Abstract
Introduction
The recent finding that shrinkage of key areas of the facial skeleton contributes to the aging appearance of the face has prompted a search for the most appropriate bone-like implant material. Evidence that hydroxyapatite, in granular form, maintains volume in the long term supports its use in the correction of aging, in addition to its use in the correction of inherently deficient areas of the facial skeleton. The biologic response of hydroxyapatite needs to be fully understood for its use to be confidently recommended.
Materials and Methods
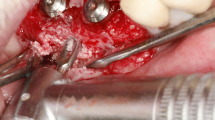
Samples of ‘living’ hydroxyapatite from the anterior maxilla, zygoma, and mandible of 17 patients were analyzed. These were obtained during revision procedures performed between 6 months and 15 years following original placement on the facial skeleton.
Results
Histology showed that in every case, the individual granules were embedded within a mass of collagen that made up about half of the total implant volume. The collagen mass also contained fine elastin, fibroblasts, lymphocytes, occasional granulomas, and vessels. By 2 years, a new compact bone containing osteoblasts and osteocytes was present in all specimens in the deep (osseous) aspect. Bone progressively replaced the original collagen between the granules with a sharply defined transition at the interface.
Conclusions
This study confirmed a two-stage biologic change following onlay placement of hydroxyapatite granules on the facial skeleton, i.e., initial collagen formation with subsequent conversion to bone. This integrates the implant with the host bone which stabilizes the implant position and shape initially and in long term.
No Level Assigned
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors.www.springer.com/00266.






Similar content being viewed by others
References
Baines FW, Elia FP (1996) Facial skeletal augmentation with hydroxyapatite granules. Churchill Livingstone, New York
Bonucci E, Marini E et al (1997) Osteogenic response to hydroxyapatite-fibrin implants in maxillofacial defects. Eur J Oral Sci 105:557–561
Byrd HS, Hobar PC, Shewmake K (1993) Augmentation of the craniofacial skeleton with porous hydroxyapatite granules. Plast Reconstr Surg 91:15–22 (Discussion 23–16)
el Deeb M, Roszkowski M (1988) Hydroxylapatite granules and blocks as an extracranial augmenting material in rhesus monkeys. J Oral Maxillofac Surg 46:33–40
Drobeck HP, Rothstein SS, Gumaer KI, Sherer AD, Slighter RG (1984) Histologic observation of soft-tissue responses to implanted, multifaceted particles and discs of hydroxylapatite. J Oral Maxillofac Surg 42:143
Farrior RT (1966) Implant materials in restoration of facial contour. Laryngoscope 76:934–954
Fortunato G, Marini E (1997) Long-term results of hydroxyapatite-fibrin glue implantation in plastic and reconstructive craniofacial surgery. J Cranio Maxfac Surg 35:124–135
Frame JW, Brady CL (1987) The versatility of hydroxyapatite blocks in maxillofacial surgery. Br J Oral Maxillofac Surg 25:452–464
Harvey WK, Pincock JL, Matukas VJ, Lemons JE (1985) Evaluation of subcutaneously implanted hydroxyapatite-avitene mixture in rabbits. J Oral Maxillofac Surg 43:277
Hinderer UT (1971) Profileplasty. Int Microbiol J Aesthet Plast Surg. doi:10.1007/BF01570230
Hobar PC, Pantaloni M, Byrd HS (2000) Porous hydroxyapatite granules for alloplastic enhancement of the facial region. Clin Plast Surg 27:557–569
Holmes RE (1979) Bone regeneration within a coralline hydroxyapatite implant. Plast Reconstr Surg 63:626
Holmes RE, Mooney V, Bucholz R, Tencer AA (1984) Coralline hydroxyapatite bone graft substitute. Clin Orthop 188:252
