Abstract
Purpose
The aim of this prospective randomized study was to evaluate whether the use of the anatomic double-bundle (DB) method for anterior cruciate ligament (ACL) reconstruction results in better clinical outcomes and a lower incidence of graft failure compared with the anatomic single-bundle (SB) method. The hypothesis was that DB ACL reconstruction would result in a lower incidence of graft failure.
Methods
Patients were randomly assigned to either the SB group (n = 78) or the DB group (n = 75). Evaluation included clinical testing, subjective assessments, functional testing, and International Knee Documentation Committee (IKDC) objective grading. Surgical techniques were anatomic, and the rehabilitation protocol was standardized.
Results
At 15-year follow-up, information was available on 100 patients (65%), of whom 55 (36%) were accepted in the final statistical analysis. There were almost three times as many graft failures in the SB group, but the result wasn´t statistically significant. Subjective assessments, knee stability (KT -1000 and pivot shift), range of motion (ROM), and functional one leg hop test showed no statistically significant differences between the groups. However, DB ACL reconstruction resulted in better International Knee Documentation Committee objective grading (P < 0.001).
Conclusion
At the 15-year follow-up, double-bundle surgery resulted in significantly better International Knee Documentation Committee objective grading compared to single-bundle surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anterior cruciate ligament reconstruction is a common surgical procedure to restore knee stability and prevent further injury after ACL tear [1, 2]. The SB technique, which is the most performed procedure and considered the gold standard, uses a single graft to reconstruct the ACL, whereas the DB technique uses two grafts to separately reconstruct the anteromedial and posterolateral bundles of the ACL [3,4,5]. The debate about which technique is better has been ongoing for many years, with studies reporting contradictory results [6,7,8,9,10]. Our meta-analysis [11] found that DB ACL reconstruction generally results in better restoration of knee laxity and subjective outcomes than SB ACL reconstruction.
Long-term graft failure after ACL reconstruction is estimated to occur in 5–6% of patients [12, 13]. For example, male gender, younger age, a family history of ACL injury, greater tibial slope and return to high activity sports are associated with an increased risk of graft failure [14, 15]. The surgical technique of the ACL also seems to have an influence on the graft failure rate [16, 17].
The purpose of this randomized clinical trial was to evaluate whether the use of the anatomic DB method for ACL reconstruction with hamstring autograft and aperture screw fixation results in better clinical outcomes and a lower incidence of graft rupture compared with the anatomic SB method with hamstring autograft and aperture screw fixation. The study followed patients over a 15-year period and aimed to test this hypothesis.
Material and methods
Patients
Ethics Committee of Tampere University Hospital approved the study, and all patients provided written informed consent before participation. Baseline data were collected between 4/2003 and 2/2008 at Hatanpää Hospital, Tampere, Finland. To be eligible for the study, patients had to meet certain inclusion criteria, including a primary ACL reconstruction, closed growth plates, and no ligamentous injuries to the contralateral knee. The inclusion period was 4.8 years and all patients who met the three inclusion criteria were included in the study. In total, 153 patients were randomly assigned to two different groups for ACL reconstruction with hamstring autografts: the anatomic SB technique with interference screw fixation group (n = 78) and the anatomic DB technique with interference screw fixation group (n = 75). Randomization was performed with closed opaque envelopes. Patients were not blinded to the surgical technique, but were not allowed to reveal the surgical technique to the investigator. All surgical procedures were performed by a single experienced orthopaedic surgeon TJ.
Evaluation
The evaluation included clinical tests (pivot shift, ROM, anterior tibial translation measured with the arthrometer KT-1000), IKDC objective grading (based on the IKDC knee examination form [18]), subjective assessments (IKDC subjective score, IKDC function score, and Lysholm score), and functional test (one leg hop). The IKDC subjective score is based on the IKDC subjective knee evaluation form [18] and the IKDC function score is the last part of this form. The number of graft failures was assessed by revision surgery. The KT-1000 arthrometer (MEDmetric Corp, San Diego, CA, USA) with a force of 134 N was used. For ROM, the result of the operated leg was compared with that of the non-operated leg. The ROM included lack of passive extension (normal < 3°, nearly normal 3–5°, abnormal 6–10°, and severely abnormal > 10°) and lack of passive flexion (normal 0–5°, nearly normal 6–15°, abnormal 16–25°, and severely abnormal > 25°). One leg hop test was performed to assess the functional capacity of the knee. The patient hopped a maximum length three times on each leg separately and the best result was recorded for both legs. The result of the operated leg was then compared with that of the non-operated leg. The categories were normal (≥ 90%), nearly normal (89–76%), abnormal (75–50%), and severely abnormal (< 50%). All clinical assessments were performed by a blinded and independent investigator AS. Preoperatively, patients' physical demands were rated 1–3 (1 = competitive sport, 2 = recreational sport, 3 = no sport).
