Abstract
Purpose
R2* relaxometry is a quantitative method for assessment of iron overload. The purpose is to analyze the cross-sectional relationships between R2* in organs across patients with primary and secondary iron overload. Secondary analyses were conducted to analyze R2* according to treatment regimen.
Methods
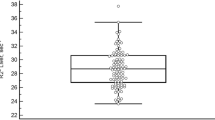
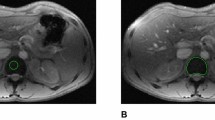
This is a retrospective, cross-sectional, institutional review board-approved study of eighty-one adult patients with known or suspected iron overload. R2* was measured by segmenting the liver, spleen, bone marrow, pancreas, renal cortex, renal medulla, and myocardium using breath-hold multi-echo gradient-recalled echo imaging at 1.5 T. Phlebotomy, transfusion, and chelation therapy were documented. Analyses included correlation, Kruskal–Wallis, and post hoc Dunn tests. p < 0.01 was considered significant.
Results
Correlations between liver R2* and that of the spleen, bone marrow, pancreas, and heart were respectively 0.49, 0.33, 0.27, and 0.34. R2* differed between patients with primary and secondary overload in the liver (p < 0.001), spleen (p < 0.001), bone marrow (p < 0.01), renal cortex (p < 0.001), and renal medulla (p < 0.001). Liver, spleen, and bone marrow R2* were higher in thalassemia than in hereditary hemochromatosis (all p < 0.01). Renal cortex R2* was higher in sickle cell disease than in hereditary hemochromatosis (p < 0.001) and in thalassemia (p < 0.001). Overall, there was a trend toward lower liver R2* in patients assigned to phlebotomy and higher liver R2* in patients assigned to transfusion and chelation therapy.
Conclusion
R2* relaxometry revealed differences in degree or distribution of iron overload between organs, underlying etiologies, and treatment.






Similar content being viewed by others
Abbreviations
- HFE:
-
High iron Fe
- HH:
-
Hereditary hemochromatosis
- MRI:
-
Magnetic resonance imaging
- ROI:
-
Region of interest
- SCD:
-
Sickle cell disease
References
Piperno A (1998) Classification and diagnosis of iron overload. Haematologica 83 (5):447-455
Modell B, Darlison M (2008) Global epidemiology of haemoglobin disorders and derived service indicators. Bull World Health Organ 86 (6):480-487
Esposito BP, Breuer W, Sirankapracha P, Pootrakul P, Hershko C, Cabantchik ZI (2003) Labile plasma iron in iron overload: redox activity and susceptibility to chelation. Blood 102 (7):2670-2677. https://doi.org/10.1182/blood-2003-03-0807
Kew MC (2014) Hepatic iron overload and hepatocellular carcinoma. Liver Cancer 3 (1):31-40. https://doi.org/10.1159/000343856
Siri-Angkul N, Chattipakorn SC, Chattipakorn N (2018) Diagnosis and treatment of cardiac iron overload in transfusion-dependent thalassemia patients. Expert Rev Hematol 11 (6):471-479. https://doi.org/10.1080/17474086.2018.1476134
Gulati V, Harikrishnan P, Palaniswamy C, Aronow WS, Jain D, Frishman WH (2014) Cardiac involvement in hemochromatosis. Cardiol Rev 22 (2):56-68. https://doi.org/10.1097/CRD.0b013e3182a67805
Kwan T, Leber B, Ahuja S, Carter R, Gerstein HC (1998) Patients with type 2 diabetes have a high frequency of the C282Y mutation of the hemochromatosis gene. Clin Invest Med 21 (6):251-257
Brissot P (2016) Optimizing the diagnosis and the treatment of iron overload diseases. Expert Rev Gastroenterol Hepatol 10 (3):359-370. https://doi.org/10.1586/17474124.2016.1119043
Labranche R, Gilbert G, Cerny M, Vu KN, Soulieres D, Olivie D, Billiard JS, Yokoo T, Tang A (2018) Liver Iron Quantification with MR Imaging: A Primer for Radiologists. Radiographics 38 (2):392-412. https://doi.org/10.1148/rg.2018170079
Lande IM, Glazer GM, Sarnaik S, Aisen A, Rucknagel D, Martel W (1986) Sickle-cell nephropathy: MR imaging. Radiology 158 (2):379-383. https://doi.org/10.1148/radiology.158.2.3941863
Midiri M, Lo Casto A, Sparacia G, D'Angelo P, Malizia R, Finazzo M, Montalto G, Solbiati L, Lagalla R, De Maria M (1999) MR imaging of pancreatic changes in patients with transfusion-dependent beta-thalassemia major. AJR American journal of roentgenology 173 (1):187-192. https://doi.org/10.2214/ajr.173.1.10397124
