Abstract
Purpose
Following lumbar spine surgery, postoperative complications can appear, including epidural adhesions. The formation of fibrosis around the dura mater can, on the one hand, lead to compression of the nerve roots with recurrent radicular pain and, on the other hand, can increase the risks of specific complications at spinal re-intervention (haematomas and dural breaches). The aim of this prospective monocentric study was to assess the safety of a new collagen antiadhesion membrane in vertebral osteotomy surgery where scar tissue and adhesions are important.
Methods
Twenty-six patients consecutively operated for lumbar posterior subtraction osteotomy with implantation of a collagen-based anti-adhesion membrane were evaluated. Membrane tolerance was evaluated at the short and midterm during the regular follow-up.
Results
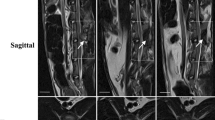
At six months’ follow-up, postoperative pain [visual analogue scale (VAS)] and disability (Oswestry Disability Index score) were significantly reduced 33.1 and 43.1 %, respectively. These results were confirmed at 12-months’ follow-up, with a decrease in pain of 39.9 % and in disability of 49.3 %. Amongst the observed postoperative complications was neither spinal fluid leak nor durotomy. Presence of the membrane was not related to complications. Two patients required further surgery for infection and nonunion at the osteotomised level. Adhesions to the dura mater were limited and thin, facilitating exposure.
Conclusions
This study shows good tolerance of the collagen based membrane for spinal osteotomy and its satisfactory use for preventing postoperative epidural adhesions. Good surgical practice associated with an anti-adhesion barrier may decrease fibrosis formation and improve postoperative functional results.



Similar content being viewed by others
References
Le Huec JC, Roussouly P (2011) Sagittal spino-pelvic balance is a crucial analysis for normal and degenerative spine. Eur Spine J 20(Suppl 5):556–557
Enercan M, Ozturk C, Kahraman S, Sarıer M, Hamzaoglu A, Alanay A (2013) Osteotomies/spinal column resections in adult deformity. Eur Spine J 22(Suppl 2):S254–S264
Ross JS, Robertson JT, Frederickson RC, Petrie JL, Obuchowski N, Modic MT, deTribolet N et al (1996) Association between peridural scar and recurrent radicular pain after lumbar discectomy: magnetic resonance evaluation. ADCON-L European Study Group. Neurosurgery 38:855–861
Ido K, Urushidani H (2001) Fibrous adhesive entrapment of lumbosacral nerve roots as a cause of sciatica. Spinal Cord 39:267–273
Cooper RG, Freemont AJ, Hoyland JA, Jenkins JP, West CG, Illingworth KJ, Jayson MI (1995) Herniated vertebral disc-associated periradicular fibrosis and vascular abnormalities occur without inflammatory cell infiltration. Spine 20:591–598
Gerometta A, Rodriguez Olaverri JC, Bittan F (2012) Infection and revision strategies in total disc arthroplasty. Int Orthop 36:471–474
Jayson MI (1989) Vascular damage, fibrosis, and chronic inflammation in mechanical back problems Semin. Arthritis Rheum 18:73–76
Rydevik B, Brown MD, Lundborg G (1984) Pathoanatomy and pathophysiology of nerve root compression. Spine 9:7–15
Rydevik B, Myers RR, Powell HC (1989) Pressure increases in the dorsal root ganglion after mechanical compression. Spine 14:574–576
Malter AD, McNeney B, Loeser J, Deyo RA (1998) 5-year reoperation rates after different types of lumbar spine surgery. Spine (Phila Pa 1976) 23:814–820
Abitbol JJ, Lincoln TL, Bl L, Amiel D, Akeson WH, Garfin SR (1994) Preventing postlaminectomy adhesion: a new experimental model. Spine 19:1809–1814
Hinton JL, Warejcka DJ, Mei Y, McLendon RE, Laurencin C, Lucas PA, Robinson JS Jr (1995) Inhibition of epidural scar formation after lumbar laminectomy in the rat. Spine 20:564–570
Songer MN, Rauschning W, Carson EW, Pandit SM (1995) Analysis of peridural scar formation and its prevention after lumbar laminotomy and discectomy in dogs. Spine 20:571–580
Jacobs R, McClain O, Neff J (1980) Control of postlaminectomy scar formation: an experimental and clinical study. Spine 5:223–229
