Abstract
Background
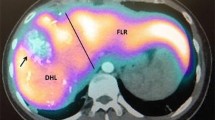
Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) has recently emerged as a treatment choice for patients with colorectal liver metastases (CLM) and inadequate future liver remnant (FLR). The aim of this study was to define the results of ALPPS compared with two-stage hepatectomy (TSH) for patients with CLM.
Materials and methods
A meta-analysis was conducted in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analysis guidelines. Identification of eligible studies was performed using three distinct databases through February 2017; Medline, ClinicalTrials.gov and Cochrane library—Cochrane Central Register of Controlled Trials using a syntax including medical subject headings terms “portal vein ligation,” “PVE,” “staged hepatectomy,” “staged liver resection,” “liver resection,” “two-stage hepatectomy,” “TSH,” “in situ liver transection with portal vein ligation,” “associating liver partition and portal vein ligation for staged hepatectomy” and “ALPPS”.
Results
Among the 634 records identified, 9 studies comparing ALPPS with TSH met the inclusion criteria. These studies included 657 patients with unresectable CLM (ALPPS, n = 186 vs TSH, n = 471). There was no difference in final postoperative FLR between ALPPS versus TSH (mean difference: 31.72, 95% CI: −27.33 to 90.77, p = 0.29). The kinetic growth rate was faster with the ALPPS versus TSH (mean difference 19.07 ml/day, 95% CI 8.12–30.02, p = 0.0006). TSH had a lower overall and major morbidity versus ALPPS (overall morbidity: RR: 1.39, 95% CI: 1.07–1.8, p = 0.01; I 2: 58%, p = 0.01; major morbidity: RR: 1.57, 95% CI: 1.18–2.08, p = 0.002; I 2: 0%, p = 0.44). Overall survival was comparable following ALPPS versus TSH.
Conclusion
While ALPPS may be a suitable approach for patients, the higher morbidity and mortality should be considered when determining the operative approach for patients with extensive CLM.





Similar content being viewed by others

References
Ferlay J, Shin HR, Bray F et al (2010) Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 127:2893–2917
Siegel R, Naishadham D, Jemal A (2012) Cancer statistics, 2012. CA Cancer J Clin 62:10–29
Abdalla EK, Adam R, Bilchik AJ et al (2006) Improving resectability of hepatic colorectal metastases: expert consensus statement. Ann Surg Oncol 13:1271–1280
de Haas RJ, Wicherts DA, Andreani P et al (2011) Impact of expanding criteria for resectability of colorectal metastases on short- and long-term outcomes after hepatic resection. Ann Surg 253:1069–1079
Saiura A, Yamamoto J, Koga R et al (2014) Favorable outcome after repeat resection for colorectal liver metastases. Ann Surg Oncol 21:4293–4299
House MG, Ito H, Gonen M, et al. (2010) Survival after hepatic resection for metastatic colorectal cancer: trends in outcomes for 1,600 patients during two decades at a single institution. J Am Coll Surg 210: 744–752, 752–745
Kanas GP, Taylor A, Primrose JN et al (2012) Survival after liver resection in metastatic colorectal cancer: review and meta-analysis of prognostic factors. Clin Epidemiol 4:283–301
Moris D, Dimitroulis D, Vernadakis S et al (2017) Parenchymal-sparing hepatectomy as the new doctrine in the treatment of liver-metastatic colorectal disease: beyond oncological outcomes. Anticancer Res 37:9–14
Lafaro K, Buettner S, Maqsood H et al (2015) Defining post hepatectomy liver insufficiency: where do we stand? J Gastrointest Surg Off J Soc Surg Alimentary Tract 19:2079–2092
Adam R, Laurent A, Azoulay D et al (2000) Two-stage hepatectomy: a planned strategy to treat irresectable liver tumors. Ann Surg 232:777–785
Masi G, Vasile E, Loupakis F et al (2011) Randomized trial of two induction chemotherapy regimens in metastatic colorectal cancer: an updated analysis. J Natl Cancer Inst 103:21–30
Van Cutsem E, Kohne CH, Hitre E et al (2009) Cetuximab and chemotherapy as initial treatment for metastatic colorectal cancer. N Engl J Med 360:1408–1417
Tschuor C, Croome KP, Sergeant G et al (2013) Salvage parenchymal liver transection for patients with insufficient volume increase after portal vein occlusion—an extension of the ALPPS approach. Eur J Surg Oncol J Eur Soc Surg Oncol Br Assoc Surg Oncol 39:1230–1235
Bjornsson B, Sparrelid E, Rosok B et al (2016) Associating liver partition and portal vein ligation for staged hepatectomy in patients with colorectal liver metastases—intermediate oncological results. Eur J Surg Oncol 42:531–537
Jaeck D, Oussoultzoglou E, Rosso E et al (2004) A two-stage hepatectomy procedure combined with portal vein embolization to achieve curative resection for initially unresectable multiple and bilobar colorectal liver metastases. Ann Surg 240:1037–1049 (discussion 1049–1051)
Schadde E, Ardiles V, Robles-Campos R et al (2014) Early survival and safety of ALPPS: first report of the international ALPPS Registry. Ann Surg 260:829–836 (discussion 836–828)
Schadde E, Ardiles V, Slankamenac K et al (2014) ALPPS offers a better chance of complete resection in patients with primarily unresectable liver tumors compared with conventional-staged hepatectomies: results of a multicenter analysis. World J Surg 38:1510–1519. doi:10.1007/s00268-014-2513-3
Zhang GQ, Zhang ZW, Lau WY et al (2014) Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS): a new strategy to increase resectability in liver surgery. Int J Surg 12:437–441
Schnitzbauer AA, Lang SA, Goessmann H et al (2012) Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small-for-size settings. Ann Surg 255:405–414