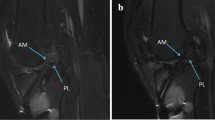
Surgical technique of the double-bundle ACL reconstruction
TJ has previously explained the surgical technique of double-bundle ACL reconstruction in detail elsewhere [19]. Briefly, this procedure first involved comprehensive diagnostic arthroscopic surgery of the knee. This step confirmed the presence of ACL tears and assessed the condition of the meniscus and cartilage. The torn portion of the ACL was then removed, but the tibial attachment site was left intact. No bony notchplasty was performed. Two tunnels were then created on the femoral side through an anteromedial portal (not through the tibia). These tunnels were created manually without a guide to ensure they corresponded to the anatomic position of the insertion site of each bundle. On the tibial side, the tunnels were created using a guide to ensure they matched the anatomic insertion site of the ACL at the tibia. The hamstring grafts (semitendinosus and gracilis) for the procedure were then harvested from the same leg and doubled. These doubled grafts were inserted through the tibial tunnels in a reverse fashion and secured with bioresorbable (specifically D-lactide, L-lactide, and trimethylene carbonate [TMC]) interference screws (Inion Hexalon, Inion Oy, Tampere, Finland). The femoral side was fixed from the inside out, whereas the tibial side was fixed from the outside in.
Surgical technique of the single-bundle ACL reconstruction
Initially, a diagnostic arthroscopic procedure and debridement were performed as described above. The femoral tunnel was created using an anteromedial portal. A freehand technique was used, and the tunnel was positioned at approximately 10 o’clock in the right knee and at 2 o’clock in the left knee. For the tibial tunnel, a tibial guide was used to ensure it was positioned at the midpoint of the tibial ACL attachment site. The tendons of the semitendinosus and gracilis muscles were then harvested, doubled over, and inserted through the tibial tunnel, extending into the femur, and fixed with metallic (Timoni Company, Kauniainen, Finland) or bioabsorbable interference screws (Inion Hexalon). Both tendons were always harvested and used with both techniques.
Postoperative rehabilitation
The two groups underwent the same rehabilitation protocol, which included unrestricted range of motion and full weight bearing without a brace. Patients used crutches for three to four weeks and began closed kinetic chain exercises immediately after surgery. They were allowed to begin cycling with an ergometer bicycle after four weeks, running after three months, and pivoting sports after six months postoperatively, provided they had regained full muscle strength and functional stability. If the patient had also undergone meniscal repair during surgery, a range of motion of 0° to 90° was recommended for the first six weeks. Otherwise, rehabilitation was performed according to the methods described above.
Statistical analysis
Statistical analysis was performed using SPSS version 28.0 (IBM Corporation, Armonk, NY, USA). As all distributions were skewed, the Mann–Whitney U test was used. Frequencies were analyzed with the chi-square test. The significance level was set at P < 0.05. Median and IQR were used to describe skewed distributions. To define the minimal clinically important difference (MCID), threshold values of 1 standard error of measurement (SEM), 1.96 SEM, and 2.77 SEM were calculated independently for both groups [20].
Results
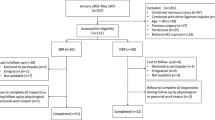
At 15-year follow-up, information on 100 patients (65%), 57 patients from the SB group (73%) and 43 patients from the DB group (57%), was available (Fig. 1). In the SB group, 13 patients (17%) underwent revision surgery because of graft failure, whereas the corresponding number of graft failures in the DB group was five (7%) (n.s.). During the 15-year follow-up period, 11 patients in each group sustained ACL tear in the contralateral knee. Moreover, four patients (5%) in the SB group and one patient (1%) in the DB group underwent total knee replacement (n.s.). Thus, 29 patients from the SB group and 26 patients from the DB group were accepted for statistical analysis. There was no difference in physical demands between the groups (n.s.). Patient demographics are presented in Table 1. The surgical findings of the two study groups are presented in Table 2. The median and mean of the follow-up time were 16.3 years (14.6–17.1) and 15.9 years (1.4), respectively.
