Abstract
Background
Capsular contracture is one of the most common complications after breast surgery involving silicone implants. The most likely cause of this condition is biofilm formation. In this study, the efficacy of local antibiotherapy against biofilm formation on implant surfaces was investigated.
Methods
Thirty-six rats were divided into six groups. Three pockets were created on the dorsum of each rat, and 1 × 2 cm implant surface samples from smooth, polyurethane and textured implants were randomly placed into pockets. All samples were inoculated with staphylococcus epidermidis. In groups 1-2-3, inoculated samples were placed into the pockets and removed after 1, 6 and 24 h, respectively. In groups 4-5-6, inoculated samples immersed with rifamycin were placed and removed after 1, 6 and 24 h, respectively. Bacterial load was measured with plate count method.
Results
Bacterial load was lower in groups 4-5-6 than in groups 1-2-3 (p < 0.05). In groups 4-5-6, bacterial load was lower for polyurethane than for textured surfaces at all time points (1, 6 and 24 h; p < 0.05). Again, in groups 4-5-6, bacterial load was lower for smooth than for textured surfaces at 24 h (p < 0.05). In groups 4-5-6, bacterial load was lower for polyurethane than for smooth surfaces at all time points, but difference was not statistically significant (1, 6 and 24 h; p < 0.05).
Conclusion
The results suggest that local antibiotic therapy was effective in reducing the bacterial load on all surfaces. The effectiveness of local rifamycin on the polyurethane surface was higher, and the duration of activity was longer than other surfaces.
No Level Assigned
This journal requires that authors assign a level of evidence to each article. For a full description of these evidence-based medicine ratings, please refer to the Table of contents or the online Instructions to Authors www.springer.com/00266.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Background
Capsular contracture is one of the most common complications after breast augmentation or reconstruction with silicone implants [1,2,3]. One of the most common etiological factors leading to capsular contracture is chronic subclinical infection created by the biofilm layer [4,5,6,7,8,9,10]. The risk of breast-implant-associated anaplastic large cell lymphoma (BIA-ALCL), which has become a hot topic during the last decade, has also been shown to be related to the structure of the implant surface, biofilm formation on the implant surface and genetic predisposition [11,12,13].
Some in vivo animal studies have shown the strong relationship between biofilm formation and capsular contracture [14,15,16,17]. Therefore, it is recommended to rinse silicone implants with antibiotic solution prior to insertion into the surgical pocket [18, 19]. Furthermore, it has been demonstrated that the surface properties of the implants are important in the development of capsular contracture [20,21,22,23,24,25]. Previous long-term studies have reported that the rate of capsular contracture in polyurethane-coated implants was 15% less than those with textured surfaces and 30% less than those with smooth surfaces [26,27,28].
There are no studies in the literature comparing the effects of local antibiotic therapy on all three implant surfaces available in the market, which are smooth, textured and polyurethane surfaces. In our research, we planned to perform an in vivo animal study to measure the efficacy and duration of local antibiotic therapy, which is used to fight the formation of a biofilm layer, on implants with different surface properties.
Objectives
Hypothesis of the study: Silicone implant surfaces have various physical properties, and microorganisms can remain attached to different surfaces at variable rates. Inserting silicone implants after rinsing with an antibiotic solution will reduce biofilm formation and thus the incidence of capsular contracture and BIA-ALCL. The holding capacity and duration of such an antibiotic solution and therefore the effectiveness of such antibiotics vary from surface to surface. Due to their hydrophilic nature and spongy structure, polyurethane-coated implants, which have higher liquid retention capacity as compared to silicone surfaces, will keep the antibiotic solution on their surfaces for a longer period. Therefore, the effectiveness on polyurethane surfaces should be higher as compared to implants with smooth and textured surfaces.
The main purpose of this study is to reveal the behavioral characteristics of different implant surfaces after bacterial contamination and the effectiveness of local antibiotic treatment after bacterial contamination at different timepoints in a standard experimental setting.
