Abstract
Background
Microsatellite instability (MSI) is detected in approximately 15% of colorectal carcinoma (CRC) patients, which has emerged as a predictor of patient response to adjuvant chemotherapy. Rectal carcinoma (RC) is the most common type of CRC. Therefore, prediction of MSI status of RC is significant for personalized medication. The purpose of this article was to develop an integrative model that combines clinical characteristics and computed tomography-based (CT-based) tumoral/peritumoral radiomics to predict the MSI status in RC.
Methods
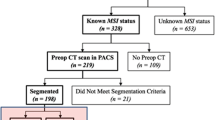
A cohort of 788 RCs with 97 high-MSI status (MSI-H) and 691 microsatellite stable status (MSS) were enrolled between January 2015 and January 2021 in this retrospective study. Clinical characteristics were recorded, and CT-based tumoral/peritumoral radiomic features were calculated after segmenting volume of interests. The patients were randomly divided into training and validation sets in a 7:3 proportion. Logistic models of single tumoral radiomics (LM-tRadio), peritumoral radiomics (LM-ptRadio), and combined tumoral/peritumoral radiomics (LM-Radio) were constructed to distinguish MSI-H from MSS, and a relevant radiomic score was calculated. An integrative nomogram (LM-Nomo) was developed, including significant clinical characteristics and CT-based tumoral/peritumoral radiomics. The area under receiver operator curve (AUC) was calculated to evaluate the efficacy of prediction.
Results
The AUCs of LM-Radio were 0.785 (95%CI 0.732–0.837) in the training set and were 0.628 (95%CI 0.528–0.723) in the validation set, which were higher than those of LM-tRadio and LM-ptRadio. The AUCs of single LM-ptRadio were slightly higher than those of LM-tRadio (0.724 vs. 0.708 in the training set, 0.613 vs. 0.602 in the validation set). The LM-Nomo containing carcinoembryonic antigen (CEA), hypertension, and CT-based tumoral/peritumoral radiomic score showed the highest AUCs of 0.796 (95%CI 0.748–0.843) in the training set and 0.679 (95%CI 0.588–0.771) in the validation set in predicting the MSI-H status of RC.
Conclusion
The AUCs of LM-ptRadio were slightly higher than LM-tRadio to evaluate the MSI-H status of RC. The LM-Nomo, which includes significant clinical characteristics and CT-based tumoral/peritumoral radiomics score, demonstrated the best performance in predicting MSI-H status of RC.





Similar content being viewed by others
References
Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018 Nov;68(6):394-424.
Siegel RL, Miller KD, Goding Sauer A, et al. Colorectal cancer statistics, 2020. CA Cancer J Clin. 2020;70(3):145-164.
Bagante F, Ruzzenente A, Sasaki K, et al. Morphologic and biologic characteristics of disease are associated with prognosis of patients with colo-rectal liver metastasis undergoing neoadjuvant chemotherapy. Hpb. 2018;20:189-190.
Tang YZ, Alabousi A. Incidental findings on staging CT for rectal cancer: Frequency, clinical significance and outcomes. Clin Imaging. 2023;93:14-22.
Wang Q, Xu J, Wang A, et al. Systematic review of machine learning-based radiomics approach for predicting microsatellite instability status in colorectal cancer. La Radiologia medica. 2023;128(2):136-148.
Trojan J, Stintzing S, Haase O, et al. Complete pathological response after neoadjuvant short-course immunotherapy with ipilimumab and nivolumab in locally advanced MSI-H/dMMR rectal cancer. Oncologist. 2021.
Boland CR, Goel A. Microsatellite instability in colorectal cancer. Gastroenterology. 2010;138(6):2073-2087.
Fan S, Li X, Cui X, et al. Computed Tomography-Based Radiomic Features Could Potentially Predict Microsatellite Instability Status in Stage II Colorectal Cancer: A Preliminary Study. Acad Radiol. 2019;26(12):1633-1640.
Kloor M, Staffa L, Ahadova A, von Knebel Doeberitz M. Clinical significance of microsatellite instability in colorectal cancer. Langenbeck's Archives of Surgery. 2014;399(1):23-31.
Mayerhoefer ME, Materka A, Langs G, et al. Introduction to Radiomics. J Nucl Med. 2020;61(4):488-495.
Pei Q, Yi X, Chen C, et al. Pre-treatment CT-based radiomics nomogram for predicting microsatellite instability status in colorectal cancer. Eur Radiol. 2022 Jan;32(1):714-724.
Zhang W, Yin H, Huang Z, et al. Development and validation of MRI-based deep learning models for prediction of microsatellite instability in rectal cancer. Cancer Med. 2021;10(12):4164-4173.
