Abstract
Background
Few guidelines exist for the initial management of wounds in disaster settings. As wounds sustained are often contaminated, there is a high risk of further complications from infection, both local and systemic. Healthcare workers with little to no surgical training often provide early wound care, and where resources and facilities are also often limited, and clear appropriate guidance is needed for early wound management.
Methods
We undertook a systematic review focusing on the nature of wounds in disaster situations, and the outcomes of wound management in recent disasters. We then presented the findings to an international consensus panel with a view to formulating a guideline for the initial management of wounds by first responders and subsequent healthcare personnel as they deploy.
Results
We included 62 studies in the review that described wound care challenges in a diverse range of disasters, and reported high rates of wound infection with multiple causative organisms. The panel defined a guideline in which the emphasis is on not closing wounds primarily but rather directing efforts toward cleaning, debridement, and dressing wounds in preparation for delayed primary closure, or further exploration and management by skilled surgeons.
Conclusion
Good wound care in disaster settings, as outlined in this article, can be achieved with relatively simple measures, and have important mortality and morbidity benefits.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In naturally occurring and man-made disaster situations, wounds are a major source of morbidity and mortality. They place substantial demands on strained, disrupted, and often rudimentary and makeshift health services. Wounds tend to be contaminated by a variety of environmental organisms and foreign matter, with crushed and devitalized tissue providing a medium for bacterial growth and invasion. First responders are often not medically trained and, though well intentioned, the treatment they provide is often compromised by a misconception that wounds should be closed to enable them to heal [1]. Experienced surgeons know that poor early wound management is often complicated by more extensive infection and tissue necrosis requiring wide excision or amputation, and preventable systemic sepsis, gangrene, and mortality [2]. Safe and effective early management of wounds by first responders in a disaster setting can prevent complications and save limbs and lives, and both first responders and subsequent healthcare personnel should be clear about what this entails.
Disasters such as the 2004 Tsunami, Hurricane Katrina in 2005, and the 2010 Haiti earthquake, were all characterized, to greater or lesser degree, by remote location, overwhelming numbers of casualties, inadequate resources, over-burdened healthcare services, and inexperienced caregivers. Much has been written about the health consequences of these disasters in general. We aimed to systematically review the nature of wounds and outcomes of wound management in recent disasters, and we then convened an international consensus panel to consider these results and formulate a concise guideline for the initial wound management for first responders and non-expert healthcare providers. It was anticipated that a generic guideline could be widely distributed, discussed among members of relevant organisations, modified according to local needs where required, and put into practice in many types of clinical settings.
Methods
We searched Cochrane Library (Wiley), Cinahl (Ebscohost), Medline (Ovid), Embase (Elsevier), and WHO Guidelines with the key words “wounds,” “crush injuries,” “open fractures,” with related complications such as “infections,” “necrosis,” “tetanus.” These terms were combined with disaster-related key words such as “tsunami,” “cyclone,” “earthquake,” and “flood.” The search included articles published up to 1 September 2012. The searches were limited to English language publications and human studies. The present review excluded burns, military blast injury, high-velocity injury, and penetrating injury. The reference lists of included articles were searched for other potentially relevant publications. Each article was assessed independently by two reviewers.
We then collated results and presented them to a consensus meeting of experts in surgery and disaster medicine that was held at the Royal Australasian College of Surgeons in September 2012. The invited experts came from Australasia and the Pacific, North America, South East Asia, and the Indian subcontinent (Table 1). This group considered the review findings and discussed and sought agreement on a set of principles that were then presented for comment and critique to an International Symposium on the Global Burden of Surgical Disease involving 151 delegates. The present report presents the results of these deliberations and a proposed simple guideline.
Results
Our literature search yielded 2,894 articles for screening, from which 62 proved to be relevant, as shown in Fig. 1. Those articles described details of the nature of wounds, wound care, and outcomes from various major incidents, including earthquakes in Marmara, Turkey (1999), Pakistan (2005), Wenchuan, China (2008), Haiti (2010), and Christchurch, New Zealand (2011); terrorist bombings in Bali, Indonesia (2002); and the 2004 tsunami centred near Banda Aceh, Indonesia.