Materials and Methods
Experimental Animals
This study was carried out on 36 Wistar Albino female rats. Each weighed approximately 250 g. No other inclusion and exclusion criteria were applied.
Study Design
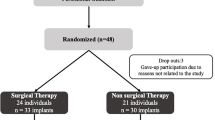
All surgical procedures were performed by Karakas E, M.D. (EK) for all animals. A total of six groups, three experimental and three control groups consisting of six animals each, were created.
Experimental Procedure
The implant surface materials used in this study were obtained from three implants from two companies: the polyurethane implant surface (1 × 2 cm) was obtained from Microthane® implants, manufactured by Polytech Health and Aesthetics (Dieburg,Germany). Microthane® is a polyurethane foam-coated implant surface with an average thickness of 1500 µ and a surface area of > 300 mm2. On the other hand, the textured implant surface (1 × 2 cm) was obtained from Siltex® implants, and the smooth implant surface (1 × 2 cm) was obtained from the smooth implants manufactured by Mentor Worldwide LLC (California, USA) (Figure 1). Siltex® is a microtextured implant surface with a surface area of 100–200 mm2 that is textured using negative contact imprinting technique by pressing the uncured silicone mandrel into polyurethane foam. [28,29,30,31]
Smooth (S), polyurethane (P), textured (T) implant surface (without antibiotic) (Above left). Smooth (S), polyurethane (P) and textured (T) implant surfaces (with antibiotic) (Above right). Preoperative incision markings for submuscular pockets (Below left). Implant surface are placed in the submuscular pocket with sterile forceps (Below right)
The three implant surface materials were placed on the dorsum of each rat under aseptic conditions. In all rats, a submuscular pocket was prepared using the same technique. After cleansing and covering, three different and disconnected pockets were prepared, one with a vertical incision of 1 cm from the nape and the other two with oblique incisions of 1 cm under both scapulae (Fig. 1). It was randomly decided which implant to be placed in which pocket in all animals. Randomization was done with a random number generating computer software.
In the control groups, the implant materials with three different surfaces were kept in a Staphylococcus epidermidis (S. epidermidis) culture (107 CFU/ml) for 24 h, which has been clinically proven to form a biofilm layer. In the experimental groups, the implant materials with three different surfaces were first kept in an S. epidermidis culture (107 CFU/ml) for 24 h and then inserted in a sterile solution containing 250 mg/3 ml of rifamycin for 5 min. Following the inoculation process, the implant surface materials were placed in the submuscular pockets, using sterile forceps (Fig. 1).
Each group included six rats, and the groups were composed as follows: Study groups are summarized in Table 1.
Group 1 (Control group—1st h): Three different implant surfaces were placed in the submuscular pockets after inoculation with S. epidermidis and removed 1 h after insertion.
Group 2 (Control group—6th h): Three different implant surfaces were placed in the submuscular pockets after inoculation with S. epidermidis and removed 6 h after insertion.
Group 3 (Control group—24th h): Three different implant surfaces were placed in the submuscular pockets after inoculation with S. epidermidis and removed 24 h after insertion.
Group 4 (Experimental group—Local antibiotic, 1st h): Three different implant surfaces were placed in the submuscular pockets after inoculation with S. epidermidis, kept in rifamycin solution for 5 min and removed 1 h after insertion.
Group 5 (Experimental group—Local antibiotic, 6th h): Three different implant surfaces were placed in the submuscular pockets after inoculation with S. epidermidis, kept in rifamycin for 5 min and then removed 6 h after insertion.
Group 6 (Experimental group—Local antibiotic, 24th h): Three different implant surfaces were placed in the submuscular pockets after inoculation with S. epidermidis, kept in rifamycin for 5 min and then removed 24 h after insertion.
Preparation and Administration of Bacterial Inoculum
The biofilm-positive RP62A strain of S. epidermidis ([ATCC]35984; American Type Culture Collection, Manassas, VA, USA) was inoculated on Tryptic Soy Agar (TSA; Merck, Germany) medium and incubated at 37 °C for 24 h. After taking 4–5 colonies from single colonies with the help of a loop, these were inoculated into tryptic soy broth (TSB) medium and were incubated at 37 °C until the bacteria reached the logarithmic growth phase.
