Abstract
Background
The effectiveness of 14-French (14F) pigtail catheters (PCs) compared to 32-40F chest tubes (CTs) in patients with traumatic hemothorax (HTX) and hemopneumothorax (HPTX) is becoming more well known but still lacking. The aim of our study was to analyze our cumulative experience and outcomes with PCs in patients with traumatic HTX/HPTX. We hypothesized that PCs would be as effective as CTs.
Methods
Using our PC database, we analyzed all trauma patients who required chest drainage for HTX/HPTX from 2008 to 2014. Primary outcomes of interest, comparing PCs to CTs, included initial drainage output in milliliters (mL), tube insertion-related complications, and failure rate. For our statistical analysis, we used the unpaired Student’s t test, Chi-square test, and Wilcoxon rank-sum test. We defined statistical significance as P < 0.05.
Results
During the 7-year period, 496 trauma patients required chest drainage for traumatic HTX/HPTX: 307 by CTs and 189 by PCs. PC patients were older (52 ± 21 vs. 42 ± 19, P < 0.001), demonstrated a significantly higher occurrence of blunt trauma (86 vs. 55%, P ≤ 0.001), and had tubes placed in a non-emergent fashion (Day 1 [interquartile range (IQR) 1–3 days] for PC placement vs. Day 0 [IQR 0–1 days] for CT placement, P < 0.001). All primary outcomes of interest were similar, except that the initial drainage output for PCs was higher (425 mL [IQR 200–800 mL] vs. 300 mL [IQR 150–500], P < 0.001). Findings for subgroup analysis among emergent and non-emergent PC placement were also similar to CT placement.
Conclusion
PCs had similar outcomes to CTs in terms of failure rate and tube insertion-related complications, and the initial drainage output from PCs was not inferior to that of CTs. The usage of PCs was, however, selective. A future multi-center study is needed to provide additional support and information for PC usage in traumatic HTX/HPTX.
Similar content being viewed by others
Introduction
14-French (14F) pigtail catheters (PCs) are small-caliber catheters placed percutaneously at the bedside, which is in contrast to traditional large-caliber (32-40F) chest tubes (CTs) placed by an open cut-down technique [1,2,3]. The effectiveness of PC in the management of trauma patients with pneumothorax [3] and hemothorax (HTX)/hemopneumothorax (HPTX) (4) has previously been published. Nonetheless, its use remains controversial and its adoption in some centers remains slow but continues to gradually increase. Many clinicians still question, for instance, whether blood in the chest cavity can be drained effectively by such a small-caliber PC, and whether one always needs a larger-caliber CT to drain the blood properly [5, 6]. Although there are a number of studies demonstrating the effectiveness of PCs at draining pleural effusions [7, 8], it is important to remember HTX/HPTX demonstrate a very different physiology given the ability of blood to clot. Current literature examining the effectiveness of PC usage in traumatic HTX/HPTX compared to traditional CT usage remains scare.
Specific benefits of a PC placed percutaneously with a small skin incision include significantly less tissue trauma and less pain at the insertion site [9]. Having previously published our experiences with PC usage on a small sample of patients with traumatic HTX/HPTX (4) and given that other clinicians’ experiences with PC usage on such patients are still limited, we wanted to continue to share our experience with PC usage and see if PC placement remains effective as our experience in their usage has increased.
The aim of our study was to analyze our cumulative experience and outcomes with PC usage in patients with traumatic HTX/HPTX. We hypothesize that PCs are just as effective as CTs in terms of initial drainage output, insertion-related complications, and failure rate.
Methods
Using our ongoing prospective PC database and our trauma registry, we analyzed all trauma patients who required chest drainage for traumatic HTX/HPTX from 2008 to 2014 at Banner-University of Arizona Medical Center, a Level-I trauma center. The database was prospectively maintained by one of the attending trauma surgeons (NK). Analyzed data include demography, mechanism of injury, injury severity score (ISS), chest abbreviated injury scale score (c-AIS), indications for tube placement, day from the arrival of the patient to tube insertion (“Day 0” tube insertion was defined as the insertion during initial evaluation and resuscitation in trauma bay and any insertion outside of that setting was considered “Day 1” or later), initial drainage output, insertion-related complications, number of tube days, mechanical ventilation use and ventilation days, intensive care unit (ICU) length of stay (LOS), hospital length of stay (HLOS), and mortality.
Primary outcomes of interest included initial drainage output in milliliters (mL), insertion-related complications, and failure rate. Failure rate was defined as incompletely drained or retained HTX that required a second intervention; for example, second PC or CT placement, interventional radiology-guided drainage, intrapleural thrombolysis, or video-assisted thoracoscopy (VATS). Our institution routinely favors the practice of early VATS within the first week, typically on hospital day 3–5. The decision of how to treat the retained HTX was left to the discretion of the managing trauma surgeon based on daily clinical status, daily chest X-ray (CXR) findings and a confirmatory computed tomographic scan. Secondary outcomes of interest included total ventilator and ICU days, HLOS, total tube days, and mortality.
