Abstract
Background
Noise pollution in operation rooms may distract the surgical team members. In particular during phases of high task complexity, noise can jeopardize concentration. Phases of high complexity are related to task specificities and may thus be different for different members of the surgical team.
Study design
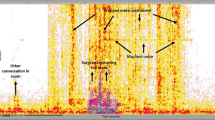
Noise exposure was measured during 110 open abdominal surgeries. Distinguishing three phases (opening, main phase, and closing), noise was related to self-report of distraction levels by main and secondary surgeons, scrub nurses and anesthetists.
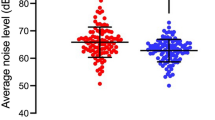
Results
Noise pollution was higher than recommended levels for concentrated work. Adjusted for duration, surgical type, and difficulty of the surgery, results showed that second surgeons are more likely distracted when noise pollution was high in the main phase; and anesthetists are more likely distracted when noise pollution was high during the closing phase. Main surgeons’ and scrub nurses’ concentration was not impaired by measured noise levels.
Conclusions
In phases with higher concentration demands, noise pollution was particularly distracting for second surgeons and anesthetist, corresponding to their specific task demands (anesthetists) and experience (second surgeons). Reducing noise levels particularly in the main and closing phase of the surgery may reduce concentration impairments.

Similar content being viewed by others
References
Katz JD (2014) Noise in the operating room. Surv Anesthesiol 121:894–898
Shankar N, Malhotra K, Ahuja S et al (2001) Noise pollution: a study of noise levels in the operation theatres of a general hospital during various surgical procedures. J Indian Med Assoc 99:244–247
Kam P, Kam A, Thompson J (1994) Noise pollution in the anaesthetic and intensive care environment. Anaesthesia 49:982–986
Healey AN, Primus CP, Koutantji M (2007) Quantifying distraction and interruption in urological surgery. Qual Saf Health Care 16:135–139
Berger EH, Royster LH, Royster JD et al (2003) The noise manual. American Industrial Hygiene Association, Fairfax
Engelmann CR, Neis JP, Kirschbaum C et al (2014) A noise-reduction program in a pediatric operation theatre is associated with surgeon’s benefits and a reduced rate of complications: a prospective controlled clinical trial. Ann Surg 259:1025–1033
Alshammari D, Sica M, Osailan S et al (2017) Noise in a university operating theatre during the cours of pediatric surgical procedures. Curr Pediatr Res 21:572–576
Hasfeldt D, Laerkner E, Birkelund R (2010) Noise in the operating room–what do we know? A review of the literature. J Perianesth Nurs 25:380–386
Hodge B, Thompson JF (1990) Noise pollution in the operating theatre. Lancet 335:891–894
Tsiou C, Efthymiatos G, Katostaras T (2008) Noise in the operating rooms of Greek hospitals. J Acoust Soc Am 123:757–765
Witterseh T, Wyon DP, Clausen G (2004) The effects of moderate heat stress and open-plan office noise distraction on SBS symptoms and on the performance of office work. Indoor Air 14:30–40
Basner M, Babisch W, Davis A et al (2014) Auditory and non-auditory effects of noise on health. Lancet 383:1325–1332
Rylander R (2004) Physiological aspects of noise-induced stress and annoyance. J Sound Vib 277:471–478
Szalma JL, Hancock PA (2011) Noise effects on human performance: a meta-analytic synthesis. Psychol Bull 137:682–707
Stansfeld SA, Matheson MP (2003) Noise pollution: non-auditory effects on health. Br Med Bull 68:243–257
Baker MA, Holding DH (1993) The effects of noise and speech on cognitive task performance. J Gen Psychol 120:339–355
Kurmann A, Peter M, Tschan F et al (2011) Adverse effect of noise in the operating theatre on surgical-site infection. Br J Surg 98:1021–1025
Grayson D, Boxerman S, Potter P, et al (2005) Do transient working conditions trigger medical errors?, DTIC Document
Dholakia S, Jeans JP, Khalid U et al (2015) The association of noise and surgical-site infection in day-case hernia repairs. Surgery 157:1153–1156
Moorthy K, Munz Y, Dosis A et al (2003) The effect of stress-inducing conditions on the performance of a laparoscopic task. Surg Endosc 17:1481–1484
Pluyter JR, Buzink SN, Rutkowski A-F et al (2010) Do absorption and realistic distraction influence performance of component task surgical procedure? Surg Endosc 24:902–907
Way TJ, Long A, Weihing J et al (2013) Effect of noise on auditory processing in the operating room. J Am Coll Surg 216:933–938
Keller S, Tschan F, Beldi G et al (2016) Noise peaks influence communication in the operating room. Observ Study Ergon 59:1541–1552
