Abstract
Background
The focus of many data collection efforts centers on creation of more granular data. The assumption is that more complex data are better able to predict outcomes. We hypothesized that data are often needlessly complex. We sought to demonstrate this concept by examination of the American Society of Anesthesiologists (ASA) scoring system.
Methods
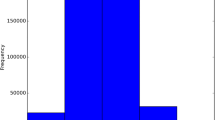
First, we created every possible consecutive two, three and four category combinations of the current five category ASA score. This resulted in 14 combinations of simplified ASA. We compared the predictive ability of these simplified scores for postoperative outcomes for 2.3 million patients in the NSQIP database. Individual model performance was assessed by comparing receiver operator characteristic (ROC) curves for each model with the standard ASA.
Results
Two of our 4-category models and one of our 3-category models had ability to predict all outcomes equivalent to standard ASA. These results held for all outcomes and on all subgroups tested. The performance of the three best performing simplified ASA scores were also equivalent to the standard ASA score in the univariate analysis and when included in a multivariate model.
Conclusions
It is assumed that the most granular data and use of the largest number of variables for risk-adjusted predictions will increase accuracy. This complexity is often at the expense of utility. Using the single best predictor in surgical outcomes research, we have shown this is not the case. In this example, we demonstrate that one can simplify ASA into a 3-category variable without losing any ability to predict outcomes.


Similar content being viewed by others
References
Khuri SF, Daley J, Henderson W et al (1998) The Department of Veterans Affairs’ NSQIP: the first national, validated, outcome-based, risk-adjusted, and peer-controlled program for the measurement and enhancement of the quality of surgical care. National VA Surgical Quality Improvement Program. Ann Surg 228:491–507
Khuri SFMDMS, Henderson WGP, Daley JMD et al (2008) Successful implementation of the Department of Veterans Affairs’ National Surgical Quality Improvement Program in the private sector: the patient safety in surgery study. Ann Surg 248:329–336
Shiloach M, Frencher SK, Steeger JE et al (2010) Toward robust information: data quality and inter-rater reliability in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg 210:6–16
Meara JG, Leather AJM, Hagander L et al (2015) Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet 386:569–624
Spence RT, Mueller JL, Chang DC (2016) A novel approach to global benchmarking of risk-adjusted surgical outcomes: beyond perioperative mortality rate. JAMA Surg 151:501–502
Anderson JE, Rose J, Noorbakhsh A et al (2014) An efficient risk adjustment model to predict inpatient adverse events after surgery. World J Surg 38:1954–1960. https://doi.org/10.1007/s00268-014-2490-6
O’Reilly GM, Gabbe B, Braaf S et al (2016) An interview of trauma registry custodians to determine lessons learnt. Injury 47:116–124
Nwomeh BC, Lowell W, Kable R et al (2006) History and development of trauma registry: lessons from developed to developing countries. World J Emerg Surg 1:32
GlobalSurg C (2016) Mortality of emergency abdominal surgery in high-, middle- and low-income countries. Br J Surg 103:971–988
Hoffmann M, Lefering R, Rueger JM et al (2012) Pupil evaluation in addition to Glasgow Coma Scale components in prediction of traumatic brain injury and mortality. Br J Surg 99:122–130
Gill M, Steele R, Windemuth R et al (2006) A comparison of five simplified scales to the out-of-hospital Glasgow Coma Scale for the prediction of traumatic brain injury outcomes. Acad Emerg Med 13:968–973
Daabiss M (2011) American Society of Anaesthesiologists physical status classification. Indian J Anaesth 55:111–115
Fitz-Henry J (2011) The ASA classification and peri-operative risk. Ann R Coll Surg Engl 93:185–187
Barbeito A, Muir HA, Gan TJ et al (2006) Use of a modifier reduces inconsistency in the American Society of Anesthesiologists Physical Status Classification in parturients. Anesth Analg 102:1231–1233
