Abstract
Purpose
To compare computed diffusion-weighted imaging (cDWI) feasibility with that of directly acquired DWI for visualizing pancreatic ductal adenocarcinoma (PDAC) and focal autoimmune pancreatitis (AIP).
Methods
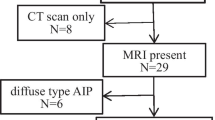
From April 2012 to January 2017, 135 patients with PDAC (n = 111) or focal AIP (n = 24) were retrospectively enrolled. They underwent DWI with b-values of 0, 500, and 1000 s/mm2. From DWI0 and DWI1000, we generated cDWIs with targeted b-values of 1500, 2000, and 3000 s/mm2. The lesions’ signal intensities, image quality, signal intensity ratio (SIR) of lesions and pancreatic parenchyma to spinal cord, and lesion-to-pancreatic parenchyma contrast ratio (CR) were compared among the five DWI protocols (DWI500, DWI1000, cDWI1500, cDWI2000, and cDWI3000). SIR was analyzed by receiver operating characteristic (ROC) analyses.
Results
DWI500, DWI1000, and cDWI1500 had higher image quality than cDWI2000 and cDWI3000 (P < 0.001). The incidence of clear hyperintense PDAC was highest on cDWI2000, followed by cDWI1500, and cDWI3000 (P < 0.001–0.002), while the incidence of clear hyperintense AIP was higher on DWI1000, cDWI1500, and cDWI2000 than on DWI500 and cDWI3000 (P = 0.001–0.022). SIRs decreased whereas CRs increased as the b-value increased, for both PDAC and AIP. The area under the ROC curve (AUC) of SIRlesion was significantly lower on cDWI1500 than on cDWI2000 and cDWI3000 (P < 0.001).
Conclusion
cDWI1500 or cDWI2000 generated from b-values of 0 and 1000 s/mm2 were the most effective for visualizing PDAC and focal AIP; however, the SIRlesion AUC was significantly lower on cDWI1500 than on cDWI2000 and cDWI3000.







Similar content being viewed by others
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424. https://doi.org/10.3322/caac.21492
Yabar CS, Winter JM (2016) Pancreatic cancer: a review. Gastroenterol Clin North Am 45:429–445. https://doi.org/10.1016/j.gtc.2016.04.003.
McGuigan A, Kelly P, Turkington RC, Jones C, Coleman HG, McCain RS (2018) Pancreatic cancer: A review of clinical diagnosis, epidemiology, treatment and outcomes. World J Gastroenterol 24:4846–4861. https://doi.org/10.3748/wjg.v24.i43.4846.
Rawla P, Sunkara T, Gaduputi V (2019) Epidemiology of pancreatic cancer: global trends, etiology and risk factors. World J Oncol 10:10–27. https://doi.org/10.14740/wjon1166.
Nagpal SJS, Sharma A, Chari ST (2018) Autoimmune pancreatitis. Am J Gastroenterol 113:1301. https://doi.org/10.1038/s41395-018-0146-0.
Kwon JH, Kim JH, Kim SY, et al (2019) Differentiating focal autoimmune pancreatitis and pancreatic ductal adenocarcinoma: contrast-enhanced MRI with special emphasis on the arterial phase. Eur Radiol 29:5763–5771. https://doi.org/10.1007/s00330-019-06200-0.
Lee S, Kim JH, Kim SY, et al (2018) Comparison of diagnostic performance between CT and MRI in differentiating non-diffuse-type autoimmune pancreatitis from pancreatic ductal adenocarcinoma. Eur Radiol 28:5267–5274. https://doi.org/10.1007/s00330-018-5565-1.
Kim HJ, Kim YK, Jeong WK, Lee WJ, Choi D (2015) Pancreatic duct “Icicle sign” on MRI for distinguishing autoimmune pancreatitis from pancreatic ductal adenocarcinoma in the proximal pancreas. Eur Radiol 25:1551–1560. https://doi.org/10.1007/s00330-014-3548-4.
Hur BY, Lee JM, Lee JE, et al (2012) Magnetic resonance imaging findings of the mass-forming type of autoimmune pancreatitis: comparison with pancreatic adenocarcinoma. J Magn Reson Imaging 36:188–197. https://doi.org/10.1002/jmri.23609.
Oki H, Hayashida Y, Oki H, et al (2015) DWI findings of autoimmune pancreatitis: comparison between symptomatic and asymptomatic patients. J Magn Reson Imaging 41:125–131. https://doi.org/10.1002/jmri.24508.
Choi SY, Kim SH, Kang TW, Song KD, Park HJ, Choi YH (2016) Differentiating mass-forming autoimmune pancreatitis from pancreatic ductal adenocarcinoma on the basis of contrast-enhanced MRI and DWI findings. AJR Am J Roentgenol 206:291–300. https://doi.org/10.2214/AJR.15.14974.
Muhi A, Ichikawa T, Motosugi U, et al (2012) Mass-forming autoimmune pancreatitis and pancreatic carcinoma: differential diagnosis on the basis of computed tomography and magnetic resonance cholangiopancreatography, and diffusion-weighted imaging findings. J Magn Reson Imaging 35:827–836. https://doi.org/10.1002/jmri.22881.
Kovac JD, Duric-Stefanovic A, Dugalic V, et al (2019) CT perfusion and diffusion-weighted MR imaging of pancreatic adenocarcinoma: can we predict tumor grade using functional parameters? Acta Radiol 60:1065–1073. https://doi.org/10.1177/0284185118812202.
Zong RL, Geng L, Wang X, Xie D (2019) Diagnostic performance of apparent diffusion coefficient for prediction of grading of pancreatic neuroendocrine tumors: a systematic review and meta-analysis. Pancreas 48:151–160. https://doi.org/10.1097/MPA.0000000000001212.
Kawakami S, Fukasawa M, Shimizu T, et al (2019) Diffusion-weighted image improves detectability of magnetic resonance cholangiopancreatography for pancreatic ductal adenocarcinoma concomitant with intraductal papillary mucinous neoplasm. Medicine (Baltimore) 98:e18039. https://doi.org/10.1097/MD.0000000000018039.
Fukukura Y, Shindo T, Hakamada H, et al (2016) Diffusion-weighted MR imaging of the pancreas: optimizing b-value for visualization of pancreatic adenocarcinoma. Eur Radiol 26:3419–3427. https://doi.org/10.1007/s00330-015-4174-5.
Higaki T, Nakamura Y, Tatsugami F, et al (2018) Introduction to the technical aspects of computed diffusion-weighted imaging for radiologists. Radiographics 38:1131–1144. https://doi.org/10.1148/rg.2018170115.
Ueno YR, Tamada T, Takahashi S, et al (2018) Computed diffusion-weighted imaging in prostate cancer: basics, advantages, cautions, and future prospects. Korean J Radiol 19:832–837. https://doi.org/10.3348/kjr.2018.19.5.832.
Tamura T, Takasu M, Higaki T, et al (2019) How to improve the conspicuity of breast tumors on computed high b-value diffusion-weighted imaging. Magn Reson Med Sci 18:119–125. https://doi.org/10.2463/mrms.mp.2018-0011.
Akagi M, Nakamura Y, Higaki T, et al (2018) Preliminary results of high-precision