The nature of wounds
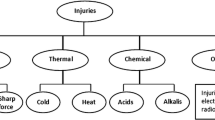
Depending on the nature of the catastrophe, extreme forces led to a spectrum of wounds variously characterized by multiple breaches of skin, deep puncture injuries [3], crushing and destruction of soft tissues, fractures of bone, and contamination with dirt, mud, seawater, sand, and debris, as well as feces and saliva [1, 4–8].
Of course many victims also had life-threatening respiratory or circulatory impairment or significant head and internal injuries. In earthquake-related disasters, 30 % of patients had head and neck injuries, and a quarter had significant chest, thoracolumbar spine, or spinal cord injuries, a third of whom required surgical interventions [9]. Musculoskeletal injuries are common, in earthquakes in particular, with the proportion of patients with closed fractures, sprains, open fractures, and neurovascular injury observed to be approximately 22, 6, 11–54, and 6 %, respectively [9].
Infection
High rates of infection occurred from contamination, tissue loss, inadequate or delayed wound cleaning and debridement, and premature wound closure [1, 6, 8]. For example, delayed initial wound care more than 24 h after injury and primary wound closure were independent predictors of secondary wound infection among tsunami victims [6]. Environmental pathogens and contaminated water used for cleaning wounds were the usual causes. Infections were often polymicrobial and included atypical bacteria and fungi [1, 7, 9], as detailed in Table 2.
The most common infective organisms following crush injuries were Gram-negative bacilli (67 %), Acinetobacter (36 %), Pseudomonas aeruginosa (21 %), Gram-positive cocci (17 %), and Enterobacter species (12 %) [10–12]. For example, following the 2008 earthquake in Wenchuan, China, 50 of 98 injured children studied developed wound infections [13], and Acinetobacter baumanii, Enterobacter cloacae, and P. aeruginosa were the pathogens most commonly isolated [13]. Prior to the earthquake, at the same institution, pediatric infections were more commonly caused by Escherichia coli and Staphylococcus aureus [13].
Among wounded tsunami survivors, it was estimated that half to two-thirds of wounds became infected, mostly within the first 72 h following the event [6], although many wounds were infected within the first 24 h [10]. Aeromonas was the single most common pathogen identified among tsunami survivors, accounting for over 20 % of infections [14]. Other, mostly Gram-negative bacteria [6] were also common, particularly E. coli and Klebsiella pneumoniae, as well as S. aureus, Proteus vulgaris, and P. aeruginosa [6].
Sepsis with or without necrotizing fasciitis was frequently seen following flood and tsunami wounds [10, 15], and it was associated with more than doubling of mortality (OR 2.45, 95 % confidence interval [CI] 1.52–3.96) [11].
Crush syndrome
Nine review articles and three descriptive studies each addressed crush syndrome, which is acute renal failure secondary to hypovolemia and rhabdomyolysis from muscle damaged at any of three different times: the time of the initial mechanical crushing force, during periods of ischemia, and during reperfusion [9, 16–18]. While skeletal muscle was thought to be relatively tolerant of ischemia for 2–4 h without permanent injury, it is likely that irreversible changes that limit functional recovery start to occur in as little as 1 h [18], especially when there is concurrent tissue damage and other injuries. Death often ensues due to hypovolemia and hyperkalemia [9].
Among earthquake survivors [3], the reported incidence of crush syndrome was 2–15 % [3, 9]. Entrapped time under the debris, multiple crush injuries, male gender, presence of infection, and creatinine kinase (CK) level were all predictive of acute renal failure [19]. Survival depended on limiting the degree of renal dysfunction and supporting organ function, and mortality was reported to be up to 48 % [9, 17, 20].
Management
The panel agreed on the principles of basic wound care in disasters, which are presented in Table 3. These highlight the importance of meticulous wound care even when resources and expertise are limited, recognizing that poorly managed wounds are associated with high mortality from sepsis and crush syndrome.
Initial patient management
Protocols for field-based triage and initial assessment of injured patients should prioritize identification and management of life-threatening conditions [21]. Early maneuvers to secure the airway, ensure adequate ventilation, and stop bleeding must take precedence over assessment and management of a non-bleeding extremity wound. Of course, wounds may compromise the airway, ventilation, cardiac function, or cause substantial hemorrhage, of which the latter may need to be addressed through application of direct pressure or a temporary tourniquet.
