Abstract
Background
While micro-plasma radiofrequency (MPR) treatment has a significant impact on hypertrophic scars, patients often require anesthesia to alleviate substantial discomfort. Currently, patients with similar degrees of scarring may choose surface anesthesia or general anesthesia based on their personal preferences. Nevertheless, the effectiveness and safety of different anesthesia modalities remain uncertain.
Objective
To assess the effectiveness and safety of both general and surface anesthesia in MPR treatment for hypertrophic scars.
Methods
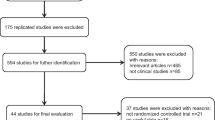
We conducted a retrospective cohort study involving 101 patients diagnosed with hypertrophic scars who underwent MPR with different anesthesia methods. The primary measures of efficacy included the Vancouver Scar Scale (VSS) scores assessed before the first treatment and six months after the final treatment. Pain relief was evaluated using Visual Analog Scale (VAS) scores. Safety was assessed by comparing the incidence of adverse reactions between the two groups.
Results
Patients in the general anesthesia group showed a significant difference in scar pigmentation 6 months after the treatment and lower pain level than those in the surface anesthesia group in the treatment of MPR. The difference in safety was not statistically significant. After adjusting for confounding factors and propensity score matching, the outcome of VSS and VAS scores was stable.
Conclusion
General anesthesia, as opposed to surface anesthesia, appears to enhance both the effectiveness and safety of MPR while reducing postoperative pain in the treatment of hypertrophic scars. For patients with heightened pain sensitivity, general anesthesia may be the preferred treatment option.
Level of Evidence II
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors http://www.springer.com/00266.





Similar content being viewed by others
Abbreviations
- MPR:
-
Micro-plasma radiofrequency
- PLA:
-
People's Liberation Army
- VSS:
-
Vancouver Scar Scale
- VAS:
-
Visual Analog Scale
- CI:
-
Confidence interval
- PSM:
-
Propensity score matching
References
Ziolkowski NI, Behman R, Klassen AF et al (2021) Determining the independent risk factors for worse SCAR-Q scores and future scar revision surgery. Plast Reconstr Surg 148(1):203–212
Guo Q, Xu P, Ye J (2022) Observation on the efficacy of 1565 nm non-ablative fractional laser combined with compound betamethasone topical application on the treatment of early scar in Chinese patients. Lasers Med Sci 37(7):2947–2953
Fu X, Dong J, Wang S, Yan M, Yao M (2019) Advances in the treatment of traumatic scars with laser, intense pulsed light, radiofrequency, and ultrasound. Burns Trauma 7:1
Baroni A, Verolino P (2021) Plasma radiofrequency ablation for scar treatment. J Clin Med 11(1):140
Li X, Fang L, Huang L (2015) In vivo histological evaluation of fractional ablative microplasma radio frequency technology using a roller tip: an animal study. Lasers Med Sci 30(9):2287–2294
Stevic M, Vlajkovic A, Trifunovic B et al (2019) Topical anesthetics for pediatric laser treatment. J Cosmet Laser Ther 21(7–8):417–421
Wang Y, Sun Z, Cai L, Zhang F (2023) Comparative efficacy and safety of six photoelectric therapies for the atrophic acne scars: a network meta-analysis. Indian J Dermatol Venereol Leprol 89(3):353–362
Lan T, Xiao Y, Tang L, Hamblin MR, Yin R (2018) Treatment of atrophic acne scarring with fractional micro-plasma radio-frequency in Chinese patients: a prospective study. Lasers Surg Med 50(8):844–850
Finnerty CC, Jeschke MG, Branski LK, Barret JP, Dziewulski P, Herndon DN (2016) Hypertrophic scarring: the greatest unmet challenge after burn injury. Lancet 388(10052):1427–1436
Li J, Wang D, Wang Y, Du Y, Yu S (2021) Effectiveness and safety of fractional micro-plasma radio-frequency treatment combined with ablative fractional carbon dioxide laser treatment for hypertrophic scar: a retrospective study. Ann Palliat Med 10(9):9800–9809
Pinheiro NM, Melo PR, Crema VO, Mendonça AC (2015) Effects of radiofrequency procedure on hypertrophic scar due to burns. J Eur Acad Dermatol Venereol 29(1):187–189
Lin MJ, Dubin DP, Torbeck RL 3rd et al (2023) Early fractional ablative laser for skin cancer excision scars: a randomized split-scar study. Dermatol Surg 49(4):338–342
