Abstract
Background
The constricted ear is an auricular deformity produced by a deficiency in the circumference of the helical rim. The classification and corrective methods for constricted ears continue to be controversial. In order to identify them, the authors have reviewed and analyzed cases operated in a Chinese specialty clinic.
Methods
Correction of constricted ears from January of 2017 to June of 2021 was retrospect through medical records. Data of patients’ variables (including sex, age, laterality, type of constricted ear, presence of other ear anomalies), surgical techniques, esthetic outcomes, and postoperative complications have been collected.
Results
The deformed ears were classified into four graded types by three criteria including deficiency of auricle cartilage, vertical height in dorsal view, and surgical outcome. A total of 68 constricted ears of 57 patients (type I, n = 6; type IIA, n = 41; type IIB, n = 19, and type III, n = 2) were enrolled in the study. Of the 66 constricted ears undergoing surgical correction, most of them were performed with helical expansion through auricular/costal cartilage graft, Mustardé-type mattress sutures, and tumbling cartilage flap. External molding using Vaseline gauze rolls was implemented on every case to assist reshaping the scapha. A triangular superficial temporal fascial flap was elevated to prevent the reoccurrence of lidding in some cases. Corrective techniques and esthetic outcomes for deformed cases of each graded type were described. Based on a four-point Likert scale, the average esthetic outcome score was 3.7.
Conclusions
The classification was practical and the constricted ears were effectively corrected by simple surgical procedures without removal of deformed auricular cartilage. All corrections were performed in one stage.
Level of Evidence IV
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.
Similar content being viewed by others
Introduction
Constricted ears, also known as “lop” or “cup” ears, are the result of a deficiency in the circumference of the helical rim relative to the scapha, and the severe deformity is beyond helix, even presenting tubular shape in extreme cases. Cosman identified four characteristics of the constricted ear: lidding (a downward fold of the upper helix, produced by a deficiency of the scapha, superior crus, and fossa triangularis), protrusion (an anterior projection of the upper pole of the ear caused by a deeper concha fossa resulting from the flattened helix and antihelix), decreased vertical height, and low ear position (seen only in severe cases) [1]. Tanzer classified the deformities into four groups (groups I, IIA, IIB, and III) and suggested certain corrective methods for each group [2]. However, due to the heterogeneity of the appearance of deformed external ears, the classification of constricted ears and the methods of surgical intervention are still confusing and controversial [3,4,5].
In this article, we present a practical classification in consideration of not only the conditions of deformed ears but also the outcomes which could be achieved through simple procedures (such as addition of a piece of cartilage) not a new framework reconstruction. Otherwise, the highly heterogeneity of constricted ears was described by this retrospective study at the largest and the most authoritative auricular reconstruction center in China. Our review described surgical techniques with more covert incision than some methods above. Furthermore, the correction outcome of severe constricted ears achieved by simple surgical procedures was also presented in this study. Among those severe cases, some also defined as concha-type or small-concha-type microtia [6] have been previously suggested to be corrected by removing the deformed cartilage and reconstructing a new framework [7,8,9].
Patients and Methods
Data were obtained from the Department of Auricular Reconstruction at the Plastic Surgery Hospital of Peking Union Medical College (Beijing, People’s Republic of China). Surgical correction of constricted ears from January of 2017 to June of 2021 was retrospect through medical records. Patients with extreme cupping deformity who underwent auricular reconstruction were excluded from this study (Fig. 1). Patient variables (including sex, age, laterality, type of constricted ear, presence of other ear anomalies), surgical techniques, esthetic outcomes, and postoperative complications were reviewed. The study was authorized by our institution’s ethics committee and followed the World Medical Association Declaration of Helsinki. All study participants provided written informed consent.
The postoperative esthetic assessment of the reshaped auricle was graded by senior surgeon, which was based on a four-point Likert scale (i.e., 1= poor, 2 = fair, 3 = good, and 4 = excellent), considering factors of symmetry, size, shape, and the reconstruction of subtle structures (such as scapha and fossa triangularis).
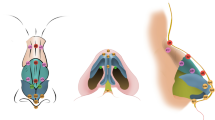
Classification of Constricted Ear
Patients showing features of lidded helix, compression of scapha and fossa triangularis, and/or cup-like protrusion were enrolled in the study. This study classified constricted ears into four groups: type I, type IIA, type IIB, and type III (Fig. 2). We considered three aspects for grading constricted ears: deficiency of auricle cartilage, vertical height in dorsal view, and surgical outcome (Table 1). Deficiency of the cartilage creates a downward fold of the upper helix with the absence of subtle structures, such as the scapha, superior crus, and fossa triangularis. The vertical height is compromised by deficiencies in the upper auricle cartilage and (or) the flattened helix and antihelix causing an anterior projection of the upper pole of the ear. Cartilage defects in the latter condition cannot be severe; therefore, the auricular deficiency could be corrected in totality through simple procedures, as type IIA constricted ears. Medium deficiency of cartilage (type IIB) could be corrected partially, and the size difference of bilateral ears (affected side and healthy side) after correction is less than one third, which is not easily noticed by a casual glance. Extreme cupping deformity (type III) featured by remarkable shortage of the helix and adjacent structures (including scapha and antihelix and even concha) could not be corrected by simple addition of pieces of cartilage, and auricular reconstruction with a new framework is required. Postoperative outcome is a guiding factor in the classification of constricted ears, and is also of great significance in the selection of surgical methods.
