Abstract
Surgical management of helical and retroauricular keloids has been rarely discussed. This study aims to introduce our successful reconstruction of helical and retroauricular keloids using a novel hemi-keystone flap. The current study is a retrospective review of patients with pathologically confirmed helical and retroauricular keloids. All keloid cases were completely excised. We covered the defect with a hemi-keystone flap followed by a single fraction of 10 Gy radiation therapy at postoperative day 0 or postoperative pressure therapy using magnets for four months. Treatment outcome was recorded as recurrence or nonrecurrence. A follow-up period of a minimum of 12 months was required in all patients. Of 45 keloids in 33 patients, none of the cases had a recurrence of their auricular keloids and the postoperative course was uneventful. We successfully reconstructed helical and retroauricular keloids using our modified hemi-keystone flaps without any keloid recurrence in one-year follow-ups. This is especially useful during the COVID-19 pandemic when facial mask wearing is mandatory.
Level of Evidence IV
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introductions
Keloids are often resistant to treatment and have high recurrence rates [1]. Surgical excision followed by adjuvant therapy is the standard treatment for the keloids [2,3,4]. However, while physicians emphasize postoperative adjuvant treatment, appropriate surgical management is rarely discussed.
Regarding earlobe keloids, we introduced a novel classification based on gross morphology in 2013 and suggested appropriate surgical methods [5]. Many authors also showed their own excellent experience with surgical management of earlobe keloids [6].
However, little documentation was made on the surgical management of helical and retroauricular keloids compared with earlobe keloids [7,8,9,10]. Techniques described such as chondrocutaneous bilateral advancement flap or helical rim advancement also require extensive dissection exposing relatively large surface of ear cartilage [9, 10].
Additionally, in the era of COVID-19, when compulsory mask wearing is required, sensitive facial skin such as cheeks, nasal bridge, and retroauricular areas is prone to adverse skin reactions. This is explained by the local pressure of facial masks on sebaceous ducts developing or aggravating acne. It could also be explained by irritant or mechanical/friction dermatitis due to masks. All these adverse reactions could contribute to keloid aggravation or recurrence.
The frictional effect of the material held in place with elastic happens at the helical and retroauricular area. So, it is preferable to reconstruct the defect with viable, healthy tissue instead of doing primary closure of extensive defect or skin grafting or traditional keystone flap, which typically makes vertical incision parallel to mask elastics.
For these reasons, we introduce our modified hemi-keystone flaps for the aesthetic reconstruction of helical and retroauricular keloids and reveal their excellence in terms of keloid recurrence based on our clinical protocol.
Patients and Methods
All research procedures in this study were performed in accordance with the ethical guidelines of the 1975 Declaration of Helsinki. Written informed consent was obtained from all patients. All patients of our study provided consent to publish the information.
This was a retrospective review of patients with retroauricular keloids (or combined with helical keloids) who visited our institution between September 2020 and March 2022. Patients who presented to the outpatient clinic were included in the study according to the following criteria: (i) The scar was elevated and extended beyond the dimensions of the initiating injury site or lesion; (ii) the patients were older than 18 years; and (iii) complete excision of keloids followed by Hemi-keystone flap reconstruction and postoperative radiation therapy or pressure therapy using magnets was scheduled depending on the presurgical counseling.
The exclusion criteria were as follows: (i) if patients were unavailable for follow-up; (ii) if patients did not agree to comply with the treatment protocol; (iii) if they received additional adjuvant therapy during treatment; (iv) if we did not obtain histological confirmation; and (v) if patients were pregnant during the follow-up period.
All included patients consented to the requirement of final follow-up after 12 months. If the patients could not visit our clinic, we surveyed the scar status by telephone or email questionnaire.
Surgical Technique and Postoperative Care
All procedures were performed under local anesthesia. We excised keloids, including the proliferating core as previously described [8], and bleeding was controlled by step-by-step bipolar coagulation.
The technical details of the original keystone flap are well described in the original paper describing the technique.
This series applied the rotation hemi-keystone flap to cover defects after complete excision of retroauricular keloids. The wound was measured intraoperatively in two dimensions, with the longest dimension as length and its perpendicular axis as width. We then proceeded with a traditional keystone flaps design that started at 90° angles from the defect corners, producing a longitudinally curvilinear flap with a width equal to that of the defect. However, the width of the keystone arc may be increased in regions lacking sufficient skin laxity.