Both CTs and PCs were placed by the members of our trauma team, which included the in-house trauma surgeon, surgical residents/fellows and/or emergency medicine residents under direct supervision and assistance of the in-house trauma surgeon attending. Typically, the 14F PCs (Cook Critical Care: Cook Incorporated, Bloomington, IN, Fig. 1) were placed at the bedside in the trauma bay or patient room by utilizing a modified Seldinger technique. Most often, the insertion approach was via the lateral mid-axillary line or anterolateral chest wall in the fourth or fifth intercostal space. After the procedure, a CXR was always obtained to confirm appropriate tube placement and location.
Data were described as mean ± standard deviation (SD), the median and 25th and 75th interquartile range (IQR), or as a percentage. Categorical data were analyzed by Chi-square test, nonparametric continuous data by a Wilcoxon rank-sum test, and normally distributed continuous data by an unpaired Student t test. Significance was defined as P value < 0.05. For our statistical analysis, we used STATA14 (College Station, TX). The Institution Review Board of the Banner-University of Arizona Medical Center approved the study.
Results
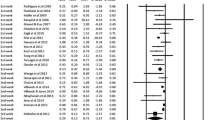
During the study period, our use of PCs in patients with traumatic HTX and HPTX increased significantly (Fig. 2, P < 0.001). Table 1 compares the generalized characteristics and outcomes of PCs and traditional CTs for all patients included in the study. Despite the similar or non-inferior results in the primary outcomes of interest (i.e., initial drainage output, insertion-related complications, and failure rate), PCs were still placed selectively in older trauma patients suffering blunt trauma and these tubes were usually placed in a delayed, non-emergent situation, that is, tube insertion day 1 (PC insertion at day 1 (IQR 1–3 days) vs. CT insertion at day 0 (IQR 0–1 days), P < 0.001).
As our comfort level and experience with PC usage continued to increase over this time period, so too did the use of PCs during emergent situations (see Table 2, non-emergent vs. Table 3 emergent placement comparison). Emergent placement (“Day 0”) is defined as placement of the CT or PC in the trauma bay shortly after patient presentation from the initial traumatic injury. Non-emergent placement (Greater than “Day 0”) is defined as placement of the chest drainage tube beyond the stay in the trauma bay from the initial traumatic injury or the number of days after the traumatic injury occurred if the patient had a delayed presentation. As Table 3 demonstrates, initial drainage output, insertion-related complications, and failure rates remained unaffected by the 14F PCs placed under emergent situations. Table 4 provides a description of tube insertion-related complications. The overall incidence was similar between PCs and CTs.
Discussion
The aim of this study was to analyze and share our cumulative experience and outcomes of PC usage in patients with traumatic HTX/HPTX. After 7 years and almost 200 patients, we found that in a selective subset of our study patients, PCs were just as effective as traditional CTs in terms of initial drainage output, insertion-related complications, and failure rate. In fact, PCs demonstrated a higher initial drainage output than CTs. Although there continued to be a selection bias toward placing PCs in non-emergent situations as well as older patients with blunt trauma, enhanced level of experience and growing comfort level allowed us to start using PCs in more emergent situations, including those patients presenting with penetrating trauma (N = 11, 9%, Table 3).
There is no other published series about PC usage in patients with traumatic HTX/HPTX. We published our first series 4 years ago, but that study contained only 36 patients and our level of experience was limited [4]. Though Russo et al. demonstrated the practicality of PC usage by using the ex-vivo swine model, they also concluded that there was no difference in the volume of blood drained by 14F PCs compared to 32F CTs [10]. This fact might as well be supported by our similar incidence of VATS between our 2 groups, supporting the dictum that blood will drain through a small-caliber tube but retained clot will not drain through a larger-caliber tube.
We did experience insertion-related complications early on in our learning curve, including PC placement for other indications such as pneumothorax [3] and pleural effusion. Over the past 3 years, however, we have experienced less technical failure in terms of conversion to a cut-down, traditional placement procedure (Table 4). We also experienced 2 additional major insertion-related complications involving intra-hepatic and through-the-spleen placement (Fig. 3). Fortunately, in both of these patients, the PCs were withdrawn and patients were successfully managed non-operatively without adverse sequela. These 2 major insertion-related complications serve as cautionary occurrence to highlight the possibility of a PC-related insertion complication due to an inadvertent placement of the needle that is either too low and/or too deep as it penetrates the costophrenic angle space and unintentionally enters the abdominal cavity, which can possibly injure the liver and spleen. It is important to remember that with any procedure, there is always the possibility for technical failures. Although rare, placement of a CT (or PC for that matter) into the abdominal cavity has been well described in current literature [11]. It is thought that sometimes what is identified as the fourth or fifth intercostal space may actually be the sixth, seventh or even eighth intercostal space [11]. It is important to keep in mind that the ribs curve upward moving anterior to a more lateral position and therefore entrance into the pleural space with either a CT or PC needs to be adjusted accordingly. Furthermore, patients suffering chest trauma will often splint or not take deep breaths due to the pain. This can result in the diaphragm elevating as high as the fourth intercostal space and inadvertent placement of the CT or PC into the abdominal cavity [11].