Operative Procedure and Technique
Surgery was performed under general anesthesia for all patients. All procedures described in the study were performed by the senior surgeons. In our series, a variety of operative techniques—Mustardé-type mattress sutures (MS), tumbling cartilage flap (CF), concha cartilage grafting, costal cartilage grafting, spilt folded helical cartilage, elevation of triangular superficial temporal fascial (TF) flap, and Vaseline gauze molding—were performed according to each classified type of deformity encountered.
Antihelical Tubing Using MS
The antihelix and superior crus were recreated through one to four MS according to the severity of protrusion. One MS (tubing only the superior crus) was effective for non-protruding ears with moderate superior helical lidding to correction. With the temporary manual molding simulation, a peak line of the ideal antihelix was marked using methylene blue on the medial side of the auricle. A syringe needle with methylene blue was used to pierce the skin and the full layer of cartilage at the designed peak points, marking the antihelical tubing position (Fig. 3, above left). Then, MS were performed using 3–0 nylon to reversely fold the protruding or flatten cartilage to reconstruct the antihelix (Fig. 3, above right; Fig. 4, above).
Reconstruction of antihelix through Mustardé sutures (above) or tumbling CF Procedure (below), auricular cartilage with blue color. (Above, right) Axial view of suture placement through the cartilage. (Above, left) Placement of three permanent, horizontal mattress sutures. Below, the horizontal section of the constricted ear. (Below, left) preoperative view. (Below, middle) skin between the points labeled A and B was excised. The CF (black arrow) was formed. (Below, right) The CF was folded, and the new antihelix (black arrow) was rebuilt. Then, the skin was sutured, and point A and point B merged into the same point, resulting in the compound structure of helix and scapha backward (red arrow).
Tumbling CF Procedure
Postauricular skin was excised along the designed line. A cartilage truncation incision was designed in the posterior auricular cartilage 5–8 mm from the rim of helix. The entire layer of the cartilage was cut through. The anterior skin was undermined to the external border of the antihelix. A fan-shaped CF was formed (Fig. 3, below), and the surface of the CF was superficially scored. When the CF was turned over and sutured to the cartilage below, the superior crus and the antihelix were formed by the tumbling rim of the CF (Fig. 4, below). The compound structure of the helix and scapha was pushed backward to reach the CF.
Helical Expansion Using Folded Cartilage, Concha Cartilage, or Costal Cartilage
When the folded helical cartilage was remanent, a free-floating folded helical cartilage flap was transplanted to expanse the helical rim. Its independent use appeared only in the condition of mild cartilage defects. Ordinarily, the folded helical cartilage only played a supplementary role due to its limitation. When it was obvious that constricted ears (type IIA and type IIB) were caused by a shortage of the helix and adjacent structure, free-floating concha cartilage flap or costal cartilage strip was more frequently performed to achieve the goal of helical expansion (Fig. 5).
Operative procedure showing the helical expansion technique using a free-floating concha flap (above, type IIA) or costal cartilage strip (below, type IIB). The dotted line indicates the size of normal auricle. The primary auricle cartilage in a light blue color; and the cartilage graft in a dark blue color. Above second from left, the harvest of a concha cartilage flap; below second from left, the harvest of a costal cartilage strip. Above second from right, a concha cartilage flap grafting; below second from right, a costal cartilage strip grafting.
A concha cartilage flap (above the cranioauricular sulcus of the deformed ear) of exact size (usually range 0.5–0.8cm×1.5–2cm) was obtained, while taking care to avoid piercing the concha cavity. When more than one piece of concha cartilage flap was required under a certain condition, it could be obtained from the concha of the healthy ear. One or two concha cartilage flaps (inlay graft) were attached to the deficient point on the helical rim to provide additional support and expansion in the upper third of the ear. Simple interrupted suture using 5–0 absorbable suture was performed for fixation, then the skin covered.
In addition, costal cartilage with nice strength was also an ideal support for surgeons and patients to choose. On the lowermost costal margin, a skin incision of approximately 2.5 cm was made, and a costal cartilage strip (8th or 9th) with the perichondrium was harvested. An ideal costal cartilage strip typically measured five to six centimeters in length, showing a spontaneously curved shape. Then, the split rib cartilage was attached to the helical rim. Reconstruction of helix corrected the upper lidding and increased the height of the constricted ear.