Kono T, Groff WF, Sakurai H, Yamaki T, Soejima K, Nozaki M (2009) Treatment of traumatic scars using plasma skin regeneration (PSR) system. Lasers Surg Med 41(2):128–130
Shirakami E, Yamakawa S, Hayashida K (2020) Strategies to prevent hypertrophic scar formation: a review of therapeutic interventions based on molecular evidence. Burns Trauma 8:tkz003
Leszczynski R, da Silva CA, Pinto A, Kuczynski U, da Silva EM (2022) Laser therapy for treating hypertrophic and keloid scars. Cochrane Database Syst Rev 9(9):Cd011642
Hultman CS, Friedstat JS, Edkins RE, Cairns BA, Meyer AA (2014) Laser resurfacing and remodeling of hypertrophic burn scars the results of a large, prospective, before-after cohort study, with long-term follow-up. Ann Surg 260(3):519–529
Halachmi S, Orenstein A, Meneghel T, Lapidoth M (2010) A novel fractional micro-plasma radio-frequency technology for the treatment of facial scars and rhytids: a pilot study. J Cosmet Laser Ther 12(5):208–212
Kilmer SL, Chotzen V, Zelickson BD et al (2003) Full-face laser resurfacing using a supplemented topical anesthesia protocol. Arch Dermatol 139(10):1279–1283
Tollan CJ, MacLaren W, Mackay IR (2016) Topical anaesthetic effects on skin vasculature with potential implications for laser treatment. Lasers Med Sci 31(4):611–617
Yuan B, Upton Z, Leavesley D, Fan C, Wang XQ (2023) Vascular and collagen target: a rational approach to hypertrophic scar management. Adv Wound Care 12(1):38–55
Abd-Elsayed A, Pope J, Mundey DA et al (2022) Diagnosis, treatment, and management of painful scar: a narrative review. J Pain Res 15:925–937
Wong BM, Keilman J, Zuccaro J, Kelly C, Maynes JT, Fish JS (2017) Anesthetic practices for laser rehabilitation of pediatric hypertrophic burn scars. J Burn Care Res 38(1):e36–e41
Searle T, Ali FR, Al-Niaimi F (2021) Lessons learned from the first decade of laser-assisted drug delivery. Dermatol Ther 11(1):93–104
Shi Y, Jiang W, Li W, Zhang W, Zou Y (2021) Comparison of fractionated frequency-doubled 1,064/532 nm picosecond Nd:YAG lasers and non-ablative fractional 1,540 nm Er: glass in the treatment of facial atrophic scars: a randomized, split-face, double-blind trial. Ann Transl Med 9(10):862
Zhang M, Fang J, Wu Q, Lin T (2020) Evaluation of the safety and efficacy of a picosecond alexandrite laser with DLA for acne scars in Chinese patients. Lasers Surg Med 52(2):176–181
Kouba DJ, LoPiccolo MC, Alam M et al (2016) Guidelines for the use of local anesthesia in office-based dermatologic surgery. J Am Acad Dermatol 74(6):1201–1219
Chandrasoma J, Harrison TK, Ching H, Vokach-Brodsky L, Chu LF (2018) Peripheral nerve blocks for hand procedures. N Engl J Med 379(10):e15
Verner I (2016) Clinical evaluation of the efficacy and safety of fractional bipolar radiofrequency for the treatment of moderate to severe acne scars. Dermatol Ther 29(1):24–27
Lan T, Tang L, Xia A, Hamblin MR, Jian D, Yin R (2021) Comparison of fractional micro-plasma radiofrequency and fractional microneedle radiofrequency for the treatment of atrophic acne scars: a pilot randomized split-face clinical study in China. Lasers Surg Med 53(7):906–913
Wang S, Mi J, Li Q, Jin R, Dong J (2017) Fractional microplasma radiofrequency technology for non-hypertrophic post-burn scars in Asians: a prospective study of 95 patients. Lasers Surg Med 49(6):563–569
Passeron T, Lim HW, Goh CL et al (2021) Photoprotection according to skin phototype and dermatoses: practical recommendations from an expert panel. J Eur Acad Dermatol Venereol 35(7):1460–1469
Elrefaie AM, Salem RM, Faheem MH (2020) High-resolution ultrasound for keloids and hypertrophic scar assessment. Lasers Med Sci 35(2):379–385
Ogawa R (2022) The most current algorithms for the treatment and prevention of hypertrophic scars and keloids: a 2020 update of the algorithms published 10 years ago. Plast Reconstr Surg 149(1):79e–94e
Funding
None.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics Statement
The patients in this manuscript have given written informed consent to the publication of their case details.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Meng, F., Wu, Q., Zheng, C. et al. The Comparison of Efficacy and Safety Between General and Topical Anesthesia on Micro-Plasma Radiofrequency Treatment for Hypertrophic Scar: A Retrospective Cohort Study. Aesth Plast Surg 48, 451–460 (2024). https://doi.org/10.1007/s00266-023-03706-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-023-03706-3