy transoral endoscopic thyroidectomy vestibular approach (TOETVA) is a safe and cosmetically appealing alternative for well-selected patients undergoing thyroidectomy. However, during TOETVA, placement of the two lateral trocars and/or manipulation of the surgical instruments through the trocars may potentially injure and/or compress the mental nerve (MN) because the actual location of the nerve foramen may vary among individuals. The MN injury rate was reported to be as high as 75% in the initial period of robotic-assisted TOETVA. To reduce the potential risk of MN injury, we implemented a three-dimensional printing technology to develop a safety device for TOETVA.
Methods
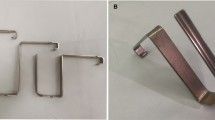
The patient-specific safety device (PSSD) was a brace with an exact fit to the lower teeth and two safety markers on each side to indicate the location of the mental foramen. For patient in whom the brace would not be applicable, a 3D mandibular model was printed as a PSSD instead. We analyzed 66 patients undergoing TOETVA at our institution from March 2017 to March 2019. The preoperative details and complication profiles were also analyzed.
Results
With incorporation of the PSSD into our TOETVA procedure, there have been no cases of MN injury.
Conclusions
Our own TOETVA series has demonstrated that the implementation of the PSSD has been successful in preoperatively identifying and preventing the potential risk of MN injury. Although the additional requirements of preoperative CT and time for fabricating the device impose limitations, the influence of the PSSD in TOETVA is positive.




Similar content being viewed by others
References
Anuwong A (2016) Transoral endoscopic thyroidectomy vestibular approach: a series of the first 60 human cases. World J Surg 40(3):491–497. https://doi.org/10.1007/s00268-015-3320-1
Kim HY et al (2018) Transoral robotic thyroidectomy: lessons learned from an initial consecutive series of 24 patients. Surg Endosc 32(2):688–694
Dionigi G et al (2017) Transoral endoscopic thyroidectomy: preliminary experience in Italy. Updates Surg 69(2):225–234
Udelsman R et al (2016) Trans-oral vestibular endocrine surgery: a new technique in the United States. Ann Surg 264(6):e13–e16
Shan LQ, Liu JN (2018) A systemic review of transoral thyroidectomy. Surg Laparosc Endosc Percutaneous Tech 28(3):135–138
Anuwong A et al (2018) Safety and outcomes of the transoral endoscopic thyroidectomy vestibular approach. JAMA Surg 153(1):21–27
Sasanakietkul T, Jitpratoom P, Anuwong A (2017) Transoral endoscopic parathyroidectomy vestibular approach: a novel scarless parathyroid surgery. Surg Endosc Other Interv Tech 31(9):3755–3763
Russell JO et al (2018) Transoral thyroid and parathyroid surgery vestibular approach: a framework for assessment and safe exploration. Thyroid 28(7):825–829
Richmon JD et al (2011) Transoral robotic-assisted thyroidectomy with central neck dissection: preclinical cadaver feasibility study and proposed surgical technique. J Robot Surg 5(4):279–282
Greenstein G, Tarnow D (2006) The mental foramen and nerve: clinical and anatomical factors related to dental implant placement: a literature review. J Periodontol 77(12):1933–1943
Kuzmanovic DV et al (2003) Anterior loop of the mental nerve: a morphological and radiographic study. Clin Oral Implants Res 14(4):464–471
Kurzmann C et al (2017) Evaluation of resins for stereolithographic 3D-printed surgical guides: the response of L929 cells and human gingival fibroblasts. Biomed Res Int 4057612(10):22
Yang JC et al (2018) Clinical experience using a 3D-printed patient-specific instrument for medial opening wedge high tibial osteotomy. Biomed Res Int 8:9246529
Kakkar A et al (2016) Primary bone tumors of the skull: spectrum of 125 cases, with review of literature. J Neurol Surg Part B Skull Base 77(4):319–325
Young CC et al (2018) Rapid intraoperative in situ synthetic cranioplasty. World Neurosurg 112:161–165
Mikolajewska E et al (2014) 3D printing technologies in rehabilitation engineering. J Health Sci 4(12):78–83
Lin HH, Lonic D, Lo LJ (2018) 3D printing in orthognathic surgery—a literature review. J Formos Med Assoc 2(17):30413–30418
Wu PK et al (2018) Printing a 3-dimensional, patient-specific splint for wound immobilization: a case report. Ostomy Wound Manage 64(7):28–33
Baba M et al (2017) Development of a tailored thyroid gland phantom for fine-needle aspiration cytology by three-dimensional printing. J Surg Educ 74(6):1039–1046
Beaumont T et al (2017) Development and test of sets of 3D printed age-specific thyroid phantoms for (131)I measurements. Phys Med Biol 62(12):4673–4693
Harris AD et al (2006) The use and interpretation of quasi-experimental studies in medical informatics. J Am Med Inform Assoc 13(1):16–23
Acknowledgements
This work was supported in part by a Taipei Veterans General Hospital Research (V106 E-003-1, V107 D39-001-MY2-1, V107C-198, V108C-180) and the Ministry of Science and Technology (MOST 107-2410-H-075-001), Taiwan.
Funding
NA.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors certify that they have no affiliations with or involvement in any organization or entity with any financial interests (such as honoraria, educational grants, participation in speakers’ bureaus, memberships, employment, consultancies, stock ownership, or other equity interests, and expert testimony or patent-licensing arrangements) or nonfinancial interests (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Ethical standards
The study was approved by the Institutional Review Board of the Taipei Veterans General Hospital (VGHIRB No: 2016–08-023CC).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yeh, YT., Chen, JY., Kuo, PC. et al. Printing a Three-Dimensional Patient-Specific Safety Device for Reducing the Potential Risk of Mental Nerve Injury During Transoral Thyroidectomy. World J Surg 44, 371–377 (2020). https://doi.org/10.1007/s00268-019-05155-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-019-05155-z