Abstract
Background
Prolonging post-operative antibiotic treatment beyond 3 days does not seem to reduce the incidence of post-operative abscess formation or wound infection after surgery for complicated appendicitis. The route of administration seems to be based on an empirical basis. Using enteral antibiotics could reduce length of stay and reduce overall costs. We aimed to examine whether treatment with enteral antibiotics during the first three post-operative days is non-inferior to intravenous antibiotics regarding intra-abdominal abscess formation or wound infection after surgery for complicated appendicitis.
Methods
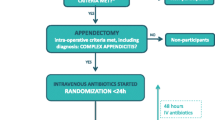
A retrospective study of adult patients having surgery for complicated appendicitis within a period of 32 months in the Capital Region of Denmark. Primary outcome was the incidence of post-operative abscess formation, and secondary outcome was wound infections, both within 30 days of surgery. Route of antibiotic administration for the first three post-operative days was registered for all patients.
Results
A total of 1141 patients were included in the study. The overall risk of developing an intra-abdominal abscess was 6.7% (95% CI 5.2%; 8.1%), and the risk of wound infection was 1.2% (95% CI 0.6%; 1.8%). In a multivariate intention-to-treat analysis, patients treated post-operatively with enteral antibiotics had an odds ratio of 0.78 (95% CI 0.41; 1.45, p = 0.429) for developing an intra-abdominal abscess and an odds ratio of 0.86 (95% CI 0.17; 4.29, p = 0.851) for developing a wound infection compared to patients treated post-operatively with intravenous antibiotics.
Conclusion
Treatment with enteral antibiotics was non-inferior compared to treatment with intravenous antibiotics during the first 3 days after surgery for complicated appendicitis.

Similar content being viewed by others
References
Collaborative G (2016) Mortality of emergency abdominal surgery in high-, middle- and low-income countries. Br J Surg. doi:10.1002/bjs.10151
Addiss DG, Shaffer N, Fowler BS, Tauxe RV (1990) The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol 132:910–925
Buckius MT, McGrath B, Monk J et al (2012) Changing epidemiology of acute appendicitis in the United States: study period 1993–2008. J Surg Res 175:185–190. doi:10.1016/j.jss.2011.07.017
Van Rossem CC, Schreinemacher MHF, Treskes K et al (2014) Duration of antibiotic treatment after appendicectomy for acute complicated appendicitis. Br J Surg 101:715–719. doi:10.1002/bjs.9481
Alamili M, Gögenur I, Rosenberg J (2010) Oral antibiotics for perforated appendicitis is not recommended. Dan Med Bull 57:A4177
Daskalakis K, Juhlin C, Påhlman L (2014) The use of pre- or postoperative antibiotics in surgery for appendicitis: a systematic review. Scand J Surg 103:14–20. doi:10.1177/1457496913497433
van Rossem CC, Schreinemacher MHF, van Geloven AAW, Bemelman WA (2015) Antibiotic duration after laparoscopic appendectomy for acute complicated appendicitis. JAMA Surg 151:1. doi:10.1001/jamasurg.2015.4236
Banani SA, Talei A (1999) Can oral metronidazole substitute parenteral drug therapy in acute appendicitis? A new policy in the management of simple or complicated appendicitis with localized peritonitis: a randomized controlled clinical trial. Am Surg 65:411–416
von Elm E, Altman DG, Egger M et al (2007) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet (Lond) 370:1453–1457. doi:10.1016/S0140-6736(07)61602-X
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213. doi:10.1097/01.sla.0000133083.54934.ae
Kimbrell AR, Novosel TJ, Collins JN et al (2014) Do postoperative antibiotics prevent abscess formation in complicated appendicitis? Am Surg 80:878–883
Kim DY, Nassiri N, Saltzman DJ et al (2015) Postoperative antibiotics are not associated with decreased wound complications among patients undergoing appendectomy for complicated appendicitis. Am J Surg. doi:10.1016/j.amjsurg.2015.07.001
Funding
The primary author received a research grant from Nordsjællands Hospital and financial support from the Department of Surgery, Nordsjællands Hospital, Copenhagen University Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Declaration of interests
The authors declare that they have no competing interests.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kleif, J., Rasmussen, L., Fonnes, S. et al. Enteral Antibiotics are Non-inferior to Intravenous Antibiotics After Complicated Appendicitis in Adults: A Retrospective Multicentre Non-inferiority Study. World J Surg 41, 2706–2714 (2017). https://doi.org/10.1007/s00268-017-4076-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-017-4076-6