Abstract
Purpose
Open surgery, nonsurgical positioning device and casting are mainstay treatments of developmental dysplasia of the hip (DDH). The optimal indicators for surgical interventions remain unclear. In this study, we aim to establish empirical, sensitive radiographic indicators for peri-acetabular osteotomy intervention in developmental dysplasia in Chinese children.
Methods
One hundred and three DDH patients treated in The Soochow University Children’s Hospital between 2006 and 2012 were assessed; patients with known causes of neuron muscular and abnormal hip joint origin were excluded. Fifty-four suitable patients, demonstrating 71 dysplasia hips with complete clinical record and adequate X-ray films, were enrolled in this study. Patients were divided into group A (conservative interventions failed, followed by salvage peri-acetabular osteotomy) and group B (conservative treatment only); a total of 16 quantitative parameters were measured on each pelvic X-ray film.
Results
Among 71 hip joints measured, 29 hips of group A underwent salvage peri-acetabular osteotomy (40.8 %,) showed higher X2, Y, h, and Smith c/b (Vh) (p < 0.05). The age, c, HT, b, A2 in the group A salvage operation were statistically significantly different compared to group B patients (without salvage operations) (p < 0.05).
Conclusions
Pre-operative pelvic X-ray film assessment of acetabulum lateralization markers (X2, c, HT, c/b ratio) and the superior migration measurements (Y, h, h/b ratio) are potentially valuable radiographic indicators for determining which DDH patients will require peri-acetabular osteotomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Developmental dysplasia of the hip (DDH) is the most common childhood hip disorder. The reported incidence of DDH ranges from 15 to 20 per 1,000 cases [1, 2]. It is characterized by a wide range, from mild forms of hip dysplasia to high dislocation of the femoral head. Hip instability during infancy usually resolves within the first few weeks after birth without treatment. The interaction between the acetabulum and femoral head is essential for natural development of the hip. Prolonged periods of dislocation of the acetabulum and femoral head and delayed restoration of their dynamic interaction will impair normal hip joint modeling and shaping. Conservative approaches and surgical procedures are widely used to restore the normal anatomical relationship of the acetabulum and femoral head [3–5]. Surgical procedures pioneered by Smith-Petersen in 1948 was later improved by several others [6], and have shown that surgical repositioning of the hip to its normal anatomical position is possible [8]. Acetabular or femoral osteotomies are commonly performed when the joint does not develop satisfactorily after initial nonsurgical reduction. The characteristic indicators of DDH which requires surgical intervention remain unclear; the extent to which age and timing of early procedures relate to prognostic factors has yet to be defined.
This study sought to identify measureable radiological indicators for predicting the subsequent requirement of acetabular dysplasia operations based on retrospective analysis. Previous papers have explored this issue in the treatment of DDH after initial open or closed reduction; however, this study is unique in addressing developmental dysplasia in Chinese children. Furthermore, we focused on measureable radiological markers to help clinicians in decision making and to improve the planning and performance of osteotomy procedures.
Materials and methods
Patient information and selection criteria
One hundred and three DDH patients treated in The Soochow University Children’s Hospital between March 2006 and February 2012 were assessed for inclusion in this study. Case selection criteria for this study were: (1) an age of 12–36 months; (2) the presence of complete clinical records and complete pre-operative and post-operative follow-up pelvic film; (3) a follow-up time of one year or over; (4) an absence of known causes for hip dislocation such as cerebral palsy, multiple joint contractures or muscle disorders. Fifty-four suitable patients were included, with a total of 71 hips enrolled in this study. Among them, ten cases were male, 44 cases were female; 19 cases enrolled only the left hip, 18 cases only the right hip and 17 cases enrolled both hips. The selected patients were then divided into two groups: group A—DDH patients failed by conservative treatment, followed by salvage pelvic osteotomy intervention; group B—DDH patients successfully treated by conservative treatments alone. The surgical procedures were standard pelvic osteotomy [7, 8] with routine anesthesia, in a supine position followed by standard post-operative care.