After flap marking, an incision was made along one “V” apex and then extended along a portion of the curvature arc of the keystone flap. This produces enough skin laxity centrally to allow easier flap advancement. To increase flap mobilization and facilitate wound edge approximation, the unilateral incised curvilinear portion of the flap is then undermined and gradually rotated toward the center of the defect. Flap rotation was carried out as much as needed until it achieved a satisfactory coverage of the defect with minimal tension. The donor site is closed in a “V–Y” fashion. This modification provides easier flap advancement and effectively shortens the overall scarring. The representative operative detail is presented in Fig. 1a–c and supplemental Fig. 1.
(Case #32 in Table 1). a A 43-year-old patient with a keloid at his left ear helix to the retroauricular area came to our department with intermittent pain, pruritus, and disfiguring appearance. b We completely excised the keloid and designed the Hemi keystone flap lateral to the defect. c We covered the defect with an elevated flap using nylon sutures. d On the same day of the surgery, our radiation oncologist at our hospital designed the area to be irradiated. e Three weeks postoperative appearance at the time of total stitches removal. Ear deformity seen on the immediate postoperative day was utterly gone without intervention
Adjuvant Pressure Therapy Using Magnets
Patients were instructed to use the magnets for approximately 8 hours per day for four months until the therapy was completed [11]. During the adjuvant pressure therapy, patients were seen frequently for follow-up for recurrence and evaluation of the success of the therapy. Our protocol included four cycles of application repeated throughout the day. Each cycle was composed of 2 hours of magnet application followed by a half-hour of relief. In some of the retroauricular areas, where the application of magnets was not feasible, we used adjuvant radiation therapy instead.
Adjuvant Radiation Therapy Protocol
When indicated, patients had received postoperative adjuvant radiotherapy within 8 hours of surgery on the same day. The planned target volume included the operative scar with a margin of 1.5 cm. The representative design is depicted in Fig. 1. The dotted circle in Fig. 1d is the area to be radiated.
A custom Cerrobend block was used to shield nontarget areas. The patients were irradiated with a 6-MeV electron beam by a linear accelerator at a 100-cm source-to-skin distance. A 0.5–1-cm bolus was applied over the skin. A single fraction of 10 Gy was administered for all cases. The corresponding biologically equivalent dose (BED) was calculated as 20 Gy (at α/β of 10). The BED was 60 Gy when adopting α/β of 2 based on a large meta-analysis, which depicted keloids as late-responding tissue.
Follow-up and Outcome Assessment
A follow-up period of at least 12 months was required in all patients. Treatment outcome was recorded as recurrence or nonrecurrence. Nonrecurrence was defined as a scar without signs of elevation and extension, although slight scarring or redness could be present. Recurrence was defined as any scar elevation or extension beyond the original surgical field.
Results
Baseline patient characteristics and outcome assessment are depicted in Table 1.
All 45 keloids in 33 patients completed the treatment protocol, with a follow-up interval of 12 months. Of these patients, 100 percent had successful treatment of their keloids without any keloid recurrence. The postoperative course was uneventful. Representative cases were presented.
Case 1 (Fig. 2)
(Case #17 in table 1). a, b A 30-year-old patient with a keloid at her left ear helix to the retroauricular area and earlobe came to our department with intermittent pain, pruritus, and disfiguring appearance. She also had a right earlobe keloids. (right side picture is not presented in this figure) c, d Postoperative appearance one year after surgery and radiation therapy. e Her left earlobe keloid was excised entirely. f Then, we completely excised her left ear helix to the retroauricular keloid and designed the Hemi keystone flap lateral to the defect. g After incision of the planned line, H We closed the defect with an elevated flap
A 30-year-old female patient with right earlobe and helical keloids came to our clinic for her disfiguring ear deformity, severe pruritus, and intermittent pain. Previously, she underwent surgical excisions followed by intralesional steroid injections four times at other hospitals and one surgical excision followed by intralesional bleomycin injection.
We completely excised the keloid tissue, including proliferating core at her right earlobe and helical region. Then, we primarily closed the earlobe, but the extensive defect at the helical region prevented us from doing direct linear closure. So, we elevated the hemi-keystone flap from the retroauricular surface and successfully closed the wound without much tension.
We adopted our unique dressing method in the early postoperative period until one day that we introduced it in 2013 [12].
On the same day of her surgery, we performed postoperative radiation therapy as described in the adjuvant radiation protocol. A single fraction of 10 Gy was administered. She did not undergo adjuvant pressure therapy using magnets. At a one-year postoperative follow-up, her right ear was well maintained without keloid recurrence. She was also very satisfied with the aesthetic outcome.