Elevation of Triangular Superficial Temporal Fascial Flap
Subcutaneous dissociation was performed using a No. 15 surgical round blade on the upper back of the auricle to obtain a triangular superficial temporal fascia flap with a side length of approximately 1–1.5 cm (Fig. 6). The triangular apex of the superficial temporal fascial flap was elevated to the cartilage of the upper auricle to correct its protrusion and prevent recurrence in the long run. Therefore, this procedure was performed in constricted ears with obvious protrusion of the upper pole of the ear.
External Molding Using Vaseline Gauze
Vaseline gauze was applied and modeled into rolls (measuring 5–10 cm in length) with a certain hardness to maintain the ear the desired shape. Roll of 5 cm was used for the deformity with reconstruction of only antihelical superior crus (Fig. 6). This procedure can be applied to all types of constricted ears.
Result
Of the 57 patients (68 constricted ears) enrolled in the study, 33 (57 percent) were male and 46 (79 percent) had unilateral deformity (right, n = 29; left, n = 17). The severity of constricted ears was classified according to the classification showed above (Table. 1) (type I, n = 6; type IIA, n = 41; type IIB, n = 19, and type III, n = 2). Among 11 cases with bilateral constricted ears, 3 patients showed different types between two ears. Only 2 type III constricted ears (corrected by auricular reconstruction without presence in this article) were combined by contralateral type IIB deformities. Four patients with unilateral constricted ears present contralateral other auricular abnormalities, including prominent ear (n = 2), polyotia (n = 1), and lobule-type microtia (n = 1). Three ears with histories of previous operations at other clinics underwent secondary operation: all of them were type IIA. 11 constricted ears (16 percent of all enrolled 68 constricted ears) present other ipsilateral accompanying anomalies, including preauricular fistula (n = 6), accessory auricle (n = 3),lobule aplasia (n = 3), and tragus abnormalities (n = 2), as each constricted ear could have more than one associated anomaly (Table 2).
Surgical Techniques Used in Each Graded Type, and Their Esthetic Outcomes
Of the 66 constricted ears undergoing correction, most of them were performed with helical expansion through auricular/costal cartilage graft, Mustardé-type mattress sutures, and tumbling cartilage flap, as showed from Fig. 7 to Fig. 10. External molding using Vaseline gauze rolls was implemented on every case to assist reshaping the scapha. A triangular superficial temporal fascial flap was elevated to prevent the reoccurrence of lidding in some cases. The average esthetic outcome score was 3.7, as shown in Table 3. Surgical procedures performed in each type deformed ears are shown in Table 4 through Table 6.
Complications
Of all 66 constricted ears, 5 cases (type IIA, n = 4; type IIB, n = 1) present auricular complications, including local congestion and (or) swelling, lidding relapse, and antitragus pinching deformity (Fig. 11). Correcting techniques performed in those cases and treatment effects are shown in Table 7.
Disccusion
Constricted ears are characterized by four components: lidding, protrusion, decreased ear size, and low ear position. The appearance of constricted ears is highly heterogeneous, that’s why the deformities have been graded by many clinical experts from different perspectives and consideration according to their practical experience [1,2,3, 6]. It was hard to identify some type IIA deformities from type IIB deformities, as their difference was defined as the requirement of skin supplementation. Therefore, it is of practical significance to regard the corrective outcome of surgical procedures as a consideration in the classification of constricted ears. Additionally, according to the classification of this study, some type I cases (Fig. 2 type I, first and second from right) were not suitable to Musgrave correction [10] for group IIA (involvement of helix and scapha) according to Tanzer’s classification, as those two deformed auricles featured by the lidding (obviously in right side view) but not cartilage deficiency.
This study was deliberately concerned about the correction of disfigured cartilage framework during surgical procedures, such as helical expansion, reconstruction of antihelix, elevation of TF flap, and Vaseline gauze molding. In addition to congenital conditions of the deformed ear, the following factors also play an important role in the selection of surgical procedures, including: (1) condition of the contralateral ear; (2) condition of the costal cartilage; (3) the ability and experience of surgeons; (4) the opinion of the patients or families. Since the symmetry of bilateral ears is an important index to evaluate the esthetic effect after surgery, it is essential to consider the size and height of the opposite ear. Coastal cartilage is not recommended for patients who are too young (less than 5 years old), as well as elderly patients due to calcification of rib cartilage. Otherwise, for type IIB constricted ears, costal cartilage grafts for helical expansion could achieve better outcome than auricle cartilage, but some parents still choose concha cartilage in consideration of low risk, small trauma, short hospital stay and so on, which differed from reports of other clinics. For esthetic effect, the difference of bilateral auricle size after correction in the case of unilateral type IIB constricted ear was identified to be less than 1/3, which is not easily noticed by a casual glance. Although simple addition of pieces of cartilage could not reach the size of the normal auricle, it met daily needs, such as wearing glasses and masks.