Basic wound assessment and management
Injuries to extremities should be addressed after initial assessment for life-threatening injuries and resuscitation has taken place [21]. Wounds must be carefully inspected, and assessment must be made for associated injuries, distal function, bone and soft tissue injury, and underlying neurovascular injury. In major earthquakes these types of injury occur in approximately 1 in 20 patients sustaining limb injury [9]. Assessment of the degree of contamination, devitalized tissue, presence of foreign bodies, and integrity of underlying structures may require wound extension and formal exploration, under anesthesia if it is available.
After adequate assessment, aggressive cleaning and debridement are required [6, 22]. Foreign bodies should be removed, and obvious embedded ones should be scrubbed before exploration, wound debridement, and removal [22] if possible. Devitalized tissue needs appropriate debridement by trimming or excising around the wound edge [22]. In one study of contaminated wounds, debridement was associated with reduced wound infection rates from 62.5 to 2 % [23].
Irrigation can be done with isotonic saline, distilled water, boiled and cooled water, dilute antiseptic solution, sterile water, or drinkable/potable tap water, with similar efficacy [24]. Untreated river water and seawater have high levels of contaminants and should not be used [25]. Dilute antiseptics, such as 1 % povidone–iodine or a 5 % solution of sodium benzyl penicillin have been shown to decrease infection rates and can be used in addition to water or normal saline [26–28].
Value of delayed primary closure
All primary and review articles confirmed that wounds sustained in disaster events are contaminated, especially when presentation is delayed, and that early primary wound closure causes high rates of serious wound infection eventually requiring much more extensive debridement and sometimes leading to the death of the patient [4, 6, 15, 29]. Such wounds should therefore be closed in a delayed fashion, which is associated with much lower infection rates. The only exception, for which initial wound closure has provided acceptably low rates of subsequent wound infection, is when primary closure followed wound assessment, meticulous debridement of all foreign material and devitalized tissue by an experienced surgeon within 6 h of injury [30].
Delayed primary closure consists of initial adequate debridement followed by wound dressing, careful wound reassessment at 48 h, repeat debridement and dressing if necessary, and, finally, closure 48 h or longer after initial inspection, but only if the wound is clean and free of foreign material and contaminated and devitalized tissue [31]. Simple closure techniques using strips, sutures, or staples can be employed if the wound edges can be brought together without undue tension. Delayed primary suturing gives similar cosmetic outcomes to immediate suture, even when closure is achieved 2–5 days after wounding. Wounds that cannot be closed without tension will need to be left open to heal by secondary intention or closed by skin graft or flap as appropriate.
Dressings
A clean, dry, absorbent dressing is usually sufficient to minimize ongoing contamination. Our search identified three systematic reviews [27, 32, 33], two randomized controlled trials [34, 35], and two other review articles [15, 36] that sought to determine whether any particular type of dressing was associated with superior outcomes compared to another.
It appears that an absorbent gauze dressing or saline-soaked gauze dressing and coverage with dry gauze are sufficient [15, 22, 34, 37]. Occlusive dressings have not been shown to further reduce infection, hasten healing, or be associated with less pain [34]. There is little evidence to support superior results over simple gauze dressings from the use of antibiotic or silver impregnated dressings and gels [33, 36, 38, 39], or antibiotic beads [40]. Medical-grade honey is reported to have peroxide and antibacterial activity, but little evidence of better outcomes exists to support its use [41, 42]. In patients with properly debrided wounds, there is also little evidence of reduction in mortality or severe infection with the additional use of advanced technologies, such as negative pressure wound therapies or hyperbaric oxygen, which may mitigate anaerobic infection by promoting a hyperoxic wound environment [9, 43]. There is some evidence that, where available, negative pressure wound therapies, which likely reduce tissue edema [44], allow earlier delayed primary closure [32, 35, 45]. However, such advanced technologies are unlikely to be available early on in the setting of a disaster when wounds are fresh.