The bacterial culture in liquid medium was diluted, and a bacterial suspension was prepared in tryptic soy broth (TSB) corresponding to the 0.5 McFarland (108 cfu/mL) standard. Then, the suspension was diluted to 1/10 to obtain a 107 cfu/mL bacterial suspension. Sufficient bacterial inoculum (107 cfu/mL, 5 mL) was added to the wells to cover the surface of the implants.
Experimental Outcomes
Postoperatively, the animals were monitored in their own cages. During and after the surgical procedures, we did not observe any complications, such as bleeding or hematoma, in any of the animals. In the control groups, implant materials were removed from the pockets under sterile conditions after 1, 6 and 24 h in groups 1, 2 and 3, respectively. Similarly, in the experimental groups, implant materials were removed from the pockets under sterile conditions after 1, 6 and 24 h in groups 4, 5 and 6, respectively. As soon as the implants were removed, all rats were euthanized via drawing intracardiac blood.
Microbiological Evaluation
The main outcome measure of this study was the number of bacteria on implant surfaces. To determine the number of bacteria on their surfaces, serial dilutions were made with PBS solution, and 100 microliters (μL) were inoculated into the TSA medium using the smear method to determine the number of viable bacteria. After being kept in an oven at 37 °C for 18 h, the colonies grown were counted. The number of bacteria per milliliter was calculated using the number of colonies grown in the media and the relevant dilution factor. This is the gold standard method for counting viable microorganisms. All microbiological evaluation was done by a blinded expert.
Statistical Analysis
All data were analyzed using the IBM SPSS 15.0 (SPSS Inc., Chicago, IL, USA) package program. Descriptive statistics were expressed as median (minimum–maximum) for variables if the distribution was not normal. For the number of colonies, the significance of the difference in terms of median values was evaluated by using Mann–Whitney U and Kruskal–Wallis tests when the number of groups was two or more than two, respectively. Within the Kruskal–Wallis test, multiple comparisons were made using the post hoc Bonferroni test. The median numbers and mean ± standard deviation values of the colonies over time were evaluated with the Friedman test. This was done separately for surfaces with and without antibiotics and for different types of surfaces. Within the Friedman test, multiple comparisons were made using the Dunn–Bonferroni test. For p < 0.05, the results were considered statistically significant.
Results
Microbiological Evaluation
Bacterial load on each implant surface was measured quantitatively via scattering on the TSA medium. In groups without local antibiotic treatment, the least colonization was observed on smooth implant surfaces at all timepoints. In group 1 (1st h group without local antibiotic), the highest bacterial load was observed on polyurethane surfaces. At 6 and 24 h (Groups 2 and 3, respectively), the bacterial loads were equivalent on the polyurethane and textured surfaces; however, the smooth material remained the least populated surface (Fig. 2). The difference between the bacterial counts on smooth and other surfaces was statistically significant at all timepoints (Table 2).
In the experimental groups with local antibiotic treatment, the least colonization was observed on the polyurethane surface material at all timepoints. At 1 h and 6 h (Groups 4 and 5, respectively), the bacterial load on polyurethane surface material was found to be significantly lower than the colonization on the smooth and textured surface materials. However, at 24 h (Group 6), colonization levels on both the smooth and polyurethane surface were found to be significantly lower than on the textured surface (Fig. 3). Colonization was significantly higher at 1 h as compared to 24 h on all surface materials with antibiotics (Table 3).
In all groups, comparisons of the data for each surface material at different times were made separately using the Friedman test, and multiple comparisons were performed by using the Dunn–Bonferroni test. On the smooth surface without a local antibiotic, the highest number of colonies was measured at 6 h, and the lowest number was observed at 1 h; the difference was statistically significant. On the textured surface materials without a local antibiotic, the highest number and the lowest number of colonies were measured at 6 h and 1 h, respectively, but the difference was not statistically significant. On the polyurethane surface without a local antibiotic, the highest number and the lowest number of colonies were measured at 1 h and 24 h, respectively, and the difference was statistically significant (Table 2). On all surfaces treated with local antibiotics (Groups 4, 5 and 6), the highest number of colonies was measured at 1 h and, and the lowest number of colonies was measured at 24 h; the difference was statistically significant (Table 3).