Pelvic film measurement and evaluation
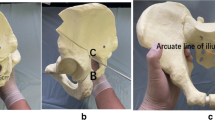
Standard anterior-posterior pelvic plain images were taken to include the whole iliac crest, hip joints and upper portion of femur bone. All X-ray film images were taken as recommended according to the departmental protocol.
Pelvic plain film measurement: before measurement, each film’s identity was blinded, one trained technician carried out the measurement based on a protocol agreed by a MDT (multidisciplinary team) composed of an orthopaedic surgeon, a radiologist and a diagnostic radiographer, with at least three repeated readings recorded on each parameter, the mean value of three measurements were used in the following analysis. A total of 16 different parameters were measured and two ratios were calculated (Fig. 1).
The 16 different parameters include: A—distance between both sides of the iliac innermost edge; A1—acetabular span; A2—acetabular depth; D2—the height of the femoral head ossification nucleus; h—distance between the uppermost proximal femoral metaphysis and line H; D1—the width of the femoral head ossification nucleus; HT—improved head teardrop distance; c—femur metaphysis proximal from the innermost and intermediate line; b—P line and the middle line distance; T—acetabular angle (degrees); X1—distance between nuclear ossification center of the femoral head and the middle line; X2—distance between nuclear ossification center of the femoral head and the line P; W—pelvis width; Y—distance between nuclear ossification center of the femoral head line H. Parameter measurements from pelvic X-ray film were as shown in Fig. 1.
Data evaluation and statistical analysis
After data quality is checked, the grouped data are proceeded to statistical analysis. SPSS 17.0 statistical software (SPSS, Chicago, IL, USA) was used for two-sample t-tests, set test α = 0.05, p values were determined; p < 0.05 was considered statistically significant.
Results and discussion
DDH is one of the most common paediatric orthopaedic diseases. DDH develops from impaired acetabular coverage of the femoral head, which leads to long-term biomechanical abnormalities, resulting in late subluxation or hip dislocation [9]. Both non-invasive approaches and surgical approaches are used in the clinic. Surgical management of developmental dysplasia remains the last solution for DDH patients if non-invasive approaches failed. Early invasive surgical operation at a young age (12 months) is traditionally recommended, to maximize the potential benefit of early recovery and normal development of hip joint function [10]. However, there are accumulating data to show that surgical intervention in older children, 18 months of age or over, remains beneficial [11], and some authors suggest that the developmental benefits may persist to even up to pre-school age [12, 13]. However, there is no consensus on the optimal timing for surgical intervention.
In this study, we analyzed 71 hips retrospectively, with median age of 20.5 months (from 12 to 36 months); the average follow-up time was 35 months (from 12 to 83 months). Fifty-four cases out of the 71 were lateral dislocations of the hip. Among 71 hips studied, 42 hips (group B, 59.2 %) recovered without surgical intervention; of the remaining 29 hips (group A, 40.8 %), most patients experienced a salvage operation due to the hip dislocation. A total of 16 parameters were measured; X-ray film measurement and data analysis were double blinded, and data were consolidated by the mean of three repeated measurements. The mean values of measurements in group A and group B, standard deviation, and p values are presented in Table 1. A series of parameters show significant differences between the two groups. These include: X2 (the distance between the centre of the femoral head ossification nucleus and line P), Y (the distance between the centre of the femoral head and nuclear ossification line H), h (the distance between the uppermost proximal femoral metaphysis and line H), Smith c p values/b (Vc) and Smith c/b (Vh) ratio, all of which are highly significantly greater in group A (DDH with surgery) (p < 0.05).
The other four parameters measured are also statistically significant in group A (DDH with surgery), including the proximal femoral metaphysis innermost and the middle line distance (c), modified head teardrop distance (HT), P line and the middle line distance (b), acetabular depth (A2), was considered statistically significant (p < 0.05). A representative follow up X-ray image of pre-operative and post-operative images presented in Fig. 2.
Although some studies support the role of early non-surgical treatment in reducing the incidence of salvage surgical operation. López-Carreño et al. [14] reported that all hips treated at or after the age of 18 months should undergo acetabuloplasty concurrent with open reduction . Others investigators believe the opposite, stating that early, routine, pelvic osteotomy to correct acetabular dysplasia may be unnecessary in many children [15].
