Abstract
Purpose
Subcutaneous seroma formation (SF) is commonly seen after axillary bromhidrosis surgeries and its treatment can be challenging and long. Current prevention methods are not consistent, and the treatment includes repeated aspirations and drains, both are associated with higher risk for infections. The purpose of this article is to present a novel and simple technique of intraoperative hypertonic saline irrigation (IHSI) to axillary bromhidrosis subcutaneous dead space, which prevents postoperative SF and enables early drain removal due to reduced secretions.
Methods
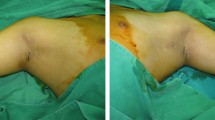
From 2015 to 2022, we performed the intraoperative irrigation of the cavity through normal saline in 100 patients with primary axillary bromhidrosis. Through an incision approximately 3 cm long at the central axillary crease, the entire subcutaneous tissues containing apocrine glands were initially dissected with straight scissors within the axillary area, and then, the undermined apocrine glands were removed with curved scissors. The skin was defatted to become a full-thickness skin flap. Any suspected hemorrhagic spots were immediately coagulated electrosurgically. Negative pressure drains were placed, and intraoperative irrigation of the cavity through the drains with 20 ml of NaCl 0.9% or NaCl 10% left at site for 10 min applies different saline solutions in the same patients.
Results
The volume of drainage on the 1st postoperative day was 6.54±0.36 mL for the group B, which was significantly less than 15.23±0.42 mL for the group A (p < 0.05). The time of drain removal for the group B was 24 h, which was shorter than 48 h for the group A. In group B, 4 percent of axillae showed significant SF postoperatively, which was lower than the 20 percent of axillae associated with the group A (p < 0.05). The rate of incision infection for the group B was 2 percent, which was significantly lower than the 6 percent of axillae in the group A (p < 0.05). Two percent of axillae showed skin edge necrosis postoperatively in the group B, which was lower than the 10 percent of axillae associated with the group A (p < 0.05).
Conclusions
IHSI enhances adhesion formation and reduces secretion rate in subcutaneous dissection space after axillary bromhidrosis surgeries, therefore enables early drain removal and prevents SF, incision infection and skin edge necrosis. As a result, reducing the pain of patients, decreasing inconveniency and cost saving of multiple outpatient visits or additional surgery.
Level of Evidence II
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.


Similar content being viewed by others
References
Sato T, Sonoda T, Itami S, Takayasu S (1998) Predominance of type I 5 alpha-reductase in apocrine sweat glands of patients with excessive or abnormal odour derived from apocrine sweat (osmidrosis). Br J Dermatol 139:806–810
Piccolo D, Mutlag MH, Pieri L, Fusco I, Conforti C, Crisman G, Bonan P (2023) Minimally invasive 1,444-nm Nd:YAG laser treatment for axillary bromhidrosis. Front Med (Lausanne) 10:1034122
Chen W, Zhang X, Zhang L, Xu Y (2021) Treatment of axillary bromhidrosis in adolescents by combining electrocauterization with ultrasound-guided botulinum toxin type a injection. J Plast Reconstr Aesthet Surg 74:3114–3119
Mohamoud AA, Zeraiq L, Vestergaard T (2022) A case series evaluating microwave-based therapy for axillary hyperhidrosis and bromhidrosis. J Dermatolog Treat 33:1572–1575
Van TN, Manh TN, Minh PPT, Minh TT, Huu ND, Cao KP, Huu QN, Cam VT, Huyen ML, Hau KT, Gandolfi M, Satolli F, Feliciani C, Tirant M, Vojvodic A, Lotti T (2019) The effectiveness of local surgical technique in treatment of axillary bromhidrosis, open access maced. J Med Sci 7:187–191
Li CY, Wang XF, Zhou HY, Fang QQ, Tan WQ (2021) Refined tumescent liposuction-curettage with pruning in small incisions for treatment of axillary bromhidrosis. Dermatol Ther 34:e14690
Hsu KC, Wang KY (2019) Sparing subcutaneous septa avoids skin necrosis in the treatment of axillary bromhidrosis with suction-curettage shaving. J Cosmet Dermatol 18:892–896
Tung TC, Wei FC (1997) Excision of subcutaneous tissue for the treatment of axillary osmidrosis. Br J Plast Surg 50:61–66
Yang H, Xu G, Huang CL, Xia Y, Wang XW, Chen Q, Wang SJ, Zhang LY, Tan WQ (2017) Effectiveness and complications of improved liposuction-curettage through mini-incisions for the treatment of axillary osmidrosis. Plast Surg (Oakv) 25:234–241
He J, Wang T, Dong J (2012) Excision of apocrine glands and axillary superficial fascia as a single entity for the treatment of axillary bromhidrosis. J Eur Acad Dermatol Venereol 26:704–709
Qian JG, Wang XJ (2010) Effectiveness and complications of subdermal excision of apocrine glands in 206 cases with axillary osmidrosis. J Plast Reconstr Aesthet Surg 63:1003–1007
