Abstract
Background
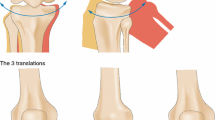
Lower lateral cartilage repositioning (LLCR) is an effective technique that places the lateral crus in a newly created caudal pocket, and is utilized for a variety of indications including cephalic malposition, alar asymmetries and tip rotation/projection alteration. However, there is a relative sparsity in the literature regarding this procedure and the dynamic changes that it produces. In this study, we report our experience with LLCR in regard to its indications and related interplays.
Methods
Data from our institution were collected from the most recent 100 primary rhinoplasties, most recent 100 secondary rhinoplasties and all LLCRs performed. For each LLCR, patient demographics and concurrent surgical techniques were compiled. A descriptive analysis was performed for all cohorts, while Fischer’s exact test was performed to compare the associations of categorical data for the respective sample sizes of the primary and secondary rhinoplasty cohorts.
Results
Overall, 127 patients underwent LLCR, with eleven (11%) LLCRs in the primary rhinoplasty cohort and twelve (12%) LLCRs in the secondary rhinoplasty cohort. The most common indication for LLCR was cephalic malposition, followed by over-projection and asymmetry of the lower lateral cartilages. Intraoperative observation of dynamic changes included invariable cephalic rotation of the tip, ability to precisely control the tip projection, drastic narrowing of the domal arch often minimizing the need for the transdomal suture, alar repositioning caudally, correction of alar retraction and more elegant tip definition. However, the external valve lost its strength on majority of LLCR patients, which required almost routine use of Gunter lateral crus strut.
Conclusion
LLCR is a powerful and versatile tool that can be utilized in either primary or secondary rhinoplasty. Its transposition results in cephalic rotation of the tip, narrowing of the domal arch, caudal reposition of the alar rim and superior tip definition.
Level of Evidence IV
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266


Similar content being viewed by others
References
Behmand RA, Ghavami A, Guyuron B (2003) Nasal tip sutures part I: the evolution. Plast Reconstr Surg. 112(4):1125–9. https://doi.org/10.1097/01.Prs.0000076503.78510.1c (discussion 1146-9)
Ghavami A, Janis JE, Acikel C, Rohrich RJ (2008) Tip shaping in primary rhinoplasty: an algorithmic approach. Plast Reconstr Surg 122(4):1229–1241. https://doi.org/10.1097/PRS.0b013e31817d5f7d
Tebbetts JB (1994) Shaping and positioning the nasal tip without structural disruption: a new, systematic approach. Plast Reconstr Surg 94(1):61–77. https://doi.org/10.1097/00006534-199407000-00006
Byun JS, Kim KK (2013) Correction of asian short nose with lower lateral cartilage repositioning and ear cartilage grafting. Plast Reconstr Surg Glob Open 1(6):e45. https://doi.org/10.1097/GOX.0b013e3182a85b29
Lam SM, Williams EF 3rd (2002) Anatomic considerations in aesthetic rhinoplasty. Facial Plast Surg 18(4):209–214. https://doi.org/10.1055/s-2002-36488
Sheen JH, Sheen AP. Aesthetic rhinoplasty. Quality Medical Pub.; 1998.
Courtiss EH, Goldwyn RM (1983) The effects of nasal surgery on airflow. Plast Reconstr Surg 72(1):9–21. https://doi.org/10.1097/00006534-198307000-00003
Constantian MB (1994) The incompetent external nasal valve: pathophysiology and treatment in primary and secondary rhinoplasty. Plast Reconstr Surg. 93(5):919–31 (discussion 932-3)
Constantian MB (1993) Functional effects of alar cartilage malposition. Ann Plast Surg 30(6):487–499. https://doi.org/10.1097/00000637-199306000-00003
Guyuron Bahman, Behmand Ramin A (2003) Nasal Tip Sutures Part II: The Interplays. Plast Reconstr Surg 112(4):1130–1145. https://doi.org/10.1097/01.PRS.0000076505.83375.74 (discussion 1146-9)
Toriumi DM, Asher SA (2015) Lateral crural repositioning for treatment of cephalic malposition. Facial Plast Surg Clin North Am 23(1):55–71. https://doi.org/10.1016/j.fsc.2014.09.004
Kridel RWH, Konior RJ, Shumrick KA, Wright WK (1989) Advances in Nasal Tip Surgery: The Lateral Crural Steal. Archives of Otolaryngol- Head Neck Surg 115(10):1206–1212. https://doi.org/10.1001/archotol.1989.01860340060018
Janis JE, Trussler A, Ghavami A, Marin V, Rohrich RJ, Gunter JP (2009) Lower lateral crural turnover flap in open rhinoplasty. Plast Reconstr Surg 123(6):1830–1841. https://doi.org/10.1097/PRS.0b013e3181a65ba2
Bared A, Rashan A, Caughlin BP, Toriumi DM (2014) Lower lateral cartilage repositioning: objective analysis using 3-dimensional imaging. JAMA Facial Plast Surg 16(4):261–267. https://doi.org/10.1001/jamafacial.2013.2552
Cho BC, Lee JW, Lee JS et al (2021) Correction of secondary unilateral cleft lip nasal deformity in adults using lower lateral cartilage repositioning, columellar strut, and onlay cartilage graft on the nasal tip with open rhinoplasty combined with reverse-U incision. J Plast Reconstr Aesthet Surg 74(5):1077–1086. https://doi.org/10.1016/j.bjps.2020.10.060
Ilhan AE, Sozen T, CaypinarEser B, Cengiz B (2017) Association of Skin Thickness With Alar Base Reduction in Patients Undergoing Lateral Crural Repositioning and Strut Grafting. JAMA Facial Plast Surg. 19(6):516–521. https://doi.org/10.1001/jamafacial.2017.0486
Shaida AM, Kenyon GS (2000) The nasal valves: changes in anatomy and physiology in normal subjects. Rhinology 38(1):7–12
Ponsky D, Eshraghi Y, Guyuron B (2010) The frequency of surgical maneuvers during open rhinoplasty. Plast Reconstr Surg 126(1):240–244. https://doi.org/10.1097/PRS.0b013e3181dc54da
Xia TY, Punjabi A, Oh JH, Wee C, Guyuron B (2020) Updated Dynamics of Rhinoplasty: A Review of the Literature and Comprehensive List of the Findings. Aesthetic Plast Surg 44(3):904–909. https://doi.org/10.1007/s00266-020-01619-z
Funding
The authors have no funding to disclose.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest to disclose.
Human and Animal Rights, or Ethical Approval
All procedures performed in studies involving human participants were conducted in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
All patients provided informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 163188 KB)
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wells, M.W., Chang, I.A. & Guyuron, B. Frequency, Indications and Intraoperative Dynamics of Repositioning of the Lateral Crura of the Lower Lateral Cartilage: A 35-Year Experience. Aesth Plast Surg 47, 717–727 (2023). https://doi.org/10.1007/s00266-022-03034-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-022-03034-y