Moorthy K, Munz Y, Undre S et al (2004) Objective evaluation of the effect of noise on the performance of a complex laparoscopic task. Surgery 136:25–30
Suh IH, Chien JH, Mukherjee M et al (2010) The negative effect of distraction on performance of robot-assisted surgical skills in medical students and residents. Int J Med Robot Comput Assist Surg 6:377–381
Murthy VS, Malhotra SK, Bala I et al (1995) Detrimental effects of noise on anaesthesists. Can J Anaesth 42:608–611
Stevenson RA, Schlesinger JJ, Wallace MT (2013) Effects of divided attention and operating room noise on perception of pulse oximeter pitch changes: a laboratory study. Anesthesiology 118:376–381
Clark C, Sörqvist P (2012) A 3 year update on the influence of noise on performance and behavior. Noise Health 14:292–296
Loewen LJ, Suedfeld P (1992) Cognitive and arousal effects of masking office noise. Environ Behav 24:381–395
Wadhera RK, Parker SH, Burkhart HM et al (2010) Is the “sterile cockpit” concept applicable to cardiovascular surgery critical intervals or critical events? The impact of protocol-driven communication during cardiopulmonary bypass. J Thorac Cardiovasc Surg 139:312–319
Parker SH, Flin R, McKinley A et al (2014) Factors influencing surgeons’ intraoperative leadership: video analysis of unanticipated events in the operating room. World J Surg 38:4–10. https://doi.org/10.1007/s00268-013-2241-0
Broom MA, Capek AL, Carachi P et al (2011) Critical phase distractions in anaesthesia and the sterile cockpit concept. Anaesthesia 66:175–179
Jenkins A, Wilkinson JV, Akeroyd MA et al (2015) Distractions during critical phases of anaesthesia for caesarean section: an observational study. Anaesthesia 70:543–548
Wadhera RK, Parker SH, Burkhart HM et al (2010) Is the “sterile cockpit” concept applicable to cardiovascular surgery critical intervals or critical events? The impact of protocol-driven communication during cardiopulmonary bypass. J Thorac Cardiovasc Surg 139:312–319
Kurmann A, Keller S, Tschan-Semmer F et al (2014) Impact of team familiarity in the operating room on surgical complications. World J Surg 38:3047–3052. https://doi.org/10.1007/s00268-014-2680-2
Ryherd EE, Okcu S, Ackerman J et al (2012) Noise pollution in hospitals: impacts on staff. JCOM 19:491–500
Ginsberg SH, Pantin E, Kraidin J et al (2013) Noise levels in modern operating rooms during surgery. J Cardiothorac Vasc Anesth 27:528–530
Tschan F, Seelandt JC, Keller S et al (2015) Impact of case-relevant and case-irrelevant communication within the surgical team on surgical-site infection. Br J Surg 102:1718–1725
Katz P (1981) Ritual in the operating-room. Ethnology 20:335–350
Wahr JA, Prager RL, Abernathy JH 3rd et al (2013) Patient safety in the cardiac operating room: human factors and teamwork: a scientific statement from the American Heart Association. Circulation 128:1139–1169
Hsu KE, Man FY, Gizicki RA et al (2008) Experienced surgeons can do more than one thing at a time: effect of distraction on performance of a simple laparoscopic and cognitive task by experienced and novice surgeons. Surg Endosc 22:196–201
Galvan C, Bacha EA, Mohr J et al (2005) A human factors approach to understanding patient safety during pediatric cardiac surgery. Prog Pediatr Cardiol 20:13–20
Reiling J (2006) Safe design of healthcare facilities. Qual Saf Health Care 15(Suppl 1):i34–i40
MacLeod M, Dunn J, Busch-Vishniac IJ et al (2007) Quieting Weinberg 5C: a case study in hospital noise control. J Acoust Soc Am 121:3501–3508
South T (2004) Managing noise and vibration at work: a practical guide to assessment, measurement and control. Elsevier, Butterworth-Heinemann, Oxford
Acknowledgements
Dr. Anita Kurmann, a scientific advisor for this study, deceased August 7, 2015. We thank Julia Seelandt for her help in organization of data collection and data collection; Anna Püschel, Moana Monnier and Nadja Jenni for their contribution to data collection; Uwe Klopsch (technician) and Brigitte Dubach (head nurse) for their technical and organizational support.
Funding
This work was supported by the Swiss National Science Foundation [grant # CR13I1_138273 and CR13I3_156882].
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
None of the authors declares a conflict of interest
Rights and permissions
About this article
Cite this article
Keller, S., Tschan, F., Semmer, N.K. et al. Noise in the Operating Room Distracts Members of the Surgical Team. An Observational Study. World J Surg 42, 3880–3887 (2018). https://doi.org/10.1007/s00268-018-4730-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-018-4730-7