Costal cartilage grafting was not recommended for type IIB constricted ear (Fig 2IIB, first from right, also called concha-type microtia) in 1–3 years old patients. In addition to the factor of costal cartilage, the normal development of the auricle was also taken into account. For these constricted ears, the goal of surgical correction is not only to increase their size, but also to correct the angulated helical cartilage and reconstruct helix so that the auricle can grow following a related normal shape.
Generally speaking, since children’s ear cartilage is relatively soft and easy to fold, Mustarde suture is mostly applied to young patients in our practice. In tumbling CF procedure, the entire deformed cartilage layer is dissected in a designed position to eliminate its reverse tension and scratches on the anterior CF are made to increase the compliance of the cartilage for easy folding. Tumbling CF can achieve a firmer effect when creating antihelix. Therefore, the tumbling CF technique is recommended for adult patients to reduce the risk of recurrent ear deformity as their developed ear cartilage is harder and less compliant. But one case presented pinching deformity at the position of antitragus in a follow-up period. Otherwise, a triangular superficial temporal fascia flap was elevated to the cartilage of the upper auricle to prevent protrusion and lidding recurrence. For better secrecy, the incision was usually made behind the ear or on the outer rim of the helix. There was usually no obvious incision on the inner side of the auricle.
In addition, blood circulation disorder in the flap is an event we need to avoid. In our experience, the flap length to width ratio less than 1:2 can avoid dry necrosis caused by insufficient arterial blood supply. At the same time, the excessively narrow pedicle of the flap should be avoided to prevent congestion. When the necrosis occurs, if the exposed area of cartilage does not exceed the size of "soybean," it can usually be gradually recovered by debridement and dressing change and no more operative procedure is required.
Limitation of this study was the relatively short follow-up period. Several practical and social factors resulted this phenomenon. As the most authoritative plastic surgery hospital in China, most of patients presented our clinic for treatment from various provinces and cities, so follow-up throughout China is difficult. Postoperative data of this study were mostly collected at the time of suture removal or their return visit, in a face-to-face manner. Besides, esthetic assessment requires multi-angle vision and requires the photographer to have a certain professional consciousness, so the result of remote assessment using photos taken by patients is not accurate. Furthermore, the COVID-19, which has continued since the beginning of 2020, also increased the difficulty of follow-up.
Conclusion
A total of 68 constricted ear cases, distinct from cases corrected by auricular reconstruction, have been analyzed. The deformed ears were classified into three graded types and two sub-types determined by deficiency of auricle cartilage, vertical height and surgical outcome. Each type of constricted ear was effectively corrected by operative techniques. All corrections were performed in one stage, without removal of deformed auricular cartilage.
References
Cosman B (1978) The constricted ear. Clin Plast Surg 5(3):389–400
Tanzer RC (1975) The constricted (cup and lop) ear. Plast Reconstr Surg 55:406–415
Park C, Park JY (2016) Classification and algorithmic management of constricted ears: a 22-year experience. Plast Reconstr Surg. 137:1523–1538
Kon M, van Wijk MP (2014) T-bar reconstruction of constricted ears and a new classification. J Plast Reconstr Aesthet Surg 67:358–361
Lee JS, Kim JS, Lee JW, Choi KY, Yang JD, Chung HY, Cho BC (2020) Correction of microtia with constriction features using a superficial temporal fascial flap combined with a rib cartilage graft. Arch Plast Surg. 47(4):317–323
Nagata S (2002) Alternative surgical methods of treatment for the constricted ear. Clin Plast Surg 29:301–315
Wilkes GH, Wong J, Guilfoyle R (2014) Microtia reconstruction. Plast Reconstr Surg 134:464e–479e
Nagata S (1994) Modification of the stages in total reconstruction of the auricle: Part I. Grafting the. three-dimensional costal cartilage framework for lobule-type microtia. Plast Reconstr Surg. 93: 221–230; discussion 267–268
Firmin F (2010) State-of-the-art autogenous ear reconstruction in cases of microtia. Adv Otorhinolaryngol 68:25–52
Musgrave RH (1966) A variation on the correction of the congenital lop ear. Plast Reconstr Surg 37:394–398
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Ethical Approval
The study was authorized by our institution’s ethics committee and followed the World Medical Association Declaration of Helsinki.
Informed Consent
All study participants provided written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huang, X., Ma, C., Chang, J. et al. Classification and Surgical Strategies of Constricted Ears in a Chinese Specialty Clinic: A Retrospective Study. Aesth Plast Surg 46, 2194–2207 (2022). https://doi.org/10.1007/s00266-021-02699-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-021-02699-1