Hulbert SF, Young FA, Mathews RS et al (1970) Potential of ceramic materials as permanently implantable skeletal prosthesis. J Biomed Mater Res 4:433–456
Ingram AE Jr, Robinson J, Rohrich RJ (1996) The antibacterial effect of porous hydroxyapatite granules. Plast Reconstr Surg 98:1119
Junqueira LC, Carneiro J, Kelley RO (eds) (1992) Basic histology. Appleton & Lange, London, pp 141–162
Kent JN, Quinn JH, Zide MF, Finger IM, Jarcho M, Rothstein SS (1992) Correction of alveolar ridge deficiencies with nonresorbable hydroxylapatite. J Am Dent Assoc 105:993–1001
Lineham R (1974) Hydroxyapatite formed from coral skeletal carbonate by hydrothermal exchange. Nature 247:220–222
Meijer HJ, Steen WH, Bosman F, Wittkampf AR (1997) Radiographic evaluation of mandibular augmentation with prefabricated hydroxylapatite/fibrin glue implants. J Oral Maxillofac Surg 55:138–144
Mendelson BC, Jacobson SR, Laviopierre AM, Huggins RJ (2010) The fate of hydroxyapatite granules used in facial skeletal augmentation. Aesthet Plast Surg 34:455–461
Mendelson BC, Wong CH (2012) Changes in the facial skeleton with ageing: implications and applications in facial rejuvenation. Aesth Plast Surg 36:753–760
Misiek DJ, Kent JN, Carr RF (1984) Soft-tissue responses to hydroxylapatite particles of different shapes. J Oral Maxillofac Surg 42:150
Moreira-Gonzalez A, Jackson IT, Miyawaki T, Dinick V, Yavuzer R (2003) Augmentation of the craniomaxillofacial region using porous hydroxyapatite granules. Plast Reconstr Surg 111:1808–1817
Pettis GY, Kaban LB, Glowacki J (1990) Tissue response to composite ceramic hydroxyapatite/demineralized bone implants. J Oral Maxillofac Surg 48:1068–1074
Piecuch JF, Fedorka NJ (1983) Results of soft-tissue surgery over implanted replamine from hydroxyapatite. J Oral Maxillofac Surg 41:80
Piecuch JF, Goldberg AJ, Shastry CV, Canowski RB (1984) Compressive strength of implanted porous replamine from hydroxyapatite. J Biomed Mater Res 18:39
Pollick S, Shors EC, Holmes RE, Kraut RA (1995) Bone formation and implant degradation of coralline porous ceramics placed in bone and ectopic sites. J Oral Maxillofac Surg 53:915–922 (Discussion 922–913)
Rees TD, Wood Smith D (1973) Cosmetic facial surgery, 1st edn. Saunders, Philadelphia
Rubin JP, Yaremchuk MJ (1997) Complications and toxicities of implantable biomaterials used in facial reconstructive and aesthetic surgery. Plast Reconstr Surg 100:1336–1353
Salyer KE, Hall CD (1989) Porous hydroxyapatite as an onlay bone graft substitute for maxillofacial surgery. Plast Reconstr Surg 84:236–244
Sari A, Yavuzer R, Ayhan S, Tuncer S, Latifoglu O, Atabay K, Celebi MC (2003) Hard tissue augmentation of the mandibular region with hydroxyapatite granules. J Craniofac Surg 14:919–923
Scales JT, Winter GD (1975) Clinical considerations in the choice of materials for orthopedic internal prostheses. J Biomed Mater Res 9:167–176
Terino EO, Flowers RS (2000) The art of alloplastic facial contouring. Mosby, St. Louis
Wolfe SA (1982) Autogenous bone grafts versus alloplastic material in maxillofacial surgery. Clin Plast Surg 9:539–540
Acknowledgments
The authors wish to thank Professor Jeffrey Kerr of Monash University, Department of Anatomy, Australia for his expertise and assistance in the interpretation of the histology.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no commercial or financial interest in any of the materials or apparatus detailed in this study.
Rights and permissions
About this article
Cite this article
Huggins, R.J., Mendelson, B.C. Biologic Behavior of Hydroxyapatite Used in Facial Augmentation. Aesth Plast Surg 41, 179–184 (2017). https://doi.org/10.1007/s00266-016-0707-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-016-0707-9