Systemic antibiotics
While topical antibiotics have not been shown to significantly influence wound infection rates [38], systemic antibiotics play an adjunct role to proper initial wound care and delayed primary closure [21, 46]. Their availability at the time of initial wound care is the main limitation for prophylaxis. Various prophylactic regimens have been recommended, ranging from a single dose of beta-lactam penicillin in patients with mildly contaminated wounds [22] or in operations for the treatment of closed fracture [47], to longer durations in wounds affecting the hands [21] and feet, as well as in all open fractures [25]. Antibiotic use has had protective effects against early infection in open fractures of the limb [46]. In established infections, antibiotics are an essential component of wound care.
A variety of oral and parenteral agents have been recommended. Initial prophylaxis with fusidic acid, flucloxacillin, or erythromycin were generally effective in preventing skin and soft tissue infections [48–50]. However, antibiotic resistance is prevalent, particularly to commonly used agents such as amoxyl–clavulanate, ceftriaxone, and cloxacillin [6, 13]. More infecting bacteria were susceptible to aminoglycoside (gentamicin, amikacin), piperacillin–tazobactam, third and fourth generation cephalosporins, quinolones (ciprofloxacin), imipenem, and meropenem [3, 8, 12, 14, 25]. Broad-spectrum antibiotic prophylaxis has been shown to decrease infection rates [22, 23] and therefore benefit wound healing [6]. Similarly, if initial antimicrobial agents are ineffective, broadening therapy with quinolones such as ciprofloxacin and gentamicin to cover Gram-negative bacteria is indicated [25].
Tetanus prophylaxis
Tetanus prophylaxis or mass vaccination campaigns have been rolled out in disaster settings [9, 21], and have shown that unnecessary vaccination is unlikely to cause harm [51]. Tetanus-prone wounds are those that are stellate in shape or longer than 1 cm, more than 6 h old, that contain devitalized tissue or gangrene, or are contaminated with dirt, saliva, or feces [5]. Avulsion injuries are also prone to tetanus. Proper initial wound care and debridement are critical for tetanus prevention [51].
The need for post-exposure prophylaxis for tetanus depends on each patient’s previous immunization status. When immunization status is unknown, or if the patient has received fewer than three previous doses of tetanus toxoid, both tetanus toxoid and tetanus immunoglobulin should be administered. A second dose of toxoid should be given within the next 2 months, followed by a third dose in the following 6–12 months [5, 50, 51]. In cases of completed immunization within 5 years, it appears unnecessary to give either tetanus toxoid or immunoglobulin. If completed immunization was longer than 5 years before injury, patients should be given a single dose of tetanus toxoid [5, 50, 51]. Pediatric patients (under 7 years of age), can be given the diphtheria, pertussis, tetanus (DPT) vaccine instead of tetanus toxoid [5, 51].
Documentation
Although none of the articles reviewed made specific reference to the need for appropriate documentation, the panel regarded clear, concise documentation of wound management to be crucial to monitoring and follow-up of each wound.
Details to be recorded include (1) the mechanism of injury (e.g., penetrating, laceration, abrasion, blast); (2) a description of the wound, including the location of the injury on the body; (3) the wound size, depth, margins, and base, and any neurovascular structures involved; and (4) any management that has been undertaken and any further action required, making clear the date and time of planned wound review.
Special situations (Table 4)
Entrapment and extrication
The entrapped victim presents the concurrent challenges of time-critical life-saving interventions and freeing the victim, followed by prevention and minimization of the harmful systemic effects of crush injury and the management of wounds and other injuries. Primary management of the entrapped victim consists of early fluid administration and coordinated extrication; however, if an entrapped limb is preventing early extrication, then amputation at the scene may be a life-saving measure [18, 44].
While limb amputation before release of the crushing force may prevent the sequelae of the reperfusion syndrome and minimize the systemic insult, it is also associated with substantial morbidity and should be done only if other options for preserving crushed limbs have been exhausted [18]. Surgical expertise is often required to remove and safely extricate an injured survivor from the scene of a disaster [9, 16, 21, 44, 52], and medical expertise is often needed immediately afterwards to manage the complications of prolonged entrapment and reperfusion injury.
Crush injury, compartment syndrome, and avoidance of fasciotomy
Crushing of a limb often leads to swelling, painful tense compartments, altered sensation, and sometimes absent distal pulses. In civilian settings a limb with these signs would usually be treated with resuscitation, limb immobilization, fracture fixation, and fasciotomy to reduce compartment pressures and restore capillary circulation.