For each surface material and time, a comparison of the data based on whether antibiotic treatment was performed, that is, between Groups 4, 5 and 6 and Groups 1, 2 and 3, was performed by using a Mann–Whitney U test. As compared to the untreated groups, bacterial colonization was significantly lower in the groups in which smooth and textured surfaces were treated with local antibiotics at 6 and 24 h. Bacterial colonization levels on the polyurethane surface at 1, 6 and 24 h were significantly lower in groups treated with local antibiotics than in untreated groups (Table 4).
Outcomes and Estimation
From a clinical point of view, we have observed that smooth implant surfaces have shown the least adherence on the part of microorganisms in untreated cases, whereas polyurethane and textured surfaces have demonstrated more colonization than smooth surfaces. However, in cases involving local antibiotic treatment, the colonization around smooth and textured surface materials remained similar to untreated cases, but polyurethane surfaces demonstrated a significant decrease in bacterial load as compared to untreated polyurethane surfaces and treated smooth and textured surfaces at all timepoints.
Regarding the interaction between the surface and the microorganisms, these findings suggest that textured implants are the most disadvantageous implants among the three surfaces available in the market because these surfaces displayed the greatest number of colonies in both untreated and treated cases. In contrast, smooth implants have the least potential to be negatively affected by the presence of bacterial contamination because they exhibit the least adherence to microorganisms. Still, due to the limited efficiency of local antibiotics on smooth surfaces, colonization not significantly reduced and, thus, may still be a risk factor for capsular contracture. Polyurethane implants demonstrated the most impressive results after local antibiotic treatment because the number of bacterial colonies was significantly reduced in treated cases. This is a huge advantage in terms of eliminating the impact of bacterial contamination on breast implant surfaces.
Adverse Events
There were no adverse effects in any of the control and experimental groups.
Discussion
Capsular contracture is the most common complication after breast augmentation, and it may cause reoperations [1,2,3]. Additionally, breast-implant-associated anaplastic large cell lymphoma (BIA-ALCL), which may emerge between the capsule and the implant, has also given rise to doubts about silicone breast implants in recent years. The biofilm which is a syntrophic community of microorganisms in which cells stick to each other and often also to a surface in an extracellular polymeric matrix is shown to be a source of subclinical infection and the subclinical infection created by biofilm is still considered among the leading etiological factors in the development of capsular contracture. Also, biofilm and subclinical infection are among the most likely causes of BIA-ALCL. Staphylococcus epidermidis (S. epidermidis) is the most frequently isolated microorganism from capsular samples. This bacterium is a natural member of breast flora, while other members of the flora include Propionibacterium acnes, Corynebacterium sp., Staphylococcus lugdunensis and hominis, Mycobacterias and others. [7,8,9, 11,12,13, 32, 33]
In our study, we aimed to evaluate the efficacy and duration of local antibiotic therapy on implants with different surfaces in terms of preventing the formation of a biofilm layer and related subclinical infection. The bacterial load on the removed implant surfaces was determined by colony counting using mediums, which is the gold standard method.
There are effective irrigation procedures described for local antibiotic treatment around the implants, such as povidone-iodine (betadine), bacitracin+sefazolin+gentamicin (Adam’s triple), betadine+sefuroxim+gentamicin (Giardano’s triple), betadine+saline and other combinations. Irrigation with these procedures has been shown to significantly reduce capsular contracture. The US Food and Drug Administration (FDA) banned the use of betadine in the spring of 2000, on the grounds that it could cause spontaneous implant rupture but FDA removed the ban against betadine use for breast implant in 2017. Authors such as Wiener suggest that there is no evidence betadin use causes spontaneous implant rupture [34,35,36,37,38,39]. In this study, we preferred rifamycin, as a single variable, due to its wide spectrum of action on both Gram (+) and Gram (-) bacteria and efficacy in preventing the atypical mycobacterial infection and the subclinical inflammatory process.
