Abstract
Background
Esophageal epiphrenic diverticulum (ED) is usually secondary to a primary esophageal motility disorder, such as achalasia. Whereas the recommended surgical treatment includes esophageal myotomy and diverticulectomy, the outcome of patients in whom a myotomy without ED resection is performed is not known. The purpose of this study was to compare the outcome of ED patients who underwent ED resection and myotomy and those of ED patients who had a myotomy only.
Methods
Retrospective review of a prospective database. Thirteen ED patients had symptom evaluation, barium swallow, endoscopy, and esophageal high-resolution manometry (HRM). All patients underwent laparoscopic myotomy and Dor fundoplication. In six patients, the ED was resected (excised ED group), whereas in seven it was left in place (nonexcised ED group): in three because it was small and in four for technical reasons.
Results
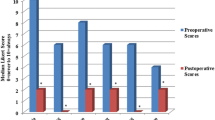
Preoperatively all patients had dysphagia and 85 % had regurgitation. The mean preoperative Eckardt score was 6.5 ± 2.1 in excised ED group and 6.6 ± 3.3 in nonexcised ED group (p = 0.95). HRM showed type II esophageal achalasia in 85 % of patients. One excised ED group patient had a staple line leak (17 %). At a median follow-up of 2 years, the Eckardt score was 0 in excised ED group and 0.1 in nonexcised ED group (p = 0.56).
Conclusions
The results of this study showed that patients in whom a myotomy without ED resection was performed had resolution of their symptoms. These findings suggest that in patients with achalasia and ED the underlying motility disorder rather than the ED may be the cause of symptoms. Studies with a larger number of patients and a longer follow-up will determine the validity of this approach.

Similar content being viewed by others
References
Nehra D, Lord RV, Demeester TR et al (2002) Physiologic basis for the treatment of epiphrenic diverticulum. Ann Surg 235:346–354
Melman L, Quinlan J, Robertson B et al (2009) Esophageal manometric characteristics and outcomes for laparoscopic esophageal diverticulectomy, myotomy, and partial fundoplication for epiphrenic diverticula. Surg Endosc 23:1337–1341
Del Genio A, Rossetti G, Maffettone V et al (2004) Laparoscopic approach in the treatment of epiphrenic diverticula: long-term results. Surg Endosc 18:741–745
Tedesco P, Fisichella PM, Way LW et al (2005) Cause and treatment of epiphrenic diverticula. Am J Surg 190:902–905
Fernando HC, Luketich JD, Samphire J et al (2005) Minimally invasive operation for esophageal diverticula. Ann Thorac Surg 80:2076–2081
Varghese TK, Marshall B, Chang AC et al (2007) Surgical treatment of epiphrenic diverticula: a 30-year experience. Ann Thorac Surg 84:1801–1809
D’Journo XB, Ferraro P, Martin J et al (2009) Lower oesophageal sphincter dysfunction is part of the functional abnormality in epiphrenic diverticulum. Br J Surg 96:892–900
Zaninotto G, Portale G, Costantini M et al (2008) Long-term outcome of operated and unoperated epiphrenic diverticula. J Gastrointest Surg 12:1485–1490
Klaus A, Hinder RA, Swain J et al (2003) Management of epiphrenic diverticula. J Gastrointest Surg 7:906–911
Fumagalli Romario U, Ceolin M, Porta M et al (2012) Laparoscopic repair of epiphrenic diverticulum. Semin Thorac Cardiovasc Surg 24:213–217
Rossetti G, Fei L, del Genio G et al (2013) Epiphrenic diverticula mini-invasive surgery: a challenge for expert surgeons—personal experience and review of the literature. Scan J Surg 102:129–135
Herbella FA, Patti MG (2012) Modern pathophysiology and treatment of esophageal diverticula. Langenbecks Arch Surg 397:29–35
Müller A, Halbfass HJ (2004) Laparoscopic esophagotomy without diverticular resection for treating epiphrenic diverticulum in hypertonic lower esophageal sphincter. Chirurg 75:302–306
Bello B, Zoccali M, Gullo R et al (2013) Gastroesophageal reflux disease and antireflux surgery. What is the proper preoperative work-up? J Gastrointest Surg 17:14–20
Allaix ME, Dobrowolsky A, Patti MG (2014) Surgical treatment of esophageal achalasia. In: Fisichella PM, Soper NJ, Pellegrini CA, Patti MG (eds) Surgical management of benign esophageal disorders: The “Chicago Approach”. Springer-Verlag London, pp 155–164
Oelschlager BK, Chang L, Pellegrini CA (2003) Improved outcome after extended gastric myotomy for achalasia. Arch Surg 138:490–497
Rebecchi F, Giaccone C, Farinella E et al (2008) Randomized controlled trial of laparoscopic Heller myotomy plus Dor fundoplication versus Nissen fundoplication for achalasia. Ann Surg 248:1023–1030
Acknowledgements
The authors did not receive Grant support for the research.
Conflict of interest
The authors have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Allaix, M.E., Borraez Segura, B.A., Herbella, F.A. et al. Is Resection of an Esophageal Epiphrenic Diverticulum Always Necessary in the Setting of Achalasia?. World J Surg 39, 203–207 (2015). https://doi.org/10.1007/s00268-014-2770-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-014-2770-1