Sood A, Kotamarti VS, Therattil PJ, Lee ES (2017) Sclerotherapy for the management of seromas: a systematic review. Eplasty 17:e25
Chen KH, Changchien CH, Fang CL, Yang CS, Tsai CB, Chen MS, Yang HY (2023) Factors affecting postoperative complications of suction-curettage by arthroscopic shaver for bromhidrosis. Ann Plast Surg 90:471–477
van Bastelaar J, Granzier R, van Roozendaal LM, Beets G, Dirksen CD, Vissers Y (2018) A multi-center, double blind randomized controlled trial evaluating flap fixation after mastectomy using sutures or tissue glue versus conventional closure: protocol for the seroma reduction after mastectomy (SAM) trial. BMC Cancer 18:830
Lee KT, Mun GH (2015) Fibrin sealants and quilting suture for prevention of seroma formation following latissimus dorsi muscle harvest: a systematic review and meta-analysis. Aesthetic Plast Surg 39:399–409
Pinero-Madrona A, Castellanos-Escrig G, Abrisqueta-Carrion J, Canteras-Jordana M (2016) Prospective randomized controlled study to assess the value of a hemostatic and sealing agent for preventing seroma after axillary lymphadenectomy. J Surg Oncol 114:423–427
Plymale MA, Harris JW, Davenport DL, Smith N, Levy S (2016) Scott roth, abdominal wall reconstruction: the uncertainty of the impact of drain duration upon outcomes. Am Surg 82:207–211
Hanna KR, Tilt A, Holland M, Colen D, Bowen B, Stovall M, Lee A, Wang J, Drake D, Lin K, Uroskie T, Campbell CA (2016) Reducing infectious complications in implant based breast reconstruction: impact of early expansion and prolonged drain use. Ann Plast Surg 76(4):S312-315
Dudai M, Gilboa Ittah K (2019) Intraoperative hypertonic saline irrigation preventing seroma formation and reducing drain secretion in extended endoscopic hernia and linea alba reconstruction glue. Hernia 23:1291–1296
Zamkowski M, Smietanski M (2023) Efficacy of intraoperative hypertonic saline irrigation in seroma prevention after abdominal wall reconstruction procedures–a pilot cohort study. ANZ J Surg 93:1594–1598
Lam Hoai XL, Kabagabo C, Simonart T (2020) Treatment of axillary bromhidrosis with lemon applications. Dermatol Ther 33:e14133
Li ZR, Sun CW, Zhang JY, Qi YQ, Hu JZ (2015) Excision of apocrine glands with preservation of axillary superficial fascia for the treatment of axillary bromhidrosis. Dermatol Surg 41:640–644
Li H, Qin G, Zhang J, Jia X, Ishaq HM, Yang H, Wu S, Xu J (2022) Axillary fossaa microbial dysbiosis and its relationship with axillary osmidrosis patients. Microb Pathog 173:105886
Li Y, Huang Z, Ran L, Wang W, Yu X, Wang R (2022) A retrospective study on comparing the surgery and microneedles radiofrequency and microwaves treatment in axillary osmidrosis. J Dermatolog Treat 33:420–426
Chen SQ, Wang TT, Zhou Y, Li W, Man XY (2022) Comparison of long-term effectiveness and safety of microwave and surgery in the treatment of axillary osmidrosis: a single-center retrospective study. Dermatol Surg 48:126–130
Wu CJ, Chang CK, Wang CY, Liao YS, Chen SG (2019) Efficacy and safety of botulinum toxin a in axillary bromhidrosis and associated histological changes in sweat glands: a prospective randomized double-blind side-by-side comparison clinical study. Dermatol Surg 45:1605–1609
Shin JY, Roh SG, Lee NH, Yang KM (2017) Osmidrosis treatment approaches: a systematic review and meta-analysis. Ann Plast Surg 78:354–359
Wang R, Yang J, Sun J (2015) A minimally invasive procedure for axillary osmidrosis: subcutaneous curettage combined with trimming through a small incision. Aesthet Plast Surg 39:106–113
Albanese G, Kondo KL (2010) Pharmacology of sclerotherapy. Semin Interv Radiol 27:391–399
Sood A, Kotamarti VS, Therattil PJ, Lee ES (2017) Sclerotherapy for the management of seromas: a systematic review. Eplasty 17:e25
Gruver DI (2003) Hypertonic saline for treatment of seroma. Plast Reconstr Surg 112(3):934
Funding
None.
Author information
Authors and Affiliations
Contributions
YW is the first author of the article. SX is corresponding author. YW involved in conceptualization, formal investigation and writing. SX involved in study initiation, design, investigation, supervision, review and editing of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest to disclose.
Ethical Approval
This article was approved by the ethics committee of the First People’s Hospital of Xuzhou.
Informed Consent
For this type of study, informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, Y., Xie, S. Intraoperative Hypertonic Saline Irrigation Preventing Seroma Formation in the Treatment of Axillary Bromhidrosis. Aesth Plast Surg (2024). https://doi.org/10.1007/s00266-024-03987-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00266-024-03987-2