In the groups without local antibiotic treatment, the bacterial loads on the polyurethane and textured surfaces were measured above the standard value (107) at all timepoints. In these groups, the bacterial load on smooth surfaces was below the standard value (107) but increased over time (Figure 2). In addition, significant differences were found between the smooth and polyurethane surfaces at all timepoints, as well as between the smooth and textured surfaces at 6 and 24 h, with the smooth surface indicating better results. However, there was no significant difference between polyurethane and textured surfaces at any timepoints (Figure 4).
On the other hand, bacterial loads on all surfaces were measured below the standard value (107) in all groups with local antibiotic treatment. A dramatic decrease in bacterial load was observed on polyurethane surfaces. In these groups, there was a significant difference between polyurethane and textured surfaces, one in favor of polyurethane surface, at all timepoints. In addition, a significant difference was observed between the smooth and textured surfaces, one in favor of smooth surfaces, at 24 h. However, the difference between the polyurethane and smooth surfaces was not significant, even though there was less colony load on the polyurethane surface (Figure 5).
When the surface materials with and without antibiotic treatment (Groups 4, 5 and 6 versus Groups 1, 2 and 3) are compared; at 1 h, the difference was not significant between the smooth surfaces with and without antibiotics; however, a significant difference was observed in favor of the antibiotic-treated samples at 6 and 24 h on smooth surfaces. At 1 h, the difference between the textured surfaces with and without antibiotics was not significant; however, a significant difference was observed, one in favor of antibiotic-treated samples, at 6 and 24 h. On polyurethane surfaces, the difference was significant at all times and in favor of antibiotic-treated samples (Figure 6).
Graph showing statistical comparisons of groups without local antibiotics and with local antibiotics according to hours with error bars. Small values could not be shown in the graph due to large differences between the data. Therefore, the data were made suitable for display by using the standardization method
The bacterial load on all surfaces was significantly decreased at 24 h as compared to 1 h, even it was zero on half of the polyurethane and smooth samples at the 24 h. We can conclude that, although the bacterial load on the polyurethane surface was higher than that on the smooth surface at the beginning, local antibiotic treatment maintained its presence and effectiveness on the surface for 24 h and reduced the bacterial load regularly. On smooth surfaces, the bacterial load likely did not increase over time, due to the weak adhesion of the bacteria to the smooth surfaces from the beginning, and the load was decreased by the effect of antibiotics.
There was a significant decrease in bacterial colonization on polyurethane surfaces from the first h, while on smooth and textured surfaces, this occurred at 6 and 24 h, respectively. This may indicate the effectiveness of antibiotics on polyurethane from the 1st h, earlier than for smooth and textured surfaces (Figs. 2, 3). The higher duration and strength of local antibiotic treatment on polyurethane surfaces can be attributed to their superior absorption capacity as compared to other surfaces due to the spongy and hydrophilic structure of this material.
In samples without local antibiotics, we detected the lowest bacterial colony count on smooth surfaces, and this count remained stable over 24 h. However, on textured and polyurethane surfaces, bacterial load was higher than on smooth surfaces and, similarly, remained stable over 24 h. On the other hand, in samples with local antibiotics, we observed a significant decrease in bacterial colonies on polyurethane surfaces within 24 h, beginning with the 1st h. On smooth and textured surfaces with antibiotics, the decrease in bacterial load started with the 6th h, and the bacterial load on smooth surfaces was similar with those on polyurethane surfaces at the 24th h. However, the bacterial load on the textured surfaces was found to be higher than that on the other two surfaces at the 24th h.
Limitations of this study include lack of in vitro experiments, studying with only staphylococcus epidermidis and rifamycin. If there were more variables, more valuable findings could be obtained.