In disaster settings, it is unclear whether the benefits of fasciotomy outweigh the risks associated with further wounds, which may act as a portal for infection of underlying devitalized muscle. In one study of earthquake victims, 81 % of fasciotomies became infected, and fasciotomy was therefore a significant factor in sepsis (p < 0.001) and mortality (p < 0.0001 [9]).
A reasonable strategy that balances potential benefits and harms in limbs with viable musculature, as indicated by responsiveness to mechanical or electrical stimulation, is for fasciotomy to be performed only if intra-compartment pressures are greater than 40 mmHg [17] or distal pulses are absent [18, 44]. Salvage of muscle is likely to be futile in limbs that have been crushed for a prolonged period and show evidence of devitalized muscle by lack of responsiveness to stimulation. In this situation, debridement of devitalized tissue should be the priority.
Systemic effects of crush injury, especially rhabdomyolysis, should be expected [19]. A urine dipstick to detect myoglobin and subclinical rhabdomyolysis can be useful in the field to triage patients; however, the serum CK level is a more sensitive biochemical marker once pathology services are available [9]. A serum CK level greater than 5,000 U/L has been shown to be the best predictor of acute renal failure in crush-injured patients, with mortality in the range of 14–48 % [9]. Urgent treatment and critical care monitoring are almost always needed if the serum CK level reaches 20,000 U/L [16]. Electrolyte abnormalities are common, and hyperkalemia and hypovolemia can be fatal, so serum potassium levels, CK level, cardiac status, and arterial pH should be measured three to fours times daily in the first few days [9, 17, 18].
Early intravenous fluid administration prior to extrication can help prevent acute renal failure due to rhabdomyolysis [9, 17, 20]. Treatment of crush syndrome usually requires early aggressive hydration and forced diuresis (urine output of 100–200 mL/h), alkalinization of urine (pH 6.5 or more), and maintenance of arterial pH <7.5 [16, 20, 53]. Hemodialysis, if available, will often be initiated if the serum creatinine is greater than 1.5 mg/dL [16, 53].
Fractures
Basic principles of fracture management should be followed, which include temporary splinting to minimize pain and bleeding and prevent further soft tissue or neurovascular injury during transportation to more specialized services [53]. Patients with open fractures should receive early systemic antibiotic treatment and tetanus vaccination [53]. External fixation is often a mainstay of early management of the mangled limb, allowing wounds and soft tissues to be properly assessed and managed even when definitive fracture fixation is unavailable [54]. Early referral should be planned to a facility capable of managing fractures and other needs of the victims.
Delayed amputation
Other than as a life-saving procedure to extricate a trapped person where other options have been exhausted, amputation of a mangled or devitalized limb should only be performed by a suitably qualified person after careful evaluation of the limb and the patient [9, 16, 21, 44, 52]. Aids to assessment, such as the Mangled Extremity Severity Score (MESS), have been developed to guide decision making [52]. The main indications for amputation have been irreparable vascular injury, completion of partial amputation and, as a last resort in patients with severe soft tissue damage, with or without fractures and deteriorating renal and cardio-respiratory function, as well as overwhelming sepsis [21].
Wounds of the head, neck, face, hands, and feet
In disaster settings wounds on the face, neck, hands, and feet should be managed according to the same principles, as they have early wound infection rates exceeding 50 % [2, 4, 37, 54, 56].
Although it may be technically challenging to treat injuries to these sites, adequate debridement and delayed primary closure are still key to preventing severe wound infection. In one series the infection rates among patients who had and had not undergone wound debridement were 2 and 62.5 %, respectively [23]. Where there are cosmetically challenging wounds, early referral to an experienced surgeon may reduce the risk of eventual disfigurement or loss of function. In any wounds of the head, neck, or face early consideration needs to be given to the possibility of brain or airway injury.
Discussion
Through this systematic review we provide an evidence-based overview of the clinical challenges of managing wounds among survivors of natural and man-made disasters. We also provide evidence of suboptimal wound management in recent disasters, noting that these wounds could have been better managed with adherence to some key principles. The review and the deliberations of the international panel have clarified and redefined these key principles, distilled from a variety of sources, that together comprise the necessary aspects of good wound care in austere environments. It is anticipated that adherence to these practices will minimize preventable deaths and improve the outcomes and quality of life among survivors.