The median scores for the IKDC subjective assessment were 85 (78–95) in the DB group and 82 (65–94) in the SB group. Similarly, for the Lysholm score, the median score was 90 (83–97) in the DB group and 89 (76–94) in the SB group. Moreover, the median IKDC function score was eight (7–10) in the DB group and 8 (7–9) in the SB group. No statistically significant differences were found in any of these scores at 15-year follow-up (Table 3).
Anterior tibial translation was measured with the KT -1000 arthrometer. The median difference (index minus opposite) was 1 mm in both groups, and the IQR was -1 to 2 mm in the SB group and 0 to 2 mm in the DB group (n.s.). Knee rotational stability was assessed with the pivot shift test. In total, 23 (79%) patients in the SB group and 23 patients (89%) in the DB group had a negative pivot shift test result (n.s.). However, DB ACL reconstruction resulted in better results in IKDC objective grading (P < 0.001). In the DB group, 12 patients (46%) had a normal IKDC objective grading, whereas the corresponding result in the SB group was 1 (3%).
In the DB group, 18 patients (69%) had normal passive extension, whereas 21 (75%) patients had normal passive extension (n.s.) in the SB group. Regarding passive flexion, 19 patients (73%) in the DB group and 15 patients (52%) in the SB group had normal results (n.s.).
One leg hop test was performed to assess the functional capacity of the knee. A total of 21 patients (81%) in the DB group and 16 patients (57%) in the SB group had normal functional results (n.s.). The 15-year follow-up results were significantly better in both groups compared with the preoperative situation in terms of Lysholm score, IKDC function score, IKDC objective grading, and stability measurements (P < 0.001).
The percentage of patients achieving the MCID for the Lysholm score was 72% (1 SEM), 72% (1.96 SEM) and 69% (2.77 SEM) in the SB group and 73% (1 SEM), 62% (1.96 SEM) and 58% (2.77 SEM) in the DB group. Correspondingly, the percentage of patients achieving the MCID for the IKDC functions score was 86% (1 SEM), 79% (1.96 SEM) and 79% (2.77 SEM) in the SB group and 81% (1 SEM), 81% (1.96 SEM) and 77% (2.77 SEM) in the DB group.
Discussion
The main finding of the present 15-year follow-up study was that the double-bundle technique resulted in better IKDC objective grading compared with singe-bundle technique. IKDC objective grading considers the measured variables as a whole. The differences appeared to come primarily from the results of ROM, although there were no statistically significant differences in passive extension or passive flexion. In addition, there were twice as many positive pivot shift test results in the SB group as in the DB group. One possible explanation for this statistically significant result in IKDC objective evaluation could be that the knees in the DB group are more stable and have a better range of motion than the knees in the SB group, although no statistically significant differences were found when the outcomes were analyzed separately. To our knowledge, similar findings comparing anatomic DB reconstruction with anatomic SB reconstruction at mid- or long-term follow-up have not previously been published.
Anterior stability results, measured with the KT-1000 arthrometer, were equal between the groups. In summary, no statistically significant difference was found between the groups in knee stability, including pivot shift test. In their long-term study, Balasingam et al. [21] reported similar results to those in our study. In contrast, Mao et al. [22]found better knee stability results in the DB group compared to the SB group in their long-term retrospective study.
Suomalainen et al. used the same research population as in the present study in their two year follow-up study in 2011, [23] and their main finding was that there were fewer graft failures in the DB group (n = 1) than in the SB group (n = 7) (P = 0.04). Similar results were also obtained in 2012 [24] and 2017 [17] when they had partially the same study population. After 15 years of follow-up, there were nearly three times as many graft failures in the SB group, but the result was no longer statistically significant. This result included previously observed graft failures from previous trials, [17, 23, 24] even if patients had not participated in the 15-year trial. The graft failures in the SB group were all caused by a minor accident. One graft failure in the DB group was due to major trauma with bone fractures, while the others were caused by a minor accident. The tunnel positions of these patients were examined by MRI at the 2-year follow-up and/or at the ACL revision surgery and were all adequate [25, 26]. If only graft failures stemming from minor trauma were considered, a statistically significant difference between the groups emerged. In their RCT study with a five year follow-up, Mohtadi et al. [27] found that graft failure occurred in fewer patients in the patellar tendon SB group than in the hamstring tendon SB and hamstring tendon DB groups.
