Abstract
Purpose
Assess use of a diagnostic certainty scale (CS) for abdominal imaging reports and identify factors associated with greater adoption.
Methods
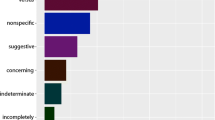
This retrospective, Institutional Review Board-exempt study was conducted at an academic health system. Abdominal radiology reports containing diagnostic certainty phrases (DCPs) generated 4/1/2019–3/31/2021 were identified by a natural language processing tool. Reports containing DCPs were subdivided into those with/without a CS inserted at the end. Primary outcome was monthly CS use rate in reports containing DCPs. Secondary outcomes were assessment of factors associated with CS use, and usage of recommended DCPs over time. Chi-square test was used to compare proportions; univariable and multivariable regression assessed impact of other variables.
Results
DCPs were used in 81,281/124,501 reports (65.3%). One-month post-implementation, 82/2310 (3.6%) of reports with DCPs contained the CS, increasing to 1862/4644 (40.1%) by study completion (p < 0.001). Multivariable analysis demonstrated reports containing recommended DCPs were more likely to have the CS (Odds Ratio [OR] 4.5; p < 0.001). Using CT as a reference, CS use was lower for ultrasound (OR 0.73; p < 0.001) and X-ray (OR 0.38; p < 0.001). There was substantial inter-radiologist variation in CS use (OR 0.01–26.3, multiple p values).
Conclusion
DCPs are very common in abdominal imaging reports and can be further clarified with CS use. Although voluntary CS adoption increased 13-fold over 2 years, > 50% of reports with DCPs lacked the CS at study’s end. More stringent interventions, including embedding the scale in report templates, are likely needed to reduce inter-radiologist variation and decrease ambiguity in conveying diagnostic certainty to referring providers and patients.
Graphical abstract




Similar content being viewed by others
References
Hartung MP, Bickle IC, Gaillard F, Kanne JP (2020) How to Create a Great Radiology Report. Radiogr Rev Publ Radiol Soc N Am Inc 40:1658–1670
Sahni VA, Khorasani R (2016) The actionable imaging report. Abdom Radiol N Y 41:429–443
Lacson R, Odigie E, Wang A, Kapoor N, Shinagare A, Boland G, Khorasani R (2019) Multivariate Analysis of Radiologists’ Usage of Phrases that Convey Diagnostic Certainty. Acad Radiol 26:1229–1234
Shinagare AB, Lacson R, Boland GW, Wang A, Silverman SG, Mayo-Smith WW, Khorasani R (2019) Radiologist Preferences, Agreement, and Variability in Phrases Used to Convey Diagnostic Certainty in Radiology Reports. J Am Coll Radiol JACR 16:458–464
Mityul MI, Gilcrease-Garcia B, Searleman A, Demertzis JL, Gunn AJ (2018) Interpretive Differences Between Patients and Radiologists Regarding the Diagnostic Confidence Associated With Commonly Used Phrases in the Radiology Report. AJR Am J Roentgenol 210:123–126
Gunn AJ, Tuttle MC, Flores EJ, Mangano MD, Bennett SE, Sahani DV, Choy G, Boland GW (2016) Differing Interpretations of Report Terminology Between Primary Care Physicians and Radiologists. J Am Coll Radiol JACR 13:1525-1529.e1
Swensen SJ, Johnson CD (2005) Radiologic Quality and Safety: Mapping Value Into Radiology. J Am Coll Radiol 2:992–1000
Eberhardt SC, Heilbrun ME (2018) Radiology Report Value Equation. RadioGraphics 38:1888–1896
Panicek DM, Hricak H (2016) How Sure Are You, Doctor? A Standardized Lexicon to Describe the Radiologist’s Level of Certainty. AJR Am J Roentgenol 207:2–3
Das JP, Panicek DM (2021) Added Value of a Diagnostic Certainty Lexicon to the Radiology Report. Radiogr Rev Publ Radiol Soc N Am Inc 41:E64–E65
Wibmer A, Vargas HA, Sosa R, Zheng J, Moskowitz C, Hricak H (2014) Value of a standardized lexicon for reporting levels of diagnostic certainty in prostate MRI. AJR Am J Roentgenol 203:W651-657
Shinagare AB, Alper DP, Hashemi SR, Chai JL, Hammer MM, Boland GW, Khorasani R (2020) Early adoption of a certainty scale to improve diagnostic certainty communication. J Am Coll Radiol 17:1276–1284
https://github.com/Center-for-Evidence-Based-Imaging/CEBI-Miner. Accessed 5 Oct 2021.
Acknowledgements
The authors wish to thank Laura Peterson for manuscript editing assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Glazer, D.I., Budiawan, E., Burk, K.S. et al. Adoption of a diagnostic certainty scale in abdominal imaging: 2-year experience at an academic institution. Abdom Radiol 47, 1187–1195 (2022). https://doi.org/10.1007/s00261-021-03391-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-021-03391-3