Avisse et al. [16] reported that ossification of acetabular is observed as early as three months after birth. The ossification process facilitates hip joint cup formation under the pressure of the femoral head. Early diagnosis of DDH and re-establishment of the hip joint interface is important for shaping the acetabulum, allowing normal hip development and reducing the possibility of salvage surgery. However, Luhmann et al. [7] showed no significant decrease in the rate of secondary salvage surgery in the six month group and the 12-month group in a retrospective study of 153 hips, and even children given the delayed 12-month operation were not affected in terms of the incidence of the secondary salvage surgery. Our data indicate that the older the patient, the more likely to require pelvic osteotomy; this difference between younger and older children groups (12-month group and 36-month group) is significant (p = 0.025). Older children are more likely to need a surgical intervention, which is consistent with data from several other studies [2, 11]. However, due to the limitation imposed by the number of cases in our study, we are unable to compare the effect of different nonsurgical methods on the incidence of salvage osteotomy—which is under way in our further research.
This study sought, as Brougham et al. [17] recommended, to develop early radiological guideline markers for the requirement of subsequent acetabular operations surgery dysplasia, to enable early rather than late surgery to be performed to assist clinical decision making. Several studies have attempted to determine the predictors of outcome or prognosis factors, or evaluation of specific indicators for the need for pelvic osteotomy [5, 10, 17] . Our study, as other researchers have proposed [18, 19], to assess the value of imaging features of DDH after birth up to two to three years using pelvic plain film, in order to develop a simple, reliable indicator to predict radiological DDH and its association with the requirements of salvage osteotomy.
It is worth noting that the lateralization index (X2, HT, c, c/b ratio) and upward shift indicators (Y, h, h/b) are increased significantly in the operation group (Table 1). The sideways and superior shifting of the femoral head impacts the development of acetabular cup, affecting its depth and shape. The acetabulum needs the femoral head to develop normally [5]. Our study is unique in addressing the multiple issues involved. We focused on better defining acetabular insufficiency in order to improve the planning and performance of surgical procedures to enable early rather than late surgery to be performed, while avoiding unnecessary acetabular operations.
In this study, we selected the X-ray imaging approach, because X-ray film and imaging are widely accessible in local or central regional hospitals in China. Most X-ray imaging facilities have strong post-image processing capacity, allowing relatively wide imaging conditions; various X-ray image processing techniques also have no direct effect on the final read-out of image; standardized measurement making it a practical, reliable and cost-effective choice. Although ultrasound has been widely used for newborns and infants, but there are obvious differences in the results between the two modalities [20, 21]. Other more advanced modalities such as computer tomography (CT) uses higher doses of X-rays, which are unsuitable for children and magnetic resonance imaging (MRI) is prohibitively costly, making both CT and MRI unsuitable for general screening of DHH children and follow-up imaging.
In conclusion, the femoral head lateralization shift indicators (X2, c, HT, c/b ratio) and femoral head upward shift indicators (Y, h, h/b ratio) show predictive values for infant DDH which require pelvic osteotomy operation; they are potentially valuable indicators for clinician decision-making regarding early surgical operation in infant DDH.