Zou X, Li H, Egund N, Lind M, Bünger C (2004) Inhibition of spinal fusion by use of a tissue ingrowth inhibitor. Eur Spine J 13:157–163
Kitano T, Zerwekh JE, Edwards ML, Usui Y, Allen MD (1991) Viscous carboxymethylcellulose in the prevention of epidural scar formation. Spine 16:820–823
Langenskjöld A, Kiviluoto O (1976) Prevention of epidural scar formation after operations on the lumbar spine by means of free fat transplants. Clin Orthop Relat 115:92–95
Gill GG, Scheck M, Kelley ET, Rodrigo JJ (1985) Pedicle fat grafts for the prevention of scar in low-back surgery: a preliminary report on the first 92 cases. Spine 10:662–677
Yong-Hing K, Reilly J, de Korompay V, Kirkaldy-Willis WH (1980) Prevention of nerve root adhesions after laminectomy. Spine 5:59–64
MacKay MA, Fischgrund JS, Herkowitz HN, Kurz LT, Hecht B, Schwartz M (1995) The effect of interposition membrane on the outcome of lumbar laminectomy and discectomy. Spine 20:1793–1796
Jensen TT, Asmussen K, Berg-Hansen EM, Lauritsen B, Manniche C, Vinterberg H, Jensen L, Kramhøft J (1996) First-time operation for lumbar disc herniation with or without free fat transplantation. Prospective triple-blind randomized study with reference to clinical factors and enhanced computed tomographic scan 1 year after operation. Spine 21:1072–1076
Bernsmann K, Krämer J, Ziozios I, Wehmeier J, Wiese M (2001) Lumbar micro disc surgery with and without autologus fat graft : a prospective randomized trial evaluated with reference to clinical and social factors. Arch Orthop Trauma Surg 121:476–480
Manchikanti L, Saini B, Singh V (2001) Spinal endoscopy and lysis of epidural adhesions in the management of chronic low back pain. Pain Physician 4:240–265
Gillard DM, Corenman DS, Dornan GJ (2014) Failed less invasive lumbar spine surgery as a predictor of subsequent fusion outcomes. Int Orthop 38:811–815
Howe JF, Loeser JD, Calvin WH (1977) Mechanosensitivity of dorsal root ganglion and chronically injured axons. A physiological basis for the radicular pain of nerve root compression. Pain 3:25–41
Arrotegi I (2011) Reduction of clinical symptoms after lumbar discectomy using Collagen Dural Matrix clinical trial. World Spinal Column J 2(1):7–11
Gill GG, Sakovich L, Thompson E (1979) Pedicle fat grafts for the prevention of scar formation after laminectomy. An experimental study in dogs. Spine 4:176–186
Cheng J, Wang H, Zheng W, Li C, Wang J, Zhang Z, Huang B, Zhou Y (2013) Reoperation after lumbar disc surgery in two hundred and seven patients. Int Orthop 37:1511–1517
Dangelmajer S, Zadnik P, Rodriguez S, Gokaslan ZL, Sciubba DM (2014) Minimally invasive spine surgery for adult degenerative lumbar scoliosis. Neurosurg Focus 36(5):E7
Smith JS, Shaffrey CI, Sansur CA et al (2011) Rates of infection after spine surgery based on 108,419 procedures: a report from the Scoliosis Research Society Morbidity and Mortality Committee. Spine 36:556–563
Mummaneni PV, Dhall SS, Ondra SL, Mummaneni VP, Berven S (2008) Pedicle subtraction osteotomy. Neurosurgery 63:171–176
Fairbank J, Couper J, Davies J, O’Brien JP (1980) The Oswestry low back pain questionnaire. Physiotherapy 66:271–273
Copay AG, Glassman SD, Subach BR, Berven S, Schuler TC, Carreon LY (2008) Minimum clinically important difference in lumbar spine surgery patients: a choice of methods using the Oswestry Disability Index, Medical Outcomes Study questionnaire Short Form 36, and pain scales. Spine J 8:968–974
Shih HN, Fang JF, Chen JH, Yang CL, Chen YH, Sung TH, Shih LY (2004) Reduction in experimental peridural adhesion with the use of a crosslinked hyaluronate/ collagen membrane. J Biomed Mater Res B Appl Biomater 71B:421–428
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
LeHuec, JC., Sadikki, R., Cogniet, A. et al. Role of a collagen membrane in adhesion prevention strategy for complex spinal surgeries. International Orthopaedics (SICOT) 39, 1383–1390 (2015). https://doi.org/10.1007/s00264-015-2767-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-2767-x