de Santibanes E (2012) Clavien PA playing Play-Doh to prevent postoperative liver failure: the “ALPPS” approach. Ann Surg 255:415–417
Moher D, Liberati A, Tetzlaff J et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 62:1006–1012
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5:13
Shindoh J, Vauthey JN, Zimmitti G et al (2013) Analysis of the efficacy of portal vein embolization for patients with extensive liver malignancy and very low future liver remnant volume, including a comparison with the associating liver partition with portal vein ligation for staged hepatectomy approach. J Am Coll Surg 217:126–133 (discussion 133–124)
Croome KP, Hernandez-Alejandro R, Parker M et al (2015) Is the liver kinetic growth rate in ALPPS unprecedented when compared with PVE and living donor liver transplant? A multicentre analysis. HPB Off J Int Hepato Pancreato Biliary Assoc 17:477–484
Matsuo K, Murakami T, Kawaguchi D et al (2016) Histologic features after surgery associating liver partition and portal vein ligation for staged hepatectomy versus those after hepatectomy with portal vein embolization. Surgery 159:1289–1298
Tanaka K, Matsuo K, Murakami T et al (2015) Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS): short-term outcome, functional changes in the future liver remnant, and tumor growth activity. Eur J Surg Oncol J Eur Soc Surg Oncol Br Assoc Surg Oncol 41:506–512
Ratti F, Schadde E, Masetti M et al (2015) Strategies to increase the resectability of patients with colorectal liver metastases: a multi-center case-match analysis of alpps and conventional two-stage hepatectomy. Ann Surg Oncol 22:1933–1942
Knoefel WT, Gabor I, Rehders A et al (2013) In situ liver transection with portal vein ligation for rapid growth of the future liver remnant in two-stage liver resection. Br J Surg 100:388–394
Kambakamba P, Linecker M, Alvarez FA et al (2016) Short chemotherapy-free interval improves oncological outcome in patients undergoing two-stage hepatectomy for colorectal liver metastases. Ann Surg Oncol 23:3915–3923
Adam R, Imai K, Castro Benitez C et al (2016) Outcome after associating liver partition and portal vein ligation for staged hepatectomy and conventional two-stage hepatectomy for colorectal liver metastases. Br J Surg 103:1521–1529
Adam R, Avisar E, Ariche A et al (2001) Five-year survival following hepatic resection after neoadjuvant therapy for nonresectable colorectal. Ann Surg Oncol 8:347–353
Yamamoto J, Kosuge T, Takayama T et al (1996) Recurrence of hepatocellular carcinoma after surgery. Br J Surg 83:1219–1222
Ulmer TF, de Jong C, Andert A et al (2017) ALPPS procedure in insufficient hypertrophy after portal vein embolization (PVE). World J Surg 41:250–257. doi:10.1007/s00268-016-3662-3
Fard-Aghaie MH, Stavrou GA, Schuetze KC et al (2015) ALPPS and simultaneous right hemicolectomy—step one and resection of the primary colon cancer. World J Surg Oncol 13:124
Petrou A, Moris D, Kountourakis P et al (2016) The ALPPS procedure as a novel “liver-first” approach in treating liver metastases of colon cancer: the first experience in Greek Cypriot area. World J Surg Oncol 14:67
Chan AC, Poon RT, Chan C et al (2016) Safety of ALPPS procedure by the anterior approach for hepatocellular carcinoma. Ann Surg 263:e14–16
Hernandez-Alejandro R, Bertens KA, Pineda-Solis K et al (2015) Can we improve the morbidity and mortality associated with the associating liver partition with portal vein ligation for staged hepatectomy (ALPPS) procedure in the management of colorectal liver metastases? Surgery 157:194–201
Abulkhir A, Limongelli P, Healey AJ et al (2008) Preoperative portal vein embolization for major liver resection: a meta-analysis. Ann Surg 247:49–57
Truant S, Scatton O, Dokmak S et al (2015) Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS): impact of the inter-stages course on morbi-mortality and implications for management. Eur J Surg Oncol J Eur Soc Surg Oncol Br Assoc Surg Oncol 41:674–682
Alvarez FA, Ardiles V, de Santibanes M et al (2015) Associating liver partition and portal vein ligation for staged hepatectomy offers high oncological feasibility with adequate patient safety: a prospective study at a single center. Ann Surg 261:723–732
Moris D, Vernadakis S, Papalampros A et al (2016) Mechanistic insights of rapid liver regeneration after associating liver partition and portal vein ligation for stage hepatectomy. World J Gastroenterol 22:7613–7624
Moris D, Pawlik TM (2016) Liver hypoxia as a trigger to liver regeneration: no more than another piece of the puzzle. Surgery 161:1176–1177
Schadde E, Tsatsaris C, Swiderska-Syn M et al (2016) Hypoxia of the growing liver accelerates regeneration. Surgery 161:666–679
Aloia TA, Vauthey JN (2012) Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS): what is gained and what is lost? Ann Surg 256:e9 (author reply e16–19)
Dokmak S, Belghiti J (2012) Which limits to the “ALPPS” approach? Ann Surg 256:e6 (author reply e16–17)
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Moris, D., Ronnekleiv-Kelly, S., Kostakis, I.D. et al. Operative Results and Oncologic Outcomes of Associating Liver Partition and Portal Vein Ligation for Staged Hepatectomy (ALPPS) Versus Two-Stage Hepatectomy (TSH) in Patients with Unresectable Colorectal Liver Metastases: A Systematic Review and Meta-Analysis. World J Surg 42, 806–815 (2018). https://doi.org/10.1007/s00268-017-4181-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-017-4181-6