The most critical step is avoiding premature closure of contaminated and inadequately cleaned and debrided wounds. Simple cleaning, dressing, and review of wounds at 48 h allows identification and adequate management of the vast majority of wound infections that could otherwise be life-threatening or limb-threatening. When the open wound is re-inspected, the presence of erythema, purulent exudate, necrotic core, and tissue edema are all signs that the wound should not yet be closed, that further cleaning and debridement should performed, and that antibiotic therapy should be considered. The wound should then be redressed and inspected another 48 h later.
The review and deliberations also highlighted the challenges faced in standardizing these practices. In disaster settings health care services are usually overburdened, first responders are often inexperienced in wound care, and resources are mostly inadequate. Experienced surgeons who can manage complex wounds are usually a scarce resource, and crucial strategies, such as delaying wound closure, may be unfamiliar to those immediately responsible for care of the victims.
The consensus panel acknowledged that promoting practice improvements among dispersed, relatively unskilled personnel working at unpredictable times in austere environments with few of the usual clinical resources is a very challenging task. We regarded a wide dissemination strategy and endorsement by relevant clinicians and their representative organizations to be essential. With this in mind, our panel developed a simple generic poster that provides guidelines for wound care in disaster settings (Fig. 1). It is anticipated that the poster would be useful for promoting discussion about optimal wound management, for education, and for field-based guidance in the acute aftermath of a disaster. It is presented as a simple A, B, C, D, E, F, G aide de memoir for easy reference and to facilitate recollection. This poster can be modified for local use if necessary, and included in disaster management equipment packs, and in emergency care facilities during disaster situations. It was launched at the joint meeting of the RACS International Committee and the Alliance for Surgery and Anesthesia Presence at the Royal Australasian College of Surgeons and Australian and New Zealand College of Anaesthetists Annual Scientific Congress in Singapore on 5 May 2014, and it is likely to be made available for download from many surgical college websites.
References
Prasartritha T, Tungsiripat R, Warachit P (2008) The revisit of 2004 tsunami in Thailand: characteristics of wounds. Int Wound J 5:8–19
Department of Violence and Injury Prevention and Disability, World Health Organization Prevention and management of wound infection, pp 1–3
Kang M, Xie Y, Mintao C et al (2009) Antimicrobial susceptibility of clinical isolates from earthquake victims in Wenchuan. Clin Microbiol Infect 15:87–92
Edsander-Nord Å (2008) Wound complications from the tsunami disaster: a reminder of indications for delayed closure. Eur J Trauma Emerg Surg 34:457–464
Afshar M, Raju M, Ansell D et al (2011) Narrative review: tetanus—a health threat after natural disasters in developing countries. Ann Intern Med 154:329–335
Doung-Ngern P, Vatanaprasan T, Chungpaibulpatana J et al (2009) Infections and treatment of wounds in survivors of the 2004 tsunami in Thailand. Int Wound J 6:347–354
Kiani QH, Amir M, Ghazanfar MA et al (2009) Microbiology of wound infections among hospitalised patients following the 2005 Pakistan earthquake. J Hosp Infect 73:71–78
Hiransuthikul N, Tantisiriwat W, Lertutsahakul K et al (2005) Skin and soft-tissue infections among tsunami survivors in southern Thailand. Clin Infect Dis 41:e93–e96
Bartels SA, VanRooyen MJ (2012) Medical complications associated with earthquakes. Lancet 379:748–757
Kespechara K, Koysombat T, Pakamol S et al (2005) Infecting organisms in victims from the tsunami disaster: experiences from Bangkok Phuket Hospital, Thailand. Int J Disaster Med 3:66–70
