Abstract
Purpose
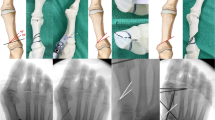
The effectiveness of minimally invasive surgery (MIS)-distal chevron metatarsal osteotomy (DCMO) for the correction of moderate-to-severe hallux valgus deformity is unclear. This study aimed to compare the radiographic and clinical outcomes of our novel MIS-proximal chevron metatarsal osteotomy (PCMO) with those of MIS-DCMO performed during the same timeframe.
Methods
We prospectively compared the outcomes of patients who underwent MIS-PCMO (n = 20 patients; 22 cases) with those of patients who underwent MIS-DCMO (n = 23 patients; 26 cases) for moderate-to-severe hallux valgus deformity (hallux valgus angle [HVA] ≥ 30° and first-to-second intermetatarsal angle [IMA] ≥ 13°) between June 2017 and January 2019. The minimum follow-up duration for study inclusion was two years. The HVA, IMA, distal metatarsal articular angle (DMAA), relative length of the second metatarsal, medial sesamoid position, and Meary’s angle to evaluate the degree of deformity correction and its maintenance were measured pre-operatively and at the final follow-up.
Results
Compared with MIS-DCMO, MIS-PCMO resulted in significantly greater correction of the HVA (P < 0.001) and IMA (P = 0.01), along with Meary’s angle improvement (P < 0.001); however, the DMAA worsened (P = 0 .01). Furthermore, a significantly greater change was found in the relative second metatarsal length in the MIS-DCMO group (P = 0.01). No significant between-group differences were noted in the correction of the medial sesamoid position (P = 0.445).
Conclusion
Compared with MIS-DCMO, MIS-PCMO can be a better option for correcting moderate-to-severe hallux valgus deformities. However, this technique should be applied carefully when the pre-operative DMAA is already large because the DMAA can become worse post-operatively.





Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this published article.
References
Choi JY, Yoon HH, Suh YM, Suh JS (2017) Surgical correction of hallux valgus complicated with adult-type pes plano-valgus. J Orthop Surg 25(1):1–6
Zhang Y, Awrejcewicz J, Szymanowska O et al (2018) Effects of severe hallux valgus on metatarsal stress and the metatarsophalangeal loading during balanced standing: a finite element analysis. Comput Biol Med 1(97):1–7
Nix S, Smith M, Vicenzino B (2010) Prevalence of hallux valgus in the general population: a systematic review and meta-analysis. J Foot Ankle Res 27(3):21
Coughlin MJ, Anderson RB (2014) Hallux valgus. In: Coughlin MJ, Saltzman CL, Anderson RB (eds) Mann’s surgery of the foot and ankle, 9th edn. Elsevier, Philadelphia, pp 155–321
Bia A, Guerra-Pinto F, Pereira BS, Corte-Real N, Olivia XM (2018) Percutaneous osteotomies in hallux valgus: a systematic review. J Foot Ankle Surg 57:123–130
Brogan K, Voller T, Gee C, Borbely T, Palmer S (2014) Third generation minimally invasive correction of hallux valgus: technique and early outcomes. Int Orthop 38(10):2115–2121
Lee M, Walsh J, Smith MM, Ling J, Wines A, Lam P (2017) Hallux valgus correction comparing percutaneous chevron/Akin (PECA) and open scarf/Akin osteotomies. Foot Ankle Int 38(8):838–846
Malagelada F, Sahirad C, Dalmau-Pastor M et al (2019) Minimally invasive surgery for hallux valgus: a systematic review of current surgical technique. Int Orthop 43:625–637
Lucas y Hernandez J, Golanó P, Roshan-Zamir S, Darcel V, Chauveaux D, Laffenêtre O (2016) Treatment of moderate hallux valgus by percutaneous, extra-articular reverse-L Chevron (PERC) osteotomy. Bone Joint J 98-B(3):365–373
Holme TJ, Sivaloganathan SS, Patel B, Kunasingam K (2020) Third-generation minimally invasive chevron Akin osteotomy for hallux valgus. Foot Ankle Int 41(1):50–56
Vernois J, Redfern D (2013) Percutaneous Chevron; the union of classic stable fixed approach and percutaneous technique. Fuss Sprunggelenk 11(2):70–75
Kaufmann G, Dammerer D, Heyenbrock F, Braito M, Moertlbauer L, Liebensteiner M (2019) Minimally invasive versus open chevron osteotomy for hallux valgus correction: a randomized controlled trial. Int Orthop 43:343–350
