Abstract
Background
The aim of this study was to compare postoperative outcome and long-term results after management of liver hydatid cysts (LHC) by subadventitial cystectomy (SC) and resection of the protruding dome (RPD) in two tertiary liver surgery centers.
Methods
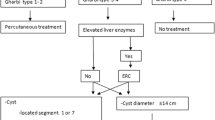
Medical records of 52 patients who underwent SC in one center, and 27 patients who underwent RPD in another center between 1991 and 2011 were reviewed. Patients underwent long-term follow-up, including serology tests and morphological examinations.
Results
Postoperative mortality was nil. The rate of severe morbidity was 7.7 and 22 % (p = 0.082), while the rate of serological clearing-up was 20 and 13.3 % after SC and RPD, respectively (p = 1.000). After a mean follow-up of 41 months (1–197), four patients developed a long-term cavity-related complication (LTCRC) after RPD (including one recurrence) and none after SC (p = 0.012). All LTCRCs occurred in patients with hydatid cysts located at the liver dome; three required an invasive procedure by either puncture aspiration injection re-aspiration (N = 1) or repeat surgery (N = 2).
Conclusions
RPD exposes to specific LTCRC, especially when hydatid cysts are located at the liver dome, while SC allows ad integrum restoration of the operated liver. Therefore, SC should be considered as the standard surgical treatment for LHC in experienced hepato-pancreato-biliary centers.



Similar content being viewed by others
References
Brunetti E, Kern P, Vuitton DA, Writing Panel for the WHO-IWGE (2010) Expert consensus for the diagnosis and treatment of cystic and alveolar echinococcosis in humans. Acta Trop 114:1–16
WHO Informal Working Group (2003) International classification of ultrasound images in cystic echinococcosis for application in clinical and field epidemiological settings. Acta Trop 85:253–261
Dziri C, Haouet K, Fingerhut A (2004) Treatment of hydatid cyst of the liver: where is the evidence? World J Surg 28:731–736. doi:10.1007/s00268-004-7516-z
Dervenis C, Delis S, Avgerinos C et al (2005) Changing concepts in the management of liver hydatid disease. J Gastrointest Surg 9:869–877
Buttenschoen K, Carli Buttenschoen D (2003) Echinococcus granulosus infection: the challenge of surgical treatment. Langenbecks Arch Surg 388:218–230
Yüksel O, Akyürek N, Sahin T et al (2008) Efficacy of radical surgery in preventing early local recurrence and cavity-related complications in hydatic liver disease. J Gastrointest Surg 12:483–489
Prousalidis J, Kosmidis CH, Fahantidis E et al (2004) Surgical treatment of multiple cystic echinococcosis. HPB (Oxford) 6:110–114
Avgerinos ED, Pavlakis E, Stathoulopoulos A et al (2006) Clinical presentations and surgical management of liver hydatidosis: our 20 year experience. HPB (Oxford) 8:189–193
Peng X, Zhang S, Niu JH (2002) Total subadventitial cystectomy for the treatment of 30 patients with hepatic hydatid cyst. Chin J Gen Surg 17:529–530
Dziri C, Haouet K, Fingerhut A, Zaouche A (2009) Management of cystic echinococcosis complications and dissemination: where is the evidence? World J Surg 33:1266–1273. doi:10.1007/s00268-009-9982-9
Kayaalp C, Bostanci B, Yol S, Akoglu M (2003) Distribution of hydatid cysts into the liver with reference to cystobiliary communications and cavity-related complications. Am J Surg 185:175–179
American Society of Anesthesiologists (1963) New classification of physical status. Anesthesiology 24:111
Peng X, Li J, Wu X et al (2006) Detection of osteopontin in the pericyst of human hepatic Echinococcus granulosus. Acta Trop 100:163–171
Cirenei A, Bertoldi I (2001) Evolution of surgery for liver hydatidosis from 1950 to today: analysis of a personal experience. World J Surg 25:87–92. doi:10.1007/s002680020368
Akbulut S, Senol A, Sezgin A et al (2010) Radical vs conservative surgery for hydatid liver cysts: experience from single center. World J Gastroenterol 16:953
Tagliacozzo S, Miccini M, Amore Bonapasta S (2011) Surgical treatment of hydatid disease of the liver: 25 years of experience. Am J Surg 201:797–804
Chautems R, Bühler LH, Gold B et al (2005) Surgical management and long-term outcome of complicated liver hydatid cysts caused by Echinococcus granulosus. Surgery 137:312–316
Daradkeh S, EL-Muhtaseb H, Farah G et al (2006) Predictors of morbidity and mortality in the surgical management of hydatid cyst of the liver. Langenbecks Arch Surg 392:35–39
Akcan A, Sozuer E, Akyildiz H et al (2010) Predisposing factors and surgical outcome of complicated liver hydatid cysts. World J Gastroenterol 16:3040–3048
Saylam B, Coşkun F, Demiriz B et al (2013) A new and simple score for predicting cystobiliary fistula in patients with hepatic hydatid cysts. Surgery 153:699–704
Yagci G, Ustunsoz B, Kaymakcioglu N et al (2005) Results of surgical, laparoscopic, and percutaneous treatment for hydatid disease of the liver: 10 years experience with 355 patients. World J Surg 29:1670–1679. doi:10.1007/s00268-005-0058-1
Atahan K, Küpeli H, Deniz M et al (2011) Can occult cystobiliary fistulas in hepatic hydatid disease be predicted before surgery? Int J Med Sci 8:315–320
Junghanss T, da Silva AM, Horton J et al (2008) Clinical management of cystic echinococcosis: state of the art, problems, and perspectives. Am J Trop Med Hyg 79:301–311
Smego RA, Sebanego P (2005) Treatment options for hepatic cystic echinococcosis. Int J Infect Dis 9:69–76
Kouraklis G, Dosios T, Glinavou A et al (2005) Myoplasty versus omentoplasty in the surgical treatment of hydatidosis of the liver dome. Langenbecks Arch Surg 390:42–46
El Malki HO, El Mejdoubi Y, Souadka A et al (2010) Does primary surgical management of liver hydatid cyst influence recurrence? J Gastrointest Surg 14:1121–1127
Dziri C, Paquet JC, Hay JM et al (1999) Omentoplasty in the prevention of deep abdominal complications after surgery for hydatid disease of the liver: a multicenter, prospective, randomized trial. French Associations for Surgical Research. J Am Coll Surg 188:281–289
Bildik N, evik A, Altinta M et al (2007) Efficacy of preoperative albendazole use according to months in hydatid cyst of the liver. J Clin Gastroenterol 41:312–316
Cobo F, Yarnoz C, Sesma B et al (1998) Albendazole plus praziquantel versus albendazole alone as a pre-operative treatment in intra-abdominal hydatisosis caused by Echinococcus granulosus. Trop Med Int Health 3:462–466
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications. Ann Surg 240:205–213
Funding
No grant support was received for the research reported.
Conflicts of interest
The authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mohkam, K., Belkhir, L., Wallon, M. et al. Surgical Management of Liver Hydatid Disease: Subadventitial Cystectomy versus Resection of the Protruding Dome. World J Surg 38, 2113–2121 (2014). https://doi.org/10.1007/s00268-014-2509-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-014-2509-z