References
Bolland BJ, Wahed A, Al-Hallao S, Culliford DJ, Clarke NM (2010) Late reduction in congenital dislocation of the hip and the need for secondary surgery: radiologic predictors and confounding variables. J Pediatr Orthop 30(7):676–682. doi:10.1097/BPO.0b013e3181efb8c7
Sankar WN, Tang EY, Moseley CF (2009) Predictors of the need for femoral shortening osteotomy during open treatment of developmental dislocation of the hip. J Pediatr Orthop 29(8):868–871. doi:10.1097/BPO.0b013e3181c29cb2
Cherney DL, Westin GW (1989) Acetabular development in the Infant’s dislocated hips. Clin Orthop 242:98
Shefelbine SJ, Carter DR (2004) Mechanobiological predictions of growth front morphology in developmental hip dysplasia. J Orthop Res 22:346–352. doi:10.1016/j.orthres.2003.08.004
Sankar WN, Young CR, Lin AG, Crow SA, Baldwin KD, Moseley CF (2011) Risk factors for failure after open reduction for DDH:a matched cohort analysis. J Pediatr Orthop 31:232–239. doi:10.1097/BPO.0b013e31820c9b31
Troelsen A (2009) Surgical advances in periacetabular osteotomy for treatment of hip dysplasia in adults. Acta Orthop Suppl 80(332):1–33
Luhmann SJ, Bassett GS, Gordon JE, Schootman M, Schoenecker PL (2003) Reduction of a dislocation of the hip due to developmental dysplasia implications for the need for future surgery. J Bone Joint Surg Am 85-A:239–243
Tibrewal S, Gulati V, Ramachandran M (2013) The pavlik method: a systematic review of current concepts. J Pediatr Orthop B 22(6):516–20. doi:10.1097/BPB.0b013e328365760e
Weinstein SL (1987) Natural history of congenital hip dislocation (CDH) and hip dysplasia. Clin Orthop Relat Res 225:62–76
Honda M, Arita S, Mitani S, Takeda Y, Ozaki T, Inamura K, Kanazawa S (2010) Infant hip joint diagnostic support system based on clinical manifestations in X-ray images. Acta Med Okayama 64(3):189–196
Albinana J, Dolan LA, Spratt KF, Morcuende J, Meyer MD, Weinstein SL (2004) Acetabular dysplasia after treatment for developmental dysplasia of the hip. Implications for secondary procedures. J Bone Joint Surg (Br) 86(6):876–886. doi:10.1302/0301-620X.86B6.14441
Weiner DS, Hoyt WA Jr, O’dell HW (1977) Congenital dislocation of the hip the relationship of premanipulation traction and age to avascular necrosis of the femoral head. J Bone Joint Surg Am 59:306–311
Malvitz TA, Weinstein SL (1994) Closed reduction for congenital dysplasia of the hip functional and radiographic results after an average of thirty years. J Bone Joint Surg Am 76:1777–1792
López-Carreño E, Carillo H, Gutiérrez M (2008) Dega versus salter osteotomy for the treatment of developmental dysplasia of the hip. J Pediatr Orthop B 17(5):213–21. doi:10.1097/BPB.0b013e32830850eb
Olney B, Latz K, Asher M (1998) Treatment of hip dysplasia in older children with a combined one-stage procedure. Clin Orthop Relat Res 347:215–223
Avisse C, Gomes H, Delvinquiere V (1997) Anatomic study of the pre- and neonatal hip.Physiopathologic considerations on dyspalasia and congenital dislocation of the hip. Surg Radiol Anat 19:155–159
Brougham DI, Broughton NS, Cole WG, Menelaus MB (1988) The predictability of acetabular development after closed reduction for congenital dislocation of the hip. J Bone Joint Surg (Br) 70(5):733–736
Mitani S, Odak TG (1993) Prediction for prognosis from radiologic measurements of patients treated with Pavlik harness for congenital dislocation of the hip. J Pediatr Orthop 13(3):303–310
Broughton NS, Brougham DI, Cole WG, Menelaus MB (1989) Reliability of radiological measurements in the assessment of the child’s hip. J Bone Joint Surg (Br) 71(1):6–8
Arti H, Mehdinasab SA, Arti S (2013) Comparing results of clinical versus ultrasonographic examination in developmental dysplasia of hip. J Res Med Sci 18(12):1051–1055
Atweh LA, Kan JH (2013) Multimodality imaging of developmental dysplasia of the hip. Pediatr Radiol 43(Suppl 1):S166–S171. doi:10.1007/s00247-012-2591-z
Acknowledgments
The study was financially supported by Jiangsu Province Natural Science Foundation (BK20131156), Suzhou research project funding SYS201437 and SYS201351,Open Funding of Key laboratory of stem cells and biomedical materials of Jiangsu Province.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
None.
Additional information
Yunfang Zhen and Chunhua Yin contributed equally to this work.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Zhen, Y., Yin, C., Tan, S. et al. Retrospective analysis of the radiographic indicators for peri-acetabular osteotomy of developmental dysplasia in children. International Orthopaedics (SICOT) 40, 341–345 (2016). https://doi.org/10.1007/s00264-015-3038-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-3038-6