Li Z, Dai H, Liu Y, Pan F, Zhang M. Radiomics Analysis of Multi-Sequence MR Images For Predicting Microsatellite Instability Status Preoperatively in Rectal Cancer. Frontiers in Oncology. 2021;7(11):697497.
Zhang W, Huang Z, Zhao J, He D, Song B. Development and validation of magnetic resonance imaging- based radiomics models for preoperative prediction of microsatellite instability in rectal cancer. Annals of Translational Medicine. 2021;9(2):134-146.
Huang Z, Zhang W, He D, et al. Development and validation of a radiomics model based on T2WI images for preoperative prediction of microsatellite instability status in rectal cancer: Study Protocol Clinical Trial (SPIRIT Compliant). Medicine (Baltimore). 2020;99(10):e19428.
Li Z, Zhang J, Zhong Q, et al. Development and external validation of a multiparametric MRI-based radiomics model for preoperative prediction of microsatellite instability status in rectal cancer: a retrospective multicenter study. Eur Radiol. 2023;33(3):1835-1843.
Zhang Y, Liu J, Wu C, Peng J, Wei Y, Cui S. Preoperative Prediction of Microsatellite Instability in Rectal Cancer Using Five Machine Learning Algorithms Based on Multiparametric MRI Radiomics. Diagnostics (Basel, Switzerland). 2023;13(2):269.
Paku M, Uemura M, Kitakaze M, et al. Clinical Significance of Preoperative and Postoperative Serum CEA and Carbohydrate Antigen 19-9 Levels in Patients Undergoing Curative Resection of Locally Recurrent Rectal Cancer. Dis Colon Rectum. 2023;66(3):392-400.
Yuan H, Xu X, Tu S, Chen B, Wei Y, Ma Y. The CT-based intratumoral and peritumoral machine learning radiomics analysis in predicting lymph node metastasis in rectal carcinoma. BMC gastroenterology. 2022;22(1):463.
Umar A, Boland CR, Terdiman JP, et al. Revised Bethesda Guidelines for hereditary nonpolyposis colorectal cancer (Lynch syndrome) and microsatellite instability. J Natl Cancer Inst. 2004;96(4):261-268.
Büsing KA, Kilian Ak Fau - Schaible T, Schaible T Fau - Debus A, Debus A Fau - Weiss C, Weiss C Fau - Neff KW, Neff KW. Reliability and validity of MR image lung volume measurement in fetuses with congenital diaphragmatic hernia and in vitro lung models. Radiology. 2008;246(2):553-561.
Koivu A, Sairanen M, Airola A, Pahikkala T. Synthetic minority oversampling of vital statistics data with generative adversarial networks. J Am Med Inform Assoc. 2020;27(11):1667-1674.
Meng WJ, Sun XF, Tian C, et al. Microsatellite instability did not predict individual survival in sporadic stage II and III rectal cancer patients. Oncology. 2007;72(1-2):82-88.
Kawakami H, Zaanan A, Sinicrope FA. Microsatellite instability testing and its role in the management of colorectal cancer. Current treatment options in oncology. 2015;16(7):30.
de la Chapelle A, Hampel H. Clinical relevance of microsatellite instability in colorectal cancer. J Clin Oncol. 2010;28(20):3380-3387.
Ying M, Pan J, Lu G, et al. Development and validation of a radiomics-based nomogram for the preoperative prediction of microsatellite instability in colorectal cancer. BMC cancer. 2022;22(1):524.
Li Z, Dai H, Liu Y, Pan F, Yang Y, Zhang M. Radiomics Analysis of Multi-Sequence MR Images For Predicting Microsatellite Instability Status Preoperatively in Rectal Cancer. Front Oncol. 2021;11:697497.
Acar T, Acar N, Kamer E, et al. Do tumor localization, microsatellite instability and mismatch repair deficiency have an impact on the prognosis of colorectal cancer? Nigerian journal of clinical practice. 2021;24(12):1814-1823.
Cao Y, Zhang G, Zhang J, et al. Predicting Microsatellite Instability Status in Colorectal Cancer Based on Triphasic Enhanced Computed Tomography Radiomics Signatures: A Multicenter Study. Front Oncol. 2021;10(11):687771.
Li M, Jin Y, Rui J, et al. Computed tomography-based radiomics for predicting lymphovascular invasion in rectal cancer. Eur J Radiol. 2022;146:110065.
Funding
Funding was provided by Medical and Health Research Projects of Health Commission of Zhejiang Province (Nos. 2022KY040, 2023KY472).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ma, Y., Xu, X., Lin, Y. et al. An integrative clinical and CT-based tumoral/peritumoral radiomics nomogram to predict the microsatellite instability in rectal carcinoma. Abdom Radiol 49, 783–790 (2024). https://doi.org/10.1007/s00261-023-04099-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-023-04099-2