At two year follow-up [23], seven patients (2 in the DB group and 5 in the SB group) had an invisible graft on MRI assessment. At the 15-year follow-up, two of these patients had undergone total knee replacement, 1 patient (DB) had undergone revision surgery, three patients were accepted for statistical analysis, and one patient (DB) was excluded from statistical analysis because of a contralateral ACL injury. At the two year follow-up, the MRI findings of the invisible grafts appeared to have no clinical significance, but at the 15-year follow-up, one of them had undergone revision surgery and two had undergone total knee replacement, so the invisible graft appeared to have long-term clinical significance in at least some of the patients (3/7).
Subjective assessments of the condition of the knees are one of the most important outcomes when the follow-up period becomes longer. All three subjective assessment forms were better in the DB group, although only slightly. However, a statistically significant difference could not be shown in subjective evaluation. Xu et al. have reported similar results in their new meta-analysis [28] which includes only anatomical ACL reconstructions. However, Eliya et al. found that anatomical DB ACL reconstruction moderately improved Tegner scores over the long term [29].
The major limitation of our study was the relatively low follow-up rate (65%), which can add attrition bias to the study. However, with a follow-up period of 15 years, it is difficult to get patients to participate in the study. Some of the patients became bored with the study, some moved abroad or to a more distant location, and at least one patient died. In addition, the research material was collected during the COVID -19 pandemic, which may have reduced the enthusiasm of patients to participate in the study. Furthermore, because only a few patients were included in the statistical analysis at 15 years, the differences between the groups had to be large for the results to be statistically significant.
The strength of the study was the long follow-up period of 15 years and a study design based on an RCT with a blinded examiner. To date, the follow-up period of our study is the longest on the topic of SB versus DB ACL reconstruction.
Since the ACL DB technique appeared to achieve a better result than the SB technique even at 15-year follow-up, its use in ACL reconstruction is recommended option for conventional SB technique. However, it should be borne in mind that the DB technique is more demanding to perform than the SB technique and is therefore only suitable for experienced ACL surgeons.
Conclusion
The main finding of this 15-year follow-up study was that the double-bundle technique resulted in better IKDC objective grading. Otherwise, no difference between the groups was demonstrated.
Data availability
Only members of the research group have access to the data.
Code availability
Statistical analysis was performed using SPSS version 28.0 (IBM Corporation, Armonk, NY, USA).
Abbreviations
- DB :
-
Double-bundle
- ACL :
-
Anterior cruciate ligament
- SB :
-
Single-bundle
- RCT :
-
Randomized controlled trial
- IKDC :
-
International knee documentation committee
- ROM :
-
Range of motion
- SEM :
-
Standard error of measurement
- MCID :
-
Minimal clinically important difference
- n.s . :
-
Not significant
References
Herzog MM, Marshall SW, Lund JL, Pate V, Mack CD, Spang JT (2017) Incidence of anterior cruciate ligament reconstruction among adolescent females in the United States, 2002 Through 2014. JAMA Pediatr 171:808–810. https://doi.org/10.1001/jamapediatrics.2017.0740
Mall NA, Chalmers PN, Moric M, Tanaka MJ, Cole BJ, Bach BR Jr et al (2014) Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med 42:2363–2370. https://doi.org/10.1177/0363546514542796
Fujita N, Kuroda R, Matsumoto T, Yamaguchi M, Yagi M, Matsumoto A et al (2011) Comparison of the clinical outcome of double-bundle, anteromedial single-bundle, and posterolateral single-bundle anterior cruciate ligament reconstruction using hamstring tendon graft with minimum 2-year follow-up. Arthroscopy 27:906–913. https://doi.org/10.1016/j.arthro.2011.02.015