Conclusion
Although the initial bacterial load on polyurethane surfaces was higher as compared to other two surfaces, the effect of antibiotics began more quickly on polyurethane surfaces than smooth and textured surfaces and effectively reduced the bacterial load within 24 h. This may be attributed to the fact that polyurethane surface is spongy and more hydrophilic than the other materials. Bacterial colonization on smooth surfaces was also lower than that on textured and polyurethane surfaces from the beginning of the experiment, and bacterial load was significantly reduced with local antibiotic treatment within 24 h. However, on textured surfaces, we observed that the bacterial load was higher than that on smooth surfaces, which similar to the results for polyurethane surfaces, from the beginning of the experiment, but the local antibiotic treatment did not respond as effectively as on the polyurethane and smooth surfaces. Ultimately, the number of bacterial colonies on the textured surfaces at the 24th h was higher than on the other two surfaces, despite local antibiotic treatment.
This pioneering study comparing three different surface materials has shown that surface materials have different responses in the scenario of bacterial contamination. While smooth implants display the advantage of reduced bacterial adherence on the surface, textured implants remain the most inappropriate implants in terms of the bacterial load and following inflammatory response. On the other hand, polyurethane implants prove to be advantageous due to the fast and effective antibiotic response despite highest bacterial load among three surface materials.
References
Headon H, Kasem A, Mokbel K (2015) Capsular contracture after breast augmentation: an update for clinical practice. Arch Plast Surg 42(5):532–543. https://doi.org/10.5999/aps.2015.42.5.532
Chong SJ, Deva AK (2015) Understanding the etiology and prevention of capsular contracture: translating science into practice. Clin Plast Surg 42(4):427–436. https://doi.org/10.1016/j.cps.2015.06.007
Gampper TJ, Khoury H, Gottlieb W, Morgan RF (2007) Silicone gel implants in breast augmentation and reconstruction. Ann Plast Surg 59(5):581–590. https://doi.org/10.1097/01.sap.0000258970.31562.5d
Adams WP Jr (2009) Capsular contracture: What is it? What causes it? How can it be prevented and managed? Clin Plast Surg 36(1):119–126. https://doi.org/10.1016/j.cps.2008.08.007
Ajdic D, Zoghbi Y, Gerth D, Panthaki ZJ, Thaller S (2016) The relationship of bacterial biofilms and capsular contracture in breast implants. Aesthet Surg J 36(3):297–309. https://doi.org/10.1093/asj/sjv177
Bachour Y, Bargon CA, de Blok CJM, Ket JCF, Ritt M, Niessen FB (2018) Risk factors for developing capsular contracture in women after breast implant surgery: a systematic review of the literature. J Plast Reconstr Aesthet Surg 71(9):e29–e48. https://doi.org/10.1016/j.bjps.2018.05.022
Bachour Y, Verweij SP, Gibbs S et al (2018) The aetiopathogenesis of capsular contracture: a systematic review of the literature. J Plast Reconstr Aesthet Surg 71(3):307–317. https://doi.org/10.1016/j.bjps.2017.12.002
Virden CP, Dobke MK, Stein P, Parsons CL, Frank DH (1992) Subclinical infection of the silicone breast implant surface as a possible cause of capsular contracture. Aesthetic Plast Surg Spring 16(2):173–179. https://doi.org/10.1007/bf00450610
Pajkos A, Deva AK, Vickery K, Cope C, Chang L, Cossart YE (2003) Detection of subclinical infection in significant breast implant capsules. Plast Reconstr Surg 111(5):1605–1611. https://doi.org/10.1097/01.Prs.0000054768.14922.44
Rieger UM, Mesina J, Kalbermatten DF et al (2013) Bacterial biofilms and capsular contracture in patients with breast implants. Br J Surg 100(6):768–774. https://doi.org/10.1002/bjs.9084