Siegelman ES, Mitchell DG, Rubin R, Hann HW, Kaplan KR, Steiner RM, Rao VM, Schuster SJ, Burk DL, Jr., Rifkin MD (1991) Parenchymal versus reticuloendothelial iron overload in the liver: distinction with MR imaging. Radiology 179 (2):361-366. https://doi.org/10.1148/radiology.179.2.2014275
Villeneuve JP, Bilodeau M, Lepage R, Cote J, Lefebvre M (1996) Variability in hepatic iron concentration measurement from needle-biopsy specimens. Journal of hepatology 25 (2):172-177
Emond MJ, Bronner MP, Carlson TH, Lin M, Labbe RF, Kowdley KV (1999) Quantitative study of the variability of hepatic iron concentrations. Clin Chem 45 (3):340-346
Rockey DC, Caldwell SH, Goodman ZD, Nelson RC, Smith AD, American Association for the Study of Liver D (2009) Liver biopsy. Hepatology 49 (3):1017-1044. https://doi.org/10.1002/hep.22742
Wood JC, Zhang P, Rienhoff H, Abi-Saab W, Neufeld EJ (2015) Liver MRI is more precise than liver biopsy for assessing total body iron balance: a comparison of MRI relaxometry with simulated liver biopsy results. Magnetic resonance imaging 33 (6):761-767. https://doi.org/10.1016/j.mri.2015.02.016
Franca M, Marti-Bonmati L, Porto G, Silva S, Guimaraes S, Alberich-Bayarri A, Vizcaino JR, Pessegueiro Miranda H (2018) Tissue iron quantification in chronic liver diseases using MRI shows a relationship between iron accumulation in liver, spleen, and bone marrow. Clinical radiology 73 (2):215 e211–215 e219. https://doi.org/10.1016/j.crad.2017.07.022
Gutierrez L, House MJ, Vasavda N, Drasar E, Gonzalez-Gascon YMI, Kulasekararaj AG, St Pierre TG, Thein SL (2015) Tissue Iron Distribution Assessed by MRI in Patients with Iron Loading Anemias. PloS one 10 (9):e0139220. https://doi.org/10.1371/journal.pone.0139220
Wood JC (2014) Guidelines for quantifying iron overload. Hematology Am Soc Hematol Educ Program 2014 (1):210-215. https://doi.org/10.1182/asheducation-2014.1.210
Bydder M, Yokoo T, Hamilton G, Middleton MS, Chavez AD, Schwimmer JB, Lavine JE, Sirlin CB (2008) Relaxation effects in the quantification of fat using gradient echo imaging. Magnetic resonance imaging 26 (3):347-359. https://doi.org/10.1016/j.mri.2007.08.012
Wood JC, Enriquez C, Ghugre N, Tyzka JM, Carson S, Nelson MD, Coates TD (2005) MRI R2 and R2* mapping accurately estimates hepatic iron concentration in transfusion-dependent thalassemia and sickle cell disease patients. Blood 106 (4):1460-1465. doi:2004-10-3982
Krzanowski WJ (2000) Principles of multivariate analysis : a user's perspective. Rev. edn. Oxford University Press, Oxford
Papakonstantinou O, Alexopoulou E, Economopoulos N, Benekos O, Kattamis A, Kostaridou S, Ladis V, Efstathopoulos E, Gouliamos A, Kelekis NL (2009) Assessment of iron distribution between liver, spleen, pancreas, bone marrow, and myocardium by means of R2 relaxometry with MRI in patients with beta-thalassemia major. J Magn Reson Imaging 29 (4):853-859. https://doi.org/10.1002/jmri.21707
Brissot P, Troadec MB, Loreal O, Brissot E (2019) Pathophysiology and classification of iron overload diseases; update 2018. Transfusion clinique et biologique : journal de la Societe francaise de transfusion sanguine 26 (1):80-88. https://doi.org/10.1016/j.tracli.2018.08.006
Schein A, Enriquez C, Coates TD, Wood JC (2008) Magnetic resonance detection of kidney iron deposition in sickle cell disease: a marker of chronic hemolysis. J Magn Reson Imaging 28 (3):698-704. https://doi.org/10.1002/jmri.21490
Salgia RJ, Brown K (2015) Diagnosis and management of hereditary hemochromatosis. Clin Liver Dis 19 (1):187-198. https://doi.org/10.1016/j.cld.2014.09.011
Adams PC, Barton JC (2010) How I treat hemochromatosis. Blood 116 (3):317-325. https://doi.org/10.1182/blood-2010-01-261875
Taher AT, Saliba AN (2017) Iron overload in thalassemia: different organs at different rates. Hematology Am Soc Hematol Educ Program 2017 (1):265-271. https://doi.org/10.1182/asheducation-2017.1.265