Case 2 (Fig. 3)
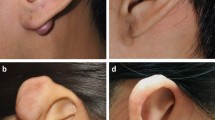
(Case #23 in table 1). a, b A 25-year-old patient with a keloid at her left ear helix to the retroauricular area came to our department with intermittent pain, pruritus, and disfiguring appearance. c, d Postoperative appearance one year after surgery and radiation therapy. e Appearance of excised keloid tissue. f We completely excised the keloid and designed the Hemi keystone flap lateral to the defect. g We covered the defect with an elevated flap using nylon sutures
A 25-year-old female patient with left retroauricular keloid came to our clinic for her disfiguring ear deformity, pruritus, and pain. Previously, she underwent surgical excision followed by intralesional steroid injections once at other hospitals. Still, it failed, and she received multiple intralesional steroid injections afterward to relieve the pain and pruritus. We completely excised the keloid tissue, including proliferating core at her right earlobe and helical region. After complete excision, we elevated the hemi-keystone flap from the retroauricular surface and successfully closed the wound without much tension.
On the same day of her surgery, we performed postoperative radiation therapy described in the adjuvant radiation protocol. A single fraction of 10 Gy was administered. She did not undergo adjuvant pressure therapy using magnets. At a one-year postoperative follow-up, her right ear was well maintained without keloid recurrence. She was also very satisfied with the aesthetic outcome.
Discussion
Numerous surgical techniques have been used to reconstruct auricular keloids following complete excision, including the subcutaneous island pedicle flap and suprakeloidal flap, and primary skin grafting, such as full and split-thickness skin grafts [5].
Although these techniques have pros and cons, primary closure after keloid excision is desirable whenever possible. Using flaps and skin grafts and neglecting the first step on the reconstructive ladder can jeopardize the wound to a higher keloid recurrence rate. Nevertheless, in some rare clinical situations, direct closure is not feasible or not possible.
In these unique cases, we have to use skin grafts or local flaps to cover the defect after keloid excision. However, skin graft uptake significantly decreases if we use early postoperative adjuvant radiation therapy after skin grafting to decrease the keloid recurrence. For this reason, radiation therapy should be postponed if skin grafting was used to cover the defect after keloid excision making keloids vulnerable to recurrence. So, it is better not to use skin grafting as a coverage method after keloid excision once the patient is scheduled to undergo postoperative radiation therapy.
In addition, it was assumed that closing defects with skin grafts using distant tissue would make poor color and texture match between the graft and the surrounding skin, which contributes to poor patient satisfaction.
Some authors elevated wide retroauricular flaps to reconstruct defects of the helical rim keloid excision [13]. However, this flap requires wide dissection of normal scalp area and also needs additional flap detachment surgery three weeks postoperatively. As we know, any additional surgery increases the possibility of keloid recurrence, and there is a chance that this wide flap dissection and subsequent detachment surgery cannot provide an aesthetically pleasing result.
Techniques described to reconstruct the helical keloids such as chondrocutaneous bilateral advancement flap or helical rim advancement also require extensive dissection exposing relatively large surface of ear cartilage despite some advantages [9, 10].
In 2013, we published our initial successful experience treating retroauricular keloids treated with complete excision followed by postoperative magnet therapy [14]. Although the simple treatment protocol mentioned in that study was excellent overall, some female patients complained of loss of normal mastoid-helix angle with a mild lying ear deformity after primary closure of retroauricular defect. This deformity might have been prevented with flap or skin grafting at a significant defect within the mastoid-helix angle following keloid excision. To overcome this, we introduced our successful reconstruction of retroauricular keloids with keystone design perforator island flap (KDPIF) in this clinical situation to reduce wound tension in 2018 [15]. The major advantage of this KDPIF is that it is a single-stage operation using redundant soft tissue in the mastoid-helix area that does not distort the normal mastoid-helix angle.
Although the keystone flap has become a versatile option for reconstruction of retroauricular keloids after complete excision, it has certain limiting issues. One is that the keystone flap demands a relatively remarkable incision area proportional to the defect size [16]. In the long-term follow-up, any additional incisions for keloid patients could be possible recurrence sites.
To address this problem, we came up with a novel rotation hemi-keystone flap design involving combing the principle of the modified rotation advancement keystone design while minimizing the incisional area of the traditional keystone flap. The actual incision length is almost half the length of the original keystone flap. The technique involves a unilateral incision of the conventional keystone flap followed by an additional step of flap elevation and dissection of the curvilinear portion of the flap. The flap is then rotated until the defect is closed, tension-free. In this approach, the wounds can be closed with low tension without compromising the flap vascularity while using only a part of the original keystone design.