American College of S ACS National Surgical Quality Improvement Program® (ACS NSQIP®), Chicago, IL, 2017
Quinn JW, Barnard G, Rose J et al (2015) NSQIP-LITE: measuring surgical outcomes in Mozambique. The Lancet Commission on global surgery teaching case. Babson College, Wellesley
Saklad MDM (1941) Grading of patients for surgical procedures. Anesthesiology 2:281–284
Delegates AHo ASA Physical Status Classification System 2014
Grzybowski M, Younger JG (1997) Statistical methodology: III. Receiver operating characteristic (ROC) curves. Acad Emerg Med 4:818–826
Park SH, Goo JM, Jo C-H (2004) Receiver operating characteristic (ROC) curve: practical review for radiologists. Korean J Radiol 5:11–18
Metz CE (2006) Receiver operating characteristic analysis: a tool for the quantitative evaluation of observer performance and imaging systems. J Am Coll Radiol 3:413–422
Hanley JA, McNeil BJ (1982) The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 143:29–36
Centor RM (1991) Signal detectability: the use of ROC curves and their analyses. Med Decis Mak 11:102–106
Hoffmann MMDMBA, Lehmann WMDP, Rueger JMMDP et al (2012) Introduction of a novel trauma score. J Trauma Acute Care Surg 73:1607–1613
Schluter PJ (2011) Trauma and Injury Severity Score (TRISS): is it time for variable re-categorisations and re-characterisations? Injury 42:83–89
Schluter PJ (2011) The Trauma and Injury Severity Score (TRISS) revised. Injury 42:90–96
Moore LM, Lavoie AP, LeSage NMDM et al (2006) Statistical validation of the revised trauma score. J Trauma Injury Infect Crit Care 60:305–311
Kuhls DA, Malone DL, McCarter RJ et al (2002) Predictors of mortality in adult trauma patients: the Physiologic Trauma Score is equivalent to the Trauma and Injury Severity Score 1. J Am Coll Surg 194:695–704
Watters DA, Hollands MJ, Gruen RL et al (2015) Perioperative Mortality Rate (POMR): a global indicator of access to safe surgery and anaesthesia. World J Surg 39:856–864. https://doi.org/10.1007/s00268-014-2638-4
Ariyaratnam R, Palmqvist CL, Hider P et al (2015) Toward a standard approach to measurement and reporting of perioperative mortality rate as a global indicator for surgery. Surgery 158:17–26
Ng-Kamstra JS, Greenberg SLM, Kotagal M et al (2015) Use and definitions of perioperative mortality rates in low-income and middle-income countries: a systematic review. Lancet 385:S29
Elliott IS, Sonshine DB, Akhavan S et al (2015) What factors influence the production of orthopaedic research in east Africa? A qualitative analysis of interviews. Clin Orthop Relat Res 473:2120–2130
Silverstein A, Mugenzi P, Lule J et al (2016) Barriers to expansion of cancer research: data collection challenges at a single-institution in Rwanda. J Cancer Policy 7:1–3
Schultz CRMD, Ford HRMDF, Cassidy LDP et al (2007) Development of a hospital-based trauma registry in Haiti: an approach for improving injury surveillance in developing and resource-poor settings. J Trauma Injury Infect Crit Care 63:1143–1154
Sonshine DB, Shantz J, Kumah-Ametepey R et al (2013) The implementation of a pilot femur fracture registry at Komfo Anokye Teaching Hospital: an analysis of data quality and barriers to collaborative capacity-building. World J Surg 37:1506–1512. https://doi.org/10.1007/s00268-012-1726-6
Haynes SR, Lawler PGP (1995) An assessment of the consistency of ASA physical status classification allocation. Anaesthesia 50:195–199
Ranta S, Hynynen M, Tammisto T (1997) A survey of the ASA physical status classification: significant variation in allocation among Finnish anaesthesiologists. Acta Anaesthesiol Scand 41:629–632
Owens MD, William D, Felts MD, James A, Spitznagel PD, Edward L (1978) ASA physical status classifications: a study of consistency of ratings. Anesthesiology 49:239–243
Acknowledgements
Funding was provided by the Massachusetts General Hospital and the Codman Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Anderson, G.A., Bohnen, J., Spence, R. et al. Data Improvement Through Simplification: Implications for Low-Resource Settings. World J Surg 42, 2725–2731 (2018). https://doi.org/10.1007/s00268-018-4535-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-018-4535-8