Coates TD, Wood JC (2017) How we manage iron overload in sickle cell patients. British journal of haematology 177 (5):703-716. https://doi.org/10.1111/bjh.14575
Sirlin CB, Reeder SB (2010) Magnetic resonance imaging quantification of liver iron. Magn Reson Imaging Clin N Am 18 (3):359–381, ix. https://doi.org/10.1016/j.mric.2010.08.014
Hoffbrand AV, Taher A, Cappellini MD (2012) How I treat transfusional iron overload. Blood 120 (18):3657-3669. https://doi.org/10.1182/blood-2012-05-370098
Danielson CF (2002) The role of red blood cell exchange transfusion in the treatment and prevention of complications of sickle cell disease. Ther Apher 6 (1):24-31. https://doi.org/10.1046/j.1526-0968.2002.00396.x
Kim HC (2014) Red cell exchange: special focus on sickle cell disease. Hematology Am Soc Hematol Educ Program 2014 (1):450-456. https://doi.org/10.1182/asheducation-2014.1.450
Yawn BP, Buchanan GR, Afenyi-Annan AN, Ballas SK, Hassell KL, James AH, Jordan L, Lanzkron SM, Lottenberg R, Savage WJ, Tanabe PJ, Ware RE, Murad MH, Goldsmith JC, Ortiz E, Fulwood R, Horton A, John-Sowah J (2014) Management of sickle cell disease: summary of the 2014 evidence-based report by expert panel members. JAMA 312 (10):1033-1048. https://doi.org/10.1001/jama.2014.10517
Pfeifer CD, Schoennagel BP, Grosse R, Wang ZJ, Graessner J, Nielsen P, Adam G, Fischer R, Yamamura J (2015) Pancreatic iron and fat assessment by MRI-R2* in patients with iron overload diseases. J Magn Reson Imaging 42 (1):196-203. https://doi.org/10.1002/jmri.24752
Doyle EK, Toy K, Valdez B, Chia JM, Coates T, Wood JC (2018) Ultra-short echo time images quantify high liver iron. Magnetic resonance in medicine : official journal of the Society of Magnetic Resonance in Medicine / Society of Magnetic Resonance in Medicine 79 (3):1579-1585. https://doi.org/10.1002/mrm.26791
Krafft AJ, Loeffler RB, Song R, Tipirneni-Sajja A, McCarville MB, Robson MD, Hankins JS, Hillenbrand CM (2017) Quantitative ultrashort echo time imaging for assessment of massive iron overload at 1.5 and 3 Tesla. Magnetic resonance in medicine : official journal of the Society of Magnetic Resonance in Medicine / Society of Magnetic Resonance in Medicine. https://doi.org/10.1002/mrm.26592
Allali S, de Montalembert M, Brousse V, Chalumeau M, Karim Z (2017) Management of iron overload in hemoglobinopathies. Transfusion clinique et biologique : journal de la Societe francaise de transfusion sanguine 24 (3):223-226. https://doi.org/10.1016/j.tracli.2017.06.008
Telfer P, Coen PG, Christou S, Hadjigavriel M, Kolnakou A, Pangalou E, Pavlides N, Psiloines M, Simamonian K, Skordos G, Sitarou M, Angastiniotis M (2006) Survival of medically treated thalassemia patients in Cyprus. Trends and risk factors over the period 1980–2004. Haematologica 91 (9):1187–1192
Loiselle K, Lee JL, Szulczewski L, Drake S, Crosby LE, Pai AL (2016) Systematic and Meta-Analytic Review: Medication Adherence Among Pediatric Patients With Sickle Cell Disease. J Pediatr Psychol 41 (4):406-418. https://doi.org/10.1093/jpepsy/jsv084
Fisher SA, Brunskill SJ, Doree C, Chowdhury O, Gooding S, Roberts DJ (2013) Oral deferiprone for iron chelation in people with thalassaemia. Cochrane Database Syst Rev (8):CD004839. https://doi.org/10.1002/14651858.CD004839.pub3
Funding
Funding for this project was supported by Grants from the Canadian Institutes of Health Research (CIHR)-Institute of Nutrition, Metabolism and Diabetes (INMD) (CIHR-INMD #273738 and #301520), from the Fonds de recherche du Québec en Santé (FRQS) and Fondation de l'association des radiologistes du Québec (FARQ) Clinical Research Scholarship – Junior 1 and 2 Salary Awards (FRQS-FARQ #26993 and #34939), and from the Centre de recherche du Centre hospitalier de l’Université de Montréal (CRCHUM) to An Tang.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Aslan, E., Luo, J.W., Lesage, A. et al. MRI-based R2* mapping in patients with suspected or known iron overload. Abdom Radiol 46, 2505–2515 (2021). https://doi.org/10.1007/s00261-020-02912-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-020-02912-w