Abstract
Background
Sequential tyrosine kinase inhibitors (TKIs) following immune checkpoint inhibitors (ICIs) increases the incidence of serious adverse events (SAEs). However, the factors and the types of TKIs that affect the incidence of SAEs remain unknown.
Methods
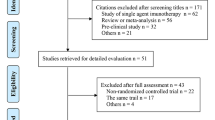
We retrospectively reviewed advanced non-small cell lung cancer (NSCLC) patients who received sequential TKIs following ICIs between November 2015 and April 2021. All AEs were evaluated using Common Terminology Criteria for Adverse Events (CTCAE) ver 5.0.
Results
Among 1,638 NSCLC patients who received ICIs, 63 patients received sequential TKIs following ICIs. The types of TKIs included EGFR-TKIs in 48 patients, ALK-TKIs in 10 patients, and others in 5 patients. The median dosing interval was 57 days (range: 7–698). Eighteen (28.6%) patients developed SAEs (Grade 3/4 or hospitalized). The incidence of SAEs and withdrawal of TKIs due to AEs were significantly higher in patients (n = 40) who initiated TKI treatment within 3 months after ICIs than in patients (n = 23) who initiated TKI treatment 3 months after ICIs (SAEs, 40.0% vs. 4.3%, p < 0.01; withdrawal rate: 57.5% vs. 21.7%, p < 0.01). There was no significant difference in the incidence of SAEs and withdrawal rate due to AEs between EGFR-TKIs and other TKIs (SAE, 22.9% vs. 40.0%, p = 0.20; withdrawal rate: 41.7% vs. 53.3%, p = 0.55).
Conclusion
The dosing interval from last ICI to the initiation of TKI treatment can affects the incidence of SAEs and the withdrawal rate due to AEs regardless of the types of TKIs.




Similar content being viewed by others
Data availability
Data are available on reasonable request.
Abbreviations
- ABCP:
-
Atezolizumab, bevacizumab, carboplatin, and paclitaxel
- ALK:
-
Anaplastic lymphoma kinase
- CTCAE:
-
Common Terminology Criteria for Adverse Events
- Dab/Tra:
-
Dabrafenib/trametinib
- ECOG:
-
Eastern Cooperative Oncology Group
- EGFR:
-
Epidermal growth factor receptor
- HER2:
-
Human epidermal growth factor receptor 2
- ICI:
-
Immune checkpoint inhibitor
- ILD:
-
Interstitial lung disease
- MAPK:
-
Mitogen-activated protein kinase
- MET:
-
C-Met
- NE:
-
Not estimable
- NRG1:
-
Neuregulin 1
- NSCLC:
-
Non-small cell lung cancer
- PD-1:
-
Programmed cell death 1
- PD-L1:
-
Programmed death-ligand 1
- PS:
-
Performance status
- ROS1:
-
C-ros oncogene 1
- SAE:
-
Serious adverse event
- TKI:
-
Tyrosine kinase inhibitor
References
Maemondo M, Inoue A, Kobayashi K et al (2010) Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N Engl J Med 362:2380–2388. https://doi.org/10.1056/NEJMoa0909530
Zhou C, Wu Y-L, Chen G et al (2011) Erlotinib versus chemotherapy as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (OPTIMAL, CTONG-0802): a multicentre, open-label, randomised, phase 3 study. Lancet Oncol 12:735–742. https://doi.org/10.1016/s1470-2045(11)70184-x
Sequist LV, Yang JC-H, Yamamoto N et al (2013) Phase III study of Afatinib or Cisplatin Plus pemetrexed in patients with metastatic lung adenocarcinoma With EGFR mutations. J Clin Oncol 31:3327–3334. https://doi.org/10.1200/jco.2012.44.2806
Solomon BJ, Mok T, Kim DW et al (2014) First-line crizotinib versus chemotherapy in ALK-positive lung cancer. N Engl J Med 371:2167–2177. https://doi.org/10.1056/NEJMoa1408440
Socinski MA, Jotte RM, Cappuzzo F et al (2018) Atezolizumab for first-line treatment of metastatic nonsquamous NSCLC. N Engl J Med 378:2288–2301. https://doi.org/10.1056/NEJMoa1716948
Kaira K, Naito T, Takahashi T et al (2010) Pooled analysis of the reports of erlotinib after failure of gefitinib for non-small cell lung cancer. Lung Cancer 68:99–104. https://doi.org/10.1016/j.lungcan.2009.05.006
Asahina H, Oizumi S, Inoue A et al (2010) Phase II study of gefitinib readministration in patients with advanced non-small cell lung cancer and previous response to gefitinib. Oncology 79:423–429. https://doi.org/10.1159/000326488