Hu H, Jacombs A, Vickery K, Merten SL, Pennington DG, Deva AK (2015) Chronic biofilm infection in breast implants is associated with an increased T-cell lymphocytic infiltrate: implications for breast implant-associated lymphoma. Plast Reconstr Surg 135(2):319–329. https://doi.org/10.1097/prs.0000000000000886
Hu H, Johani K, Almatroudi A et al (2016) Bacterial biofilm infection detected in breast implant-associated anaplastic large-cell lymphoma. Plast Reconstr Surg 137(6):1659–1669. https://doi.org/10.1097/prs.0000000000002010
Mempin M, Hu H, Chowdhury D, Deva A, Vickery K (2018) The A, B and Cs of silicone breast implants: anaplastic large cell lymphoma, biofilm and capsular contracture. Materials (Basel). https://doi.org/10.3390/ma11122393
Allan JM, Jacombs ASW, Hu H, Merten SL, Deva AK (2012) Detection of bacterial biofilm in double capsule surrounding mammary implants: findings in human and porcine breast augmentation. Plast Reconstr Surg 129(3):578e–580e. https://doi.org/10.1097/PRS.0b013e3182419c82
Jacombs A, Tahir S, Hu H et al (2014) In vitro and in vivo investigation of the influence of implant surface on the formation of bacterial biofilm in mammary implants. Plast Reconstr Surg 133(4):471e–480e. https://doi.org/10.1097/prs.0000000000000020
Bergmann PA, Tamouridis G, Lohmeyer JA et al (2014) The effect of a bacterial contamination on the formation of capsular contracture with polyurethane breast implants in comparison with textured silicone implants: an animal study. J Plast Reconstr Aesthet Surg 67(10):1364–1370. https://doi.org/10.1016/j.bjps.2014.05.040
Tamboto H, Vickery K, Deva AK (2010) Subclinical (biofilm) infection causes capsular contracture in a porcine model following augmentation mammaplasty. Plast Reconstr Surg 126(3):835–842. https://doi.org/10.1097/PRS.0b013e3181e3b456
Giordano S, Peltoniemi H, Lilius P, Salmi A (2013) Povidone-iodine combined with antibiotic topical irrigation to reduce capsular contracture in cosmetic breast augmentation: a comparative study. Aesthet Surg J 33(5):675–680. https://doi.org/10.1177/1090820x13491490
Blount AL, Martin MD, Lineberry KD, Kettaneh N, Alfonso DR (2013) Capsular contracture rate in a low-risk population after primary augmentation mammaplasty. Aesthet Surg J 33(4):516–521. https://doi.org/10.1177/1090820x13484465
Coleman DJ, Foo IT, Sharpe DT (1991) Textured or smooth implants for breast augmentation? A prospective controlled trial. Br J Plast Surg 44(6):444–448. https://doi.org/10.1016/0007-1226(91)90204-w
Loch-Wilkinson A, Beath KJ, Knight RJW et al (2017) Breast implant-associated anaplastic large cell lymphoma in australia and new zealand: high-surface-area textured implants are associated with increased risk. Plast Reconstr Surg 140(4):645–654. https://doi.org/10.1097/prs.0000000000003654
Wong CH, Samuel M, Tan BK, Song C (2006) Capsular contracture in subglandular breast augmentation with textured versus smooth breast implants: a systematic review. Plast Reconstr Surg 118(5):1224–1236. https://doi.org/10.1097/01.prs.0000237013.50283.d2
Manav S, Ayhan MS, Deniz E et al (2020) Capsular contracture around silicone miniimplants following bacterial contamination: an in vivo comparative experimental study between textured and polyurethane implants. J Plast Reconstr Aesthet Surg 73(9):1747–1757. https://doi.org/10.1016/j.bjps.2020.02.049
Hakelius L, Ohlsén L (1997) Tendency to capsular contracture around smooth and textured gel-filled silicone mammary implants: a five-year follow-up. Plast Reconstr Surg 100(6):1566–1569. https://doi.org/10.1097/00006534-199711000-00030
Pennisi VR (1990) Long-term use of polyurethane breast prostheses: a 14-year experience. Plast Reconstr Surg 86(2):368–371. https://doi.org/10.1097/00006534-199008000-00033
