Abstract
Background
The aim was to evaluate the prognoses and clinicopathological characteristics of solitary hepatocellular carcinoma (HCC) originating from the caudate lobe (HCC-CL).
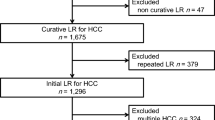
Methods
We analyzed 584 patients with a solitary tumor <10 cm from January 1990 to November 2014. Patients were classified into a caudate lobe group (CL; n = 39) and a non-caudate lobe group (NCL; n = 545). We investigated the prognoses and clinicopathological characteristics of solitary HCC-CL. We compared the surgical procedures performed in these cases.
Results
HCC-CL had a similar rate of portal venous invasion (PVI) as HCC-NCL (21% vs. 19%); however, the frequency of tumor thrombus at the first branch of the portal vein (PV) or extension to the trunk or the opposite side of the PV was significantly higher in HCC-CL (8% vs. 2%). HCC-CL had similar OS rates compared to HCC-NCL; however, HCC-CL showed significantly poorer RFS. Although there were no significant differences among the three surgical procedures, blood loss and complication rates tended to be higher in cases who underwent an isolated caudate lobectomy. Tumor size ≥5 cm, PVI, and liver fibrosis or cirrhosis (LF or LC) were independent unfavorable factors for both OS and RFS. PIVKA-II ≥120 mAU/ml was an independent unfavorable factor for RFS.
Conclusion
HCC-CL presented a poorer RFS rate. Patients with a tumor size ≥5 cm, PIVKA-II ≥120 mAU/ml, portal venous invasion, and LF or LC should be diligently followed up as these cases have a high risk of recurrence.

Similar content being viewed by others
References
Sakoda M, Ueno S, Kubo F et al (2009) Surgery for hepatocellular carcinoma located in the caudate lobe. World J Surg 33(9):1922–1926. https://doi.org/10.1007/s00268-009-0110-7
Healey JE, Schroy PC (1953) Anatomy of the biliary ducts within the human liver; analysis of the prevailing pattern of branchings and the major variations of the biliary ducts. Arch Surg 66(5):599–616
Couinaud C (1994) The paracaval segments of the liver. J Hep Bil Pancr Surg 2:145–151
Kumon M (2017) Anatomical study of the caudate lobe with special reference to portal venous and biliary branches using corrosion liver casts and clinical application. Liver Cancer 6(2):161–170
Takayasu K, Muramatsu Y, Shima Y et al (1986) Clinical and radiologic features of hepatocellular carcinoma originating in the caudate lobe. Cancer 58(7):1557–1562
Tanaka S, Shimada M, Shirabe K et al (2005) Surgical outcome of patients with hepatocellular carcinoma originating in the caudate lobe. Am J Surg 190(3):451–455
Ikegami T, Ezaki T, Ishida T et al (2004) Limited hepatic resection for hepatocellular carcinoma in the caudate lobe. World J Surg 28(7):697–701. https://doi.org/10.1007/s00268-004-7341-4
Kamiyama T, Nakanishi K, Yokoo H et al (2010) Perioperative management of hepatic resection toward zero mortality and morbidity: analysis of 793 consecutive cases in a single institution. J Am Coll Surg 211(4):443–449
Shimada S, Kamiyama T, Yokoo H et al (2017) Clinicopathological characteristics of hepatocellular carcinoma with microscopic portal venous invasion and the role of anatomical liver resection in these cases. World J Surg 41(8):2087–2094. https://doi.org/10.1007/s00268-017-3964-0
Clavien PA, Barkun J, de Oliveira ML et al (2009) The Clavien–Dindo classification of surgical complications: five-year experience. Ann Surg 250(2):187–196
Wakayama K, Kamiyama T, Shimada S et al (2017) Huge hepatocellular carcinoma greater than 10 cm in diameter worsens prognosis by causing distant recurrence after curative resection. J Surg Oncol 115(3):324–329
Hasegawa K, Kokudo N, Imamura H et al (2005) Prognostic impact of anatomic resection for hepatocellular carcinoma. Ann Surg 242(2):252–259
Sakamoto Y, Nara S, Hata S et al (2011) Prognosis of patients undergoing hepatectomy for solitary hepatocellular carcinoma originating in the caudate lobe. Surgery 150(5):959–967
Liu P, Yang JM, Niu WY et al (2010) Prognostic factors in the surgical treatment of caudate lobe hepatocellular carcinoma. World J Gastroenterol 16(9):1123–1128
Tsai TJ, Chau GY, Lui WY et al (2000) Clinical significance of microscopic tumor venous invasion in patients with resectable hepatocellular carcinoma. Surgery 127(6):603–608
Eguchi S, Takatsuki M, Hidaka M et al (2010) Predictor for histological microvascular invasion of hepatocellular carcinoma: a lesson from 229 consecutive cases of curative liver resection. World J Surg 34(5):1034–1038. https://doi.org/10.1007/s00268-010-0424-5
Shirabe K, Itoh S, Yoshizumi T et al (2007) The predictors of microvascular invasion in candidates for liver transplantation with hepatocellular carcinoma: with special reference to the serum levels of des-gamma-carboxy prothrombin. J Surg Oncol 95(3):235–240
Takayama T, Tanaka T, Higaki T et al (1994) High dorsal resection of the liver. J Am Coll Surg 179(1):72–75
Chaib E, Ribeiro MAF Jr, Maciel de Souza YED et al (2009) Anterior hepatic transection for caudate lobectomy. Clinics 64(11):1121–1125
Takayama T, Makuuchi M (1998) Segmental liver resections, present and future-caudate lobe resection for liver tumors. Hepatogastroenterology 45(19):20–23
Liu P, Qiu BA, Bai HW et al (2012) Choice of approach for hepatectomy for hepatocellular carcinoma located in the caudate lobe: Isolated or combined lobectomy? World J Gastroenterol 18(29):3904–3909
Zhou Y, Zhang X, Wu L et al (2012) Surgical outcomes of hepatocellular carcinoma originating from caudate lobe. ANZ J Surg 83(4):275–279
Dulucq JL, Wintringer P, Stabilini C et al (2006) Isorated laparoscopic resection of the hepatic caudate lobe: surgical technique and a report of 2 cases. Surg Laparosc Endosc Percutan Tech 16(1):32–35
Salloum C, Lahat E, Lim C et al (2016) Laparoscopic isolated resection of caudate lobe (segment 1): a safe and versatile technique. J Am Coll Surg 222(5):e61–e66
Jin B, Jiang Z, Hu S et al (2018) Surgical technique and clinical analysis of twelve cases of isolated laparoscopic resection of the hepatic caudate lobe. Biomed Res Int 2018:5848309
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Shimada, S., Kamiyama, T., Yokoo, H. et al. Prognoses and Clinicopathological Characteristics for Hepatocellular Carcinoma Originating from the Caudate Lobe After Surgery. World J Surg 43, 1085–1093 (2019). https://doi.org/10.1007/s00268-018-4869-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-018-4869-2