In general, the learning curve for the PC placement is relatively quick as the procedure is considered relatively simple compared to a chest tube. However, in an academic environment with constant rotations of residents and fellows, it took years of usage before we started seeing the frequency of complications decreased. The insertion-related complication rate in the latter half of the study was lower than the first half of the reporting period. Of note, 8 of the 17 PC reported insertion-related complications were a conversion to CT when PC attempts failed. In essence, these patients did not suffer from a complication per se as patients only required the default cut-down, traditional large-bore CT placement.
Despite its limitations, this study clearly demonstrates favorable outcomes in PC usage in the care and management of patients with traumatic HTX/HPTX. One limitation of this study is that it is a single institution series. However, as pointed out by Dr. Kenji Inaba in the editorial critique at the end of the Russo et al. study, “The highest yield next step would be a prospective multi-center clinical evaluation [10].” Additionally, despite the senior author’s (NK) attempt to maintain the PC database prospectively, it is still possible that the authors could have missed capturing some other minor insertion-related complications. It is generally well recognized that the incidence of tube insertion-related complications is underreported, particularly minor ones such as tube dislodgement and tube malposition [2]. Lastly, allowing the managing trauma surgeon the ability to choose between placement of a PC versus a CT introduces bias into the study, especially during those early years when PC was so new and there was a learning curve. As evident from our data, this resulted in PCs being placed in a more delayed fashion for older patients suffering blunt trauma. As previously stated, a multi-center, randomized, prospective trial should eliminate this bias. After analysis of our current data, however, the trend toward non-inferiority of PC usage versus CT usage remains promising in all settings.
Conclusion
The authors found that at our institution PC usage for patients with traumatic HTX/HPTX had similar outcomes to CT usage in terms of tube insertion-related complications and failure rate. Furthermore, PCs appeared to have better initial drainage output when compared to CTs further supporting their non-inferiority. Given our results, we recommend placement of a 14Fr pigtail catheter over a large-bore chest tube for traumatic HTX/HPTX; however, we also recommend a future multi-center study be completed to help improve the experience regarding PC usage and their overall effectiveness.
References
Dubose JA, O’Connor JV, Scalea TM (2013) Lung, trachea, and esophagus. In: Moore EE, Feliciano DV, Mattox ML (eds) Trauma, 7th edn. McGraw-Hill, New York, pp 468–470
Aho JM, Ruparel RK, Rowse PG et al (2015) Tube thoracostomy: a structured review of case reports and standardized format for reporting complications. World J Surg 39:2691–2706
Kulvatunyou N, Vijayasekaran A, Hansen A et al (2011) Two-year experience of using pigtail catheters to treat traumatic pneumothorax: a changing trend. J Trauma 71(5):1104–1107
Kulvatunyou N, Joseph B, Friese RS et al (2012) 14 French pigtail catheters placed by surgeons to drain blood on trauma patients: is 14-Fr too small? J Trauma Acute Care Surg 6:1421–1425
Inaba K, Lustengerger T, Recinos G et al (2012) Does size matter? A prospective analysis of 28–32 versus 36–40 French chest tube size in trauma. J Trauma Acute Care Surg 72:422–427
Dubose J, Inaba K, Demetriades D et al (2012) Management of post-traumatic retained hemothorax: a prospective, observational, multicenter AAST study. J Trauma Acute Care Surg 72(1):11–24
Aziz F, Penupolu S, Flores D (2012) Efficacy of percutaneous pigtail catheters for thoracostomy at bedside. J Thorac Dis 4(3):292–295
Liu YH, Lin YC, Liang SJ et al (2010) Ultrasound-guided pigtail catheters for drainage of various pleural disease. Am J Emerg Med 28(8):915–921
Kulvatunyou N, Erickson L, Vijayasekaran A et al (2014) Randomized clinical trial of pigtail catheter versus chest tube in injured patient with uncomplicated traumatic pneumothorax. BJS 101:17–22
Russo RM, Zakaluzny SA, Neff PL et al (2015) A pilot study of chest tube versus pigtail catheter drainage of acute hemothorax in swine. J Trauma Acute Care Surg 79:1038–1043
Kwiatt M, Tarbox A, Seamon MJ et al (2014) Thoracostomy tubes: a comprehensive review of complications and related topics. Int J Crit Inj Sci 4(2):143–155
Acknowledgements
We thank M. Melissa McCormick, BA, MA, for her assistance with reviewing and editing this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bauman, Z.M., Kulvatunyou, N., Joseph, B. et al. A Prospective Study of 7-Year Experience Using Percutaneous 14-French Pigtail Catheters for Traumatic Hemothorax/Hemopneumothorax at a Level-1 Trauma Center: Size Still Does Not Matter. World J Surg 42, 107–113 (2018). https://doi.org/10.1007/s00268-017-4168-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-017-4168-3