Hussein M, van Eck CF, Cretnik A, Dinevski D, Fu FH (2012) Prospective randomized clinical evaluation of conventional single-bundle, anatomic single-bundle, and anatomic double-bundle anterior cruciate ligament reconstruction: 281 cases with 3- to 5-year follow-up. Am J Sports Med 40:512–520. https://doi.org/10.1177/0363546511426416
Ibrahim SA, Hamido F, Al Misfer AK, Mahgoob A, Ghafar SA, Alhran H (2009) Anterior cruciate ligament reconstruction using autologous hamstring double bundle graft compared with single bundle procedures. J Bone Joint Surg Br 91:1310–1315. https://doi.org/10.1302/0301-620x.91b10.21886
Chen H, Chen B, Tie K, Fu Z, Chen L (2018) Single-bundle versus double-bundle autologous anterior cruciate ligament reconstruction: a meta-analysis of randomized controlled trials at 5-year minimum follow-up. J Orthop Surg Res 13:50. https://doi.org/10.1186/s13018-018-0753-x
Dong Z, Niu Y, Qi J, Song Y, Wang F (2019) Long term results after double and single bundle ACL reconstruction: Is there any difference? A meta - analysis of randomized controlled trials. Acta Orthop Traumatol Turc 53:92–99. https://doi.org/10.1016/j.aott.2018.12.004
Maestro A, Herruzo I, Varillas-Delgado D, Martín-Saborido C (2021) Subjective assessment reported by patients shows differences between single-bundle and double-bundle anterior cruciate ligament reconstruction, systematic review and meta-analysis. Sci Rep 11:15385. https://doi.org/10.1038/s41598-021-94868-0
Xu M, Gao S, Zeng C, Han R, Sun J, Li H et al (2013) Outcomes of anterior cruciate ligament reconstruction using single-bundle versus double-bundle technique: meta-analysis of 19 randomized controlled trials. Arthroscopy 29:357–365. https://doi.org/10.1016/j.arthro.2012.08.024
Zhu Y, Tang RK, Zhao P, Zhu SS, Li YG, Li JB (2013) Double-bundle reconstruction results in superior clinical outcome than single-bundle reconstruction. Knee Surg Sports Traumatol Arthrosc 21:1085–1096. https://doi.org/10.1007/s00167-012-2073-8
Seppänen A, Suomalainen P, Huhtala H, Mäenpää H, Kiekara T, Järvelä T (2022) Double bundle ACL reconstruction leads to better restoration of knee laxity and subjective outcomes than single bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 30(5):1795–1808. https://doi.org/10.1007/s00167-021-06744-z
Crawford SN, Waterman BR, Lubowitz JH (2013) Long-term failure of anterior cruciate ligament reconstruction. Arthroscopy 29:1566–1571. https://doi.org/10.1016/j.arthro.2013.04.014
Sanders TL, Pareek A, Hewett TE, Levy BA, Dahm DL, Stuart MJ, Krych AJ (2017) Long-term rate of graft failure after ACL reconstruction: a geographic population cohort analysis. Knee Surg Sports Traumatol Arthrosc 25:222–228. https://doi.org/10.1007/s00167-016-4275-y
Cronström A, Tengman E, Häger CK (2023) Return to Sports: A Risky Business? A Systematic Review with Meta-Analysis of Risk Factors for Graft Rupture Following ACL Reconstruction. I Sports Med 53:91–110. https://doi.org/10.1007/s40279-022-01747-3
Zhao D, Pan JK, Lin FZ, Luo MH, Liang GH, Zeng LF, Huang HT, Han YH, Xu NJ, Yang WY, Liu J (2023) Risk Factors for Revision or Rerupture After Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-analysis. Am J Sports Med 51:3053–3075. https://doi.org/10.1177/03635465221119787
Hurley ET, Mojica ES, Kanakamedala AC, Meislin RJ, Strauss EJ, Campbell KA, Alaia MJ (2022) Quadriceps tendon has a lower re-rupture rate than hamstring tendon autograft for anterior cruciate ligament reconstruction - A meta-analysis. J isakos 7:87–93. https://doi.org/10.1016/j.jisako.2021.10.001
Järvelä S, Kiekara T, Suomalainen P, Järvelä T (2017) Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective randomized study with 10-year results. Am J Sports Med 45(11):2578–2585. https://doi.org/10.1177/0363546517712231
American Orthopaedic Society for Sports Medicine (2000) IKDC KNEE FORMS. https://www.sportsmed.org/uploads/main/files/general/IKDC/AOSSM_IKDC_English_US.pdf. Accessed 27 November 2023.