Keven K, Ates K, Sever MS et al (2003) Infectious complications after mass disasters: the Marmara earthquake experience. Scand J Infect Dis 35:110–113
Kazancioglu R, Cagatay A, Calangu S et al (2002) The characteristics of infections in crush syndrome. Clin Microbiol Infect 8:202–206
Ran Y, Ao X, Liu L et al (2010) Microbiological study of pathogenic bacteria isolated from paediatric wound infections following the 2008 Wenchuan earthquake. Scand J Infect Dis 42:347–350
Janda JM, Abbott SL (2010) The genus Aeromonas: taxonomy, pathogenicity, and infection. Clin Microbiol Rev 23:35–73
Llewellyn M (2006) Floods and tsunamis. Surg Clin North Am 86:557–578
Gonzalez D (2005) Crush syndrome. Crit Care Med 33(1 Suppl):S34–S41
Efstratiadis G, Voulgaridou A, Nikiforou D et al (2007) Rhabdomyolysis updated. Hippokratia 11:129–137
Jagodzinski NA, Weerasinghe C, Porter K (2010) Crush injuries and crush syndrome—a review. Part 1: The systemic injury. Trauma 12:69–88
Hu Z, Zeng X, Fu P et al (2012) Predictive factors for acute renal failure in crush injuries in the Sichuan earthquake. Injury 43:613–618
Gunal AI, Celiker H, Dogukan A et al (2004) Early and vigorous fluid resuscitation prevents acute renal failure in the crush victims of catastrophic earthquakes. J Am Soc Nephrol 15:1862–1867
Wolfson N (2012) Amputations in natural disasters and mass casualties: staged approach. Int Orthop 36:1983–1988
Department of Health and Human Services, Centers for Disease Control and Prevention (2005) Emergency wound management of healthcare professionals, pp 1–2
Edlich RF, Kenney JG, Morgan RF et al (1986) Antimicrobial treatment of minor soft tissue lacerations: a critical review. Emerg Med Clin North Am 4:561–580
Fernandez R, Griffiths R (2012) Water for wound cleansing. Cochrane Database Syst Rev 2:CD003861
Okamura J, Kai T, Hayati Z et al (2009) Antimicrobial therapy for water-associated wound infections in a disaster setting: Gram-negative bacilli in an aquatic environment and lessons from Banda Aceh. Prehosp Disaster Med 24:189–196
Gravett A, Sterner S, Clinton JE et al (1987) A trial of povidone-iodine in the prevention of infection in sutured lacerations. Ann Emerg Med 16:167–171
Vermeulen H, Westerbos SJ, Ubbink DT (2010) Benefit and harm of iodine in wound care: a systematic review. J Hosp Infect 76:191–199
Lindsey D, Nava C, Marti M (1982) Effectiveness of penicillin irrigation in control of infection in sutured lacerations. J Trauma 22:186–189
Langworthy MJ, Smith JM, Gould M (2004) Treatment of the mangled lower extremity after a terrorist blast injury. Clin Orthop Relat Res 422:88–96
Atesalp AS, Erler K, Gür E et al (1999) Below-knee amputations as a result of land-mine injuries: comparison of primary closure versus delayed primary closure. J Trauma 47:724–727
Eliya MC, Banda GW (2011) Primary closure versus delayed closure for non bite traumatic wounds within 24 hours post injury. Cochrane Database Syst Rev 9:CD008574
Ubbink DT, Westerbos SJ, Nelson EA et al (2008) A systematic review of topical negative pressure therapy for acute and chronic wounds. Br J Surg 95:685–692
Vermeulen H, van Hattem JM, Storm-Versloot MN, et al (2007) Topical silver for treating infected wounds. Cochrane Database of Syst Rev 1:CD005486
Ubbink DT, Vermeulen H, Goossens A et al (2008) Occlusive vs gauze dressings for local wound care in surgical patients: a randomized clinical trial. Arch Surg 10:950–955
Perez D, Bramkamp M, Exe C et al (2010) Modern wound care for the poor: a randomized clinical trial comparing the vacuum system with conventional saline-soaked gauze dressings. Am J Surg 199:14–20
Storm-Versloot MN, Vos CG, Ubbink DT, et al (2010) Topical silver for preventing wound infection. Cochrane Database of Syst Rev 3:CD006478
World Health Organisation (2005) Wound Management. WHO, Geneva. http://apps.who.int/medicinedocs/documents/s17298e/s17298e.pdf. Accessed 10 Dec 2013
Hood R, Shermock KM, Emerman C (2004) A prospective, randomized pilot evaluation of topical triple antibiotic versus mupirocin for the prevention of uncomplicated soft tissue wound infection. Am J Emerg Med 22:1–3