Lai MC, Rikhraj IS, Woo YL, Yeo W, Sean YC, Koo K (2018) Clinical and radiological outcomes comparing percutaneous chevron-Akin osteotomies vs open scarf-Akin osteotomies for hallux valgus. Foot Ankle Int 39(3):311–317
Singh MS, Khurana A, Kapoor D, Katekar S, Kumar A, Vishwakarma G (2020) Minimally invasive vs open distal metatarsal osteotomy for hallux valgus–a systematic review and meta-analysis. J Clin Orthop Trauma 11:348–356
Choi JY, Suh YM, Yeom JW, Suh JS (2017) Comparison of postoperative height changes of the second metatarsal among 3 osteotomy methods for hallux valgus deformity correction. Foot Ankle Int 38(1):20–26
Dalmau-Pastor M, Malagelada F, Cordier G, Del Vecchio JJ, Ghioldi ME, Vega J (2020) Anatomical study of minimally invasive lateral release techniques for hallux valgus treatment. Foot Ankle Int 41(8):984–992
Frigg A, Azugg S, Maquieira G, Pellegrino A (2019) Stiffness and range of motion after minimally invasive chevron-Akin and open scarf-Akin procedures. Foot Ankle Int 460(5):515–525
Hardy RH, Clapham JC (1951) Observations on hallux valgus; based on a controlled series. J Bone Joint Surg Br 33-B(3):376–391
Ibrahim T, Beiri A, Azzabi M, Best AJ, Taylor GJ, Menon DK (2007) Reliability and validity of the subjective component of the American Orthopaedic Foot and Ankle Society clinical rating scales. J Foot Ankle Surg 46(2):65–75
Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M (1994) Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int 15(7):349–353
Martin RL, Irrgang JJ, Burdett RG, Conti SF, Van Swearingen JM (2005) Evidence of validity for the foot and ankle ability measure. Foot Ankle Int 26(11):968–983
Lee KB, Cho NY, Park HW, Seon JK, Lee SH (2015) A comparison of proximal and distal chevron osteotomy, both with lateral soft-tissue release, for moderate to severe hallux valgus in patients undergoing simultaneous bilateral correction. Bone Joint J 97-B:202–207
Park CH, Jang JH, Lee SH, Lee WC (2013) A comparison of proximal and distal chevron osteotomy for the correction of moderate hallux valgus deformity. Bone Joint J 95-B:649–656
Ahn JY, Lee HS, Seo JH, Kim JY (2016) Second metatarsal transfer lesions due to first metatarsal shortening after distal chevron metatarsal osteotomy for hallux valgus. Foot Ankle Int 37(6):589–595
Campbell B, Miller MC, William L, Conti SF (2018) Pilot study of a 3-dimensional method for analysis of pronation of the first metatarsal of hallux valgus patients. Foot Ankle Int 39:1449–1456
Wagner E, Wagner P (2020) Metatarsal pronation in hallux valgus deformity: a review. J Am Acad Orthop Surg Glob Res Rev 4(6):e20.00091
Yamaguchi S, Sasho T, Endo J et al (2015) Shape of the lateral edge of the first metatarsal head changes depending on the rotation and inclination of the first metatarsal: a study using digitally reconstructed radiographs. J Orthop Sci 20:868–878
Shibuya N, Kyprios EM, Panchani PN, Martin LR, Thorud JC, Jupiter DC (2018) Factors associated with early loss of hallux valgus correction. J Foot Ankle Surg 57:236–240
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the appropriate institutional ethics review committee and performed according to the tenets of the Declaration of Helsinki.
Consent to participate
Written informed consent was obtained from all enrolled patients.
Consent for publication
The authors agree to publication. This manuscript has not been published in any journals.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Level of Evidence: Level III, prospective comparative series
Supplementary information
Below is the link to the electronic supplementary material.
Supplementary file1. (MP4 81.9 MB)
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Choi, J.Y., Kim, B.H. & Suh, J.S. A prospective study to compare the operative outcomes of minimally invasive proximal and distal chevron metatarsal osteotomy for moderate-to-severe hallux valgus deformity. International Orthopaedics (SICOT) 45, 2933–2943 (2021). https://doi.org/10.1007/s00264-021-05106-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-021-05106-1