Conclusions
We successfully reconstructed helical and retroauricular keloids using our modified hemi-keystone flaps without any keloid recurrence in one-year follow-ups. This is especially useful during the COVID-19 pandemic when facial mask wearing is mandatory.
References
Yu Y, Wu H, Zhang Q, Ogawa R, Fu S (2021) Emerging insights into the immunological aspects of keloids. J Dermatol 48:1817–1826
Ogawa R (2022) The most current algorithms for the treatment and prevention of hypertrophic scars and keloids: a 2020 update of the algorithms published 10 years ago. Plast Reconstr Surg 149:79e–94e
Dong W, Qiu B, Fan F (2022) Adjuvant radiotherapy for keloids. Aesthetic Plast Surg 46:489–499
Ogawa R (2022) Invited discussion on: adjuvant radiotherapy for keloids. Aesthetic Plast Surg 46:500–501
Park TH, Seo SW, Kim JK, Chang CH (2012) Earlobe keloids: classification according to gross morphology determines proper surgical approach. Dermatol Surg 38:406–412
Teng Y, Hao Y, Liu H et al (2022) Histology and vascular architecture study of keloid tissue to outline the possible terminology of keloid skin flaps. Aesthetic Plastic Surg
Park TH, Rah DK (2017) Successful eradication of helical rim keloids with surgical excision followed by pressure therapy using a combination of magnets and silicone gel sheeting. Int Wound J 14:302–306
Chong Y, Kim CW, Kim YS, Chang CH, Park TH (2018) Complete excision of proliferating core in auricular keloids significantly reduces local recurrence: a prospective study. J Dermatol 45:139–144
Kwek JWM, Lee TS, Loh ICY (2019) Helical rim advancement—a technique to avoid keloid recurrence. JPRAS Open 19:61–66
Maeda T, Hayashi T, Murao N, Yamamoto Y (2019) Chondrocutaneous bilateral advancement flap with postoperative radiation therapy for a helical rim keloid. Aesthetic Plast Surg 43:658–662
Park TH, Seo SW, Kim JK, Chang CH (2011) Outcomes of surgical excision with pressure therapy using magnets and identification of risk factors for recurrent keloids. Plast Reconstr Surg 128:431–439
Park TH, Chang CH (2013) Early postoperative magnet application combined with hydrocolloid dressing for the treatment of earlobe keloids. Aesthetic Plast Surg 37:439–444
Wang YY, Wang K, Chen WL, Wang YM (2022) Use of retroauricular flaps to reconstruct defects of the helical rim and adjuvant intralesional corticosteroids after resection of large keloids. J Craniofac Surg
Park TH, Park JH, Kim JK, Seo SW, Rah DK, Chang CH (2013) Analysis of 15 cases of auricular keloids following conchal cartilage grafts in an asian population. Aesthetic Plast Surg 37:102–105
Park TH, Kim CW, Chang CH (2018) Aesthetic reconstruction of retroauricular keloid: creating a keystone flap from the mastoid-helix area. J Dermatol 45:584–586
Yoon CS, Kong YT, Lim SY, Kim J, Shin HW, Kim KN (2021) A comparative study for tension-reducing effect of Type I and Type II keystone perforator island flap in the human back. Sci Rep 11:16699
Acknowledgements
This research was supported by Hallym University Research Fund 2021(HURF-2021-36) We also deeply appreciated to Medical Art Studio for medical illustration visualizing our concept.
Funding
This research was supported by Hallym University Research Fund 2021 (HURF-2021-36).
Author information
Authors and Affiliations
Contributions
THP solely designed, performed the research, analyzed the data, wrote the paper, and finally reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The author has no conflict of interest regarding the submitted work.
Ethical Standard
The displayed study was carried out with respect to high ethical standards. All the studies have been approved, when required, by the appropriate ethics committee and have, therefore, been performed in accordance and in conformity with the World Medical Association Declaration of Helsinki (June 1964) and subsequent amendments.
Informed Consent
All patients signed an informed consent for the procedures. For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
About this article
Cite this article
Park, T.H. Aesthetic Reconstruction of Auricular Keloids with a Novel Hemi-keystone Flap. Aesth Plast Surg 46, 2807–2813 (2022). https://doi.org/10.1007/s00266-022-02909-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-022-02909-4