Abstract
Background
There are little primary data available on the delivery or quality of surgical treatment in rural sub-Saharan African hospitals. To initiate a quality improvement system, we characterized the existing data capture at a Ugandan Regional Referral Hospital.
Methods
We examined the surgical ward admission (January 2008–December/2011) and operating theater logbooks (January 2010–July 2011) at Mbarara Regional Referral Hospital.
Results
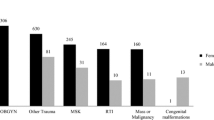
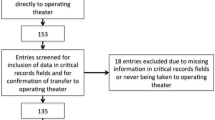
There were 6346 admissions recorded over three years. The mean patient age was 31.4 ± 22.3 years; 29.8 % (n = 1888) of admissions were children. Leading causes of admission were general surgical problems (n = 3050, 48.1 %), trauma (n = 2041, 32.2 %), oncology (n = 718, 11.3 %) and congenital condition (n = 193, 3.0 %). Laparotomy (n = 468, 35.3 %), incision and drainage (n = 188, 14.2 %) and hernia repair (n = 90, 6.8 %) were the most common surgical procedures. Of 1325 operative patients, 994 (75 %) had an ASA I–II score. Of patients undergoing 810 procedures booked as non-elective, 583 (72 %) had an ASA “E” rating. Records of 41.3 % (n-403/975) of patients age 5 years or older undergoing non-obstetric operations were missing from the ward logbook. Missing patients were younger (25 [13,40] versus 30 [18,46] years, p = 0.002) and had higher ASA scores (ASA III-V 29.0 % versus 18.9 %, p < 0.001) than patients recorded in the logbbook; there was no diffence in gender (male 62.8 % versus 67.0 %, p = 0.20).
Conclusions
The hospital records system measures surgical care, but improved data capture is needed to determine outcomes with sufficient accuracy to guide and record expansion of surgical capacity.

Similar content being viewed by others
References
Meara JG, Leather AJ, Hagander L et al (2015) Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet 386:569–624
Shrime MG, Bickler SW, Alkire BC et al (2015) Global burden of surgical disease: an estimation from the provider perspective. Lancet Glob Health 3(Suppl 2):S8–S9
Rose J, Weiser TG, Hider P et al (2015) Estimated need for surgery worldwide based on prevalence of diseases: a modeling strategy for the WHO Global Health Estimate. Lancet Glob Health 3(Suppl 2):S13–S20
Bickler SN, Weiser TG, Kassebaum N et al (2015) Chapter 2: Global burden of surgical conditions. In: Debras HT, Donfor P, Gawande A et al (eds) Essential surgery: disease control priorities, 3rd edn., vol 1. World Bank, Washington, DC
Sixthy-Eighth World Health Assembly (2015, May 26) Resolution WHA 68.15, Strengthening emergency and essential surgical care and anaesthesia as a component of universal health coverage. http://apps.who.int/gb/ebwha/pdf_files/WHA68/A68_R15-en.pdf
Barnighausen T, Bloom DE, Humair S (2011) Going horizontal—shifts in funding of global health interventions. N Engl J Med 364:2181–2183
Wang H, Dwyer-Lindgren L, Lofgren KT et al (2012) Age-specific and sex-specific mortality in 187 countries, 1970–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380:2071–2094
Chan M, Kazatchkine M, Lob-Levyt J et al (2010) Meeting the demand for results and accountability: a call for action on health data from eight global health agencies. PLoS Med 7:e1000223
Rottingen JA, Regmi S, Eide M et al (2013) Mapping of available health research and development data: what’s there, what’s missing, and what role is there for a global observatory? Lancet 382:1286–1307
Funk LM, Weiser TG, Berry WR et al (2010) Global operating theatre distribution and pulse oximetry supply: an estimation from reported data. Lancet 376:1055–1061
Bickler S, Ozgediz D, Gosselin R et al (2010) Key concepts for estimating the burden of surgical conditions and the unmet need for surgical care. World J Surg 34:374–380
Weiser TG, Regenbogen SE, Thompson KD et al (2008) An estimation of the global volume of surgery: a modeling strategy based on available data. Lancet 372:139–144
Central Intelligence Agency (2015) The World Factbook. https://www.cia.gov/library/publications/the-world-factbook/
Linden AF, Sekidde FS, Galukande M et al (2012) Challenges of surgery in developing countries: a survey of surgical and anesthesia capacity in Uganda’s public hospitals. World J Surg 36:1056–1065
World Health Organization. Tool for situational analysis to assess emergency and essential surgical care WHO integrated management for emergency and essential surgical care (IMEESC) toolkit. http://www.who.int/surgery/publications/imeesc/en/index.html
http://www.citypopulation.de/php/uganda-admin.php. Accessed 2014
Walker IA, Obua AD, Mouton F et al (2010) Paediatric surgery and anaesthesia in south-western Uganda: a cross-sectional survey. Bull World Health Organ 88:897–906
Laing GL, Skinner DL, Bruce JL et al (2014) A multi faceted quality improvement programme results in improved outcomes for the selective non-operative management of penetrating abdominal trauma in a developing world trauma centre. Injury 45:327–332
Ralston ME, Day LT, Slusher TM et al (2013) Global paediatric advanced life support: improving child survival in limited-resource settings. Lancet 381:256–265
Clarke DL, Kong VY, Handley J et al (2013) A concept paper: using the outcomes of common surgical conditions as quality metrics to benchmark district surgical services in South Africa as part of a systematic quality improvement programme. S Afr J Surg 51:84–86
Clarke DL, Furlong H, Laing GL et al (2013) Using a structured morbidity and mortality meeting to understand the contribution of human error to adverse surgical events in a South African regional hospital. S Afr J Surg 51:122–126
Nwomeh BC, Lowell W, Kable R et al (2006) History and development of trauma registry: lessons from developed to developing countries. World J Emerg Surg 1:32
Juillard CJ, Mock C, Goosen J et al (2009) Establishing the evidence base for trauma quality improvement: a collaborative WHO-IATSIC review. World J Surg 33:1075–1086
Juillard CJ, Stevens KA, Monono ME et al (2014) Analysis of prospective trauma registry data in Francophone Africa: a pilot study from Cameroon. World J Surg 38:2534–2542
Laing GL, Bruce JL, Aldous C et al (2014) The design, construction and implementation of a computerised trauma registry in a developing South African metropolitan trauma service. Injury 45:3–8
Acknowledgments
We wish to thank Manfred Amanya for electronic data entry and Nicholas Musinguzi, Trudy Poon and Hao Deng for statistical analysis.
Funding
This project was supported by funding from MGH Global Health, Massachusetts General Hospital, Boston, MA, USA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
We declare that we have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Tumusiime, G., Was, A., Preston, M.A. et al. The Quality and Utility of Surgical and Anesthetic Data at a Ugandan Regional Referral Hospital. World J Surg 41, 370–379 (2017). https://doi.org/10.1007/s00268-016-3714-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-016-3714-8