Cappuzzo F, Morabito A, Normanno N et al (2016) Efficacy and safety of rechallenge treatment with gefitinib in patients with advanced non-small cell lung cancer. Lung Cancer 99:31–37. https://doi.org/10.1016/j.lungcan.2016.06.008
Oda N, Ichihara E, Hotta K et al (2017) Phase II study of the EGFR-TKI rechallenge With Afatinib in patients with advanced NSCLC harboring sensitive EGFR mutation without T790M: Okayama lung cancer study group trial OLCSG 1403. Clin Lung Cancer 18:241–244. https://doi.org/10.1016/j.cllc.2016.07.003
Yamaguchi O, Kaira K, Mouri A et al (2019) Re-challenge of afatinib after 1st generation EGFR-TKI failure in patients with previously treated non-small cell lung cancer harboring EGFR mutation. Cancer Chemother Pharmacol 83:817–825. https://doi.org/10.1007/s00280-019-03790-w
Antonia SJ, Villegas A, Daniel D et al (2018) Overall survival with durvalumab after chemoradiotherapy in stage III NSCLC. N Engl J Med 379:2342–2350. https://doi.org/10.1056/NEJMoa1809697
Ahn MJ, Yang J, Yu H et al (2016) 136O: Osimertinib combined with durvalumab in EGFR-mutant non-small cell lung cancer: results from the TATTON phase Ib trial. J Thorac Oncol. https://doi.org/10.1016/s1556-0864(16)30246-5
Gettinger S, Hellmann MD, Chow LQM et al (2018) Nivolumab plus Erlotinib in patients with EGFR-mutant advanced NSCLC. J Thorac Oncol 13:1363–1372. https://doi.org/10.1016/j.jtho.2018.05.015
Schoenfeld AJ, Arbour KC, Rizvi H et al (2019) Severe immune-related adverse events are common with sequential PD-(L)1 blockade and osimertinib. Ann Oncol 30:839–844. https://doi.org/10.1093/annonc/mdz077
Lin JJ, Chin E, Yeap BY et al (2019) Increased hepatotoxicity associated with sequential immune checkpoint inhibitor and crizotinib therapy in patients with non-small cell lung cancer. J Thorac Oncol 14:135–140. https://doi.org/10.1016/j.jtho.2018.09.001
McCoach CE, Rolfo C, Drilon A et al (2022) hypersensitivity reactions to selpercatinib treatment with or without prior immune checkpoint inhibitor therapy in patients with non-small-cell lung cancer in LIBRETTO-001. J Thorac Oncol. https://doi.org/10.1016/j.jtho.2022.02.004
Kanda Y (2013) Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant 48:452–458. https://doi.org/10.1038/bmt.2012.244
Harding JJ, Pulitzer M, Chapman PB (2012) Vemurafenib sensitivity skin reaction after ipilimumab. N Engl J Med 366:866–868. https://doi.org/10.1056/NEJMc1114329
Imafuku K, Yoshino K, Ymaguchi K, Tsuboi S, Ohara K, Hata H (2017) Nivolumab therapy before vemurafenib administration induces a severe skin rash. J Eur Acad Dermatol Venereol 31:e169–e171. https://doi.org/10.1111/jdv.13892
Dimitriou F, Matter AV, Mangana J, Urosevic-Maiwald M, Micaletto S, Braun RP, French LE, Dummer R (2019) Cytokine release syndrome during sequential treatment with immune checkpoint inhibitors and kinase inhibitors for metastatic melanoma. J Immunother 42:29–32. https://doi.org/10.1097/CJI.0000000000000236
Gemma A, Kusumoto M, Sakai F et al (2020) Real-world evaluation of factors for interstitial lung disease incidence and radiologic characteristics in patients with EGFR T790M-positive NSCLC treated with osimertinib in Japan. J Thorac Oncol 15:1893–1906. https://doi.org/10.1016/j.jtho.2020.08.025
Brahmer JR, Drake CG, Wollner I et al (2010) Phase I study of single-agent anti-programmed death-1 (MDX-1106) in refractory solid tumors: safety, clinical activity, pharmacodynamics, and immunologic correlates. J Clin Oncol 28:3167–3175. https://doi.org/10.1200/JCO.2009.26.7609
Janne PA, Yang JC, Kim DW et al (2015) AZD9291 in EGFR inhibitor-resistant non-small-cell lung cancer. N Engl J Med 372:1689–1699. https://doi.org/10.1056/NEJMoa1411817
Mamesaya N, Kenmotsu H, Katsumata M, Nakajima T, Endo M, Takahashi T (2017) Osimertinib-induced interstitial lung disease after treatment with anti-PD1 antibody. Invest New Drugs 35:105–107. https://doi.org/10.1007/s10637-016-0389-9
Zhai X, Zhang J, Tian Y, Li J, Jing W, Guo H, Zhu H (2020) The mechanism and risk factors for immune checkpoint inhibitor pneumonitis in non-small cell lung cancer patients. Cancer Biol Med 17:599–611. https://doi.org/10.20892/j.issn.2095-3941.2020.0102