Järvelä T (2007) Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective, randomize clinical study. Knee Surg Sports Traumatol Arthrosc 15(5):500–507. https://doi.org/10.1007/s00167-006-0254-z
Rai SK, Yazdany J, Fortin PR, Aviña-Zubieta JA (2015) Approaches for estimating minimal clinically important differences in systemic lupus erythematosus. Arthritis Res Ther 17:143. https://doi.org/10.1186/s13075-015-0658-6
Balasingam S, Karikis I, Rostgård-Christensen L, Desai N, Ahldén M, Sernert N et al (2022) Anatomic Double-Bundle Anterior Cruciate Ligament Reconstruction Is Not Superior to Anatomic Single-Bundle Reconstruction at 10-Year Follow-up: A Randomized Clinical Trial. Am J Sports Med 50:3477–3486. https://doi.org/10.1177/03635465221128566
Mao Z, Wang J, Wang Y, Jiang D, Wang X, Wang H, Lin L, Liu Y, Zeng L, Yu J (2021) Double-bundle anterior cruciate ligament reconstruction technique has advantages in chondroprotection and knee laxity control compared with single-bundle technique: A long-term follow-up with a minimum of 12 years. Knee Surg Sports Traumatol Arthrosc 29:3105–3114. https://doi.org/10.1007/s00167-020-06350-5
Suomalainen P, Moisala AS, Paakkala A, Kannus P, Järvelä T (2011) Double-bundle versus single-bundle anterior cruciate ligament reconstruction: randomized clinical and magnetic resonance imaging study with 2-year follow-up. Am J Sports Med 39(8):1615–1622. https://doi.org/10.1177/0363546511405024
Suomalainen P, Järvelä T, Paakkala A, Kannus P, Järvinen M (2012) Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective randomized study with 5-year results. Am J Sports Med 40(7):1511–1518. https://doi.org/10.1177/0363546512448177
Suomalainen P, Kiekara T, Moisala AS, Paakkala A, Kannus P, Järvelä T (2014) Effect of tunnel placements on clinical and magnetic resonance imaging findings 2 years after anterior cruciate ligament reconstruction using the double-bundle technique. Open Access J Sports Med 5:197–203. https://doi.org/10.2147/oajsm.s62050
Suomalainen P, Moisala AS, Paakkala A, Kannus P, Järvelä T (2013) Comparison of tunnel placements and clinical results of single-bundle anterior cruciate ligament reconstruction before and after starting the use of double-bundle technique. Knee Surg Sports Traumatol Arthrosc 21(3):646–653. https://doi.org/10.1007/s00167-012-1981-y
Mohtadi NG, Chan DS (2019) A randomized clinical trial comparing patellar tendon, hamstring tendon, and double-bundle ACL reconstructions: Patient-reported and clinical outcomes at 5-year follow-up. J Bone Joint Surg Am 101:949–960. https://doi.org/10.2106/jbjs.18.01322
Xu Z, Ma L, Li R (2023) Anatomic Double-Bundle and Single-Bundle Reconstructions Yield Similar Outcomes Following Anterior Cruciate Ligament Rupture: A Systematic Review and Meta-Analysis. Arthroscopy. https://doi.org/10.1016/j.arthro.2023.05.017
Eliya Y, Qureshi AR, Kay J, Nagai K, Hoshino Y, de Sa D (2023) Anatomical double-bundle anterior cruciate ligament reconstruction moderately improved tegner scores over the long-term: a systematic review and meta-analysis of randomized controlled trials. Knee Surg Sports Traumatol Arthrosc 31:436–448. https://doi.org/10.1007/s00167-022-07046-8
Acknowledgements
Not applicable
Funding
Open access funding provided by Tampere University (including Tampere University Hospital). There is no funding source.
Author information
Authors and Affiliations
Contributions
Timo Järvelä and Heikki Mäenpää designed the study. Arttu Seppänen performed clinical assessments. Heini Huhtala carried out the statistical analyses. Arttu Seppänen, Piia Suomalainen and Tommi Kiekara wrote the manuscript. All authors provided critical feedback and helped shape the manuscript. All authors approved the final manuscript. Timo Järvelä supervised the project.
Corresponding author
Ethics declarations
Ethical appoval
Ethical approval was granted from the ethics committee of Tampere University Hospital.
Consent for publication
The research results are published at a general level. It is not possible to identify an individual from the results. The manuscript does not contain data of individuals in any form (including personal data, images or videos).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
NCT06001164, 08/18/2023, retrospectively registered
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Seppänen, A., Suomalainen, P., Kiekara, T. et al. Double-bundle anterior cruciate ligament reconstruction resulted in better International Knee Documentation Committee objective grading at fifteen year follow-up compared to single-bundle reconstruction. International Orthopaedics (SICOT) 48, 905–912 (2024). https://doi.org/10.1007/s00264-024-06106-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-024-06106-7