Katnimit C, Nualsrithong P, Teabput S (2006) The management of wounds caused by the 2004 tsunami. World Council Enterostomal Therapists J 26:38–41
Warner M, Henderson C, Kadrmas W et al (2010) Comparison of vacuum-assisted closure to the antibiotic bead pouch for the treatment of blast injury of the extremity. Orthopedics 33:77–82
Jull Andrew B, Rodgers A, Walker N (2008) Honey as a topical treatment for wounds. Cochrane Database Syst Rev 4:CD005083
Moore OA, Smith LA, Campbell F et al (2001) Systematic review of the use of honey as a wound dressing. BMC Complement Altern Med 1:2
Wang C, Schwaitzberg S, Berliner E et al (2003) Hyperbaric oxygen for treating wounds: a systematic review of the literature. Arch Surg 138:272–279
Jagodzinski NA, Weerasinghe C, Porter K (2010) Crush injuries and crush syndrome—a review. Part 2: The local injury. Trauma 12:133–148
Health Quality Ontario (2006) Negative pressure wound therapy: an evidence-based analysis. Ont Health Technol Assess Ser 6:1–38
Gosselin RA, Roberts I, Gillespie WJ (2004) Antibiotics for preventing infection in open limb fractures. Cochrane Database Syst Rev 1:CD003764
Slobogean GP, Kennedy SA, Davidson D et al (2008) Single- versus multiple-dose antibiotic prophylaxis in the surgical treatment of closed fractures: a meta-analysis. J Orthop Trauma 22:264–269
Morris CDE, Talbot DT (2000) A comparison of fusidic acid tablets and flucloxacillin capsules in skin and soft tissue infection. J Drug Assess 3:33–46
Wall AR, Menday AP (2000) Fusidic acid and erythromycin in the treatment of skin and soft tissue infection: a double blind study. J Drug Assess 3:63–76
Howdieshell TR, Heffernan D, Dipiro JT (2006) Surgical infection society guidelines for vaccination after traumatic injury. Surg Infect 7:275–303
Chapman LE, Sullivent EE, Grohskopf LA et al (2008) Postexposure interventions to prevent infection with HBV, HCV, or HIV, and tetanus in people wounded during bombings and other mass casualty events—United States, 2008: recommendations of the Centers for Disease Control and Prevention and Disaster Medicine and Public Health Preparedness. Disaster Med Public Health Prep 2:150–165
Helfet DL, Howey T, Sanders R et al (1990) Limb salvage versus amputation. Preliminary results of the Mangled Extremity Severity Score. Clin Orthop Relat Res 256:80–86
DePalma RG, Burris DG, Champion HR et al (2005) Current concepts: blast injuries. N Engl J Med 352:1335–1342
Johnson LM, Travis AR (2005) In the wake: tsunami pathology—then and now, Krabi Province, southern Thailand. Int J Disaster Med 14:61–65
Liu L, Tan G, Luan F et al (2012) The use of external fixation combined with vacuum sealing drainage to treat open comminuted fractures of tibia in the Wenchuan earthquake. Int Orthop 36:1441–1447
Liu J, Ma L, You C (2012) Analysis of scalp wound infections among craniocerebral trauma patients following the 2008 Wenchuan earthquake. Turk Neurosurg 22:27–31
Acknowledgments
The members of the Wound Management in Disaster Settings Consensus Meeting are listed in Table 2. P.W. was supported by a Weary Dunlop Boon Pong Fellowship of the Royal College of Surgeons of Thailand and the Royal Australasian College of Surgeons. R.L.G. was supported by a Practitioner Fellowship from the Australian National Health and Medical Research Council. The development and dissemination of the Wound Care in Disaster Settings guidelines has been supported by the Royal Australasian College of Surgeons through its International Committee.
Conflict of interest
The authors declare they have no conflicts of interest in relation to this paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made.
The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this licence, visit https://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wuthisuthimethawee, P., Lindquist, S.J., Sandler, N. et al. Wound Management in Disaster Settings. World J Surg 39, 842–853 (2015). https://doi.org/10.1007/s00268-014-2663-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-014-2663-3