Sullivan RJ, Weber JS (2021) Immune-related toxicities of checkpoint inhibitors: mechanisms and mitigation strategies. Nat Rev Drug Discov. https://doi.org/10.1038/s41573-021-00259-5
Lizotte PH, Hong RL, Luster TA et al (2018) A high-throughput immune-oncology screen identifies EGFR inhibitors as potent enhancers of antigen-specific cytotoxic T-lymphocyte tumor cell killing. Cancer Immunol Res 6:1511–1523. https://doi.org/10.1158/2326-6066.CIR-18-0193
Pollack BP, Sapkota B, Cartee TV (2011) Epidermal growth factor receptor inhibition augments the expression of MHC class I and II genes. Clin Cancer Res 17:4400–4413. https://doi.org/10.1158/1078-0432.CCR-10-3283
Frederick DT, Piris A, Cogdill AP et al (2013) BRAF inhibition is associated with enhanced melanoma antigen expression and a more favorable tumor microenvironment in patients with metastatic melanoma. Clin Cancer Res 19:1225–1231. https://doi.org/10.1158/1078-0432.CCR-12-1630
Funding
The study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
YS and TY designed the study. YS collected the clinical data. YS performed statistical data analyses, interpretation of the results, and writing of the manuscript. YS and TY drafted the manuscript. All authors read the manuscript and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Yoshida received grants and personal fees from AstraZeneca and Bristol-Myers Squibb; grants from AbbVie, MSD, Ono Pharmaceutical, and Takeda Pharmaceutical; and personal fees from Chugai and Novartis. Dr. Matsumoto received grants from Grant-in-Aid for Scientific Research on Innovative Areas, Hitachi High-Technologies, Hitachi, Ltd., and National Cancer Center Research and Development Fund and received personal fees from AMCO INC., AstraZeneca, COOK, and Olympus. Dr. Masuda received personal fees from Chugai and AstraZeneca. Dr. Shinno received personal fees from Pfizer, AstraZeneca, and Chugai Pharmaceutical and received grants from Japan Clinical Research Operations K.K., Janssen Pharmaceutical K.K., and Ono Pharmaceutical. Dr. Okuma received grants from AbbVie. Dr. Goto received grants and personal fees from Bristol-Myers Squibb, Daiichi- Sankyo, Eli Lilly, Guardant Health, MSD, Novartis, Ono Pharmaceutical, Pfizer, and Taiho Pharmaceutical; grants from Kyorin; and personal fees from AstraZeneca, Boehringer Ingelheim, Chugai, and Illumina. Dr. Horinouchi received grants and personal fees from AstraZeneca, BMS, Chugai, Eli Lilly, MSD, Taiho Pharmaceutical, and Ono Pharmaceutical and received grants from Astellas, Genomic Health, and Merck Serono. Dr. Yamamoto received grants and personal fees from BMS, Boehringer Ingelheim, Chugai, Eisai, Eli Lilly, Ono Pharmaceutical, Pfizer, and Takeda Pharmaceutical; grants from Astellas, Bayer, Chiome Bioscience Inc., Daiichi-Sankyo, GSK, Janssen Pharma, Kyowa-Hakko kirin, MSD, Merck, Novartis, Otsuka, Taiho Pharmaceutical, Quintiles, and Sumitomo Dainippon; and received personal fees from AstraZeneca, Otsuka, Cimic, and Sysmex. Dr. Ohe received grants and personal fees from AstraZeneca, Bristol-Myers Squibb, Chugai, Eli Lilly, Janssen Pharma, Kyorin, MSD, Nippon Kayaku, Novartis, Ono Pharmaceutical, Pfizer, Taiho Pharmaceutical, and Takeda Pharmaceutical; grants from Kissei; and personal fees from Boehringer Ingelheim, and Celtrion. The remaining authors declare no competing interests.
Ethical approval
The present study with human samples has been approved by the Ethics Committee of the National Cancer Center Hospital, Tokyo, Japan (2019-123).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shimoda, Y., Yoshida, T., Miyakoshi, J. et al. Incidence of serious adverse events caused by tyrosine kinase inhibitor treatment following immune checkpoint inhibitor therapy in advanced NSCLC patients with oncogenic driver alterations. Cancer Immunol Immunother 72, 2613–2621 (2023). https://doi.org/10.1007/s00262-023-03429-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-023-03429-z