Handel N, Gutierrez J (2006) Long-term safety and efficacy of polyurethane foam-covered breast implants. Aesthet Surg J 26(3):265–274. https://doi.org/10.1016/j.asj.2006.04.001
Pompei S, Evangelidou D, Arelli F, Ferrante G (2016) The modern polyurethane-coated implant in breast augmentation: long-term clinical experience. Aesthet Surg J 36(10):1124–1129. https://doi.org/10.1093/asj/sjw171
Castel N, Soon-Sutton T, Deptula P, Flaherty A, Parsa FD (2015) Polyurethane-coated breast implants revisited: a 30-year follow-up. Arch Plast Surg 42(2):186–193. https://doi.org/10.5999/aps.2015.42.2.186
ISO (2018) ISO 14607:2018 Non-active surgical implants—Mammary implants—Particular requirements. https://www.iso.org/standard/63973.html
Barr S, Hill E, Bayat A (2009) Current implant surface technology: an examination of their nanostructure and their influence on fibroblast alignment and biocompatibility. Eplasty 9:e22
Atlan M, Nuti G, Wang H, Decker S, Perry T (2018) Breast implant surface texture impacts host tissue response. J Mech Behav Biomed Mater 88:377–385. https://doi.org/10.1016/j.jmbbm.2018.08.035
Brody GS, Deapen D, Taylor CR et al (2015) Anaplastic large cell lymphoma occurring in women with breast implants: analysis of 173 cases. Plast Reconstr Surg 135(3):695–705. https://doi.org/10.1097/prs.0000000000001033
Bartsich S, Ascherman JA, Whittier S, Yao CA, Rohde C (2011) The breast: a clean-contaminated surgical site. Aesthet Surg J 31(7):802–806. https://doi.org/10.1177/1090820x11417428
Yalanis GC, Liu EW, Cheng HT (2015) Efficacy and safety of povidone-iodine irrigation in reducing the risk of capsular contracture in aesthetic breast augmentation: a systematic review and meta-analysis. Plast Reconstr Surg 136(4):687–698. https://doi.org/10.1097/prs.0000000000001576
Jewell ML, Adams WP Jr (2018) Betadine and breast implants. Aesthet Surg J 38(6):623–626. https://doi.org/10.1093/asj/sjy044
Wiener TC (2007) The role of betadine irrigation in breast augmentation. Plast Reconstr Surg 119(1):12–15. https://doi.org/10.1097/01.prs.0000251088.51675.a8
Wiener TC (2013) Betadine and breast implants: an update. Aesthet Surg J 33(4):615–617. https://doi.org/10.1177/1090820x13484036
Adams WP Jr (2018) Commentary on: surgical site irrigation in plastic surgery: What is essential? Aesthet Surg J 38(3):276–278. https://doi.org/10.1093/asj/sjx214
U.S. Food and Drug Administration (2017) Premarket approval (PMA): NATRELLE saline-filled breast implants. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpma/pma.cfm?ID=402786.
Acknowledgement
We thank Prof. Dr. Latif Ozturk and Dr. Yavuzalp Solak for their valuable contribution to the statistical analysis of the data.
Funding
Open access funding provided by the Scientific and Technological Research Council of Türkiye (TÜBİTAK). The authors received no financial support for the research, authorship and publication of this article. This study was presented at the 44th Congress of the Turkish Society of Plastic Reconstructive and Aesthetic Surgeons, which was held on November 2–6, 2022, in Antalya, Turkey, and awarded with the Second-Best Paper Prize in Experimental Research Category.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no potential conflicts of interest with respect to the research, authorship and publication of this article.
Ethical Approval
Ethical approval was obtained from the Gazi University Local Ethical Committee of Animal Experiments (Approval ID: G.U.ET-20.027).
Informed Consent
For this type of study, informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Karakas, E., Ayhan, M.S., Karasu, O. et al. In Vivo Comparison of the Efficacy and Duration of Local Antibiotics on Smooth, Textured and Polyurethane Implant Surfaces. Aesth Plast Surg (2024). https://doi.org/10.1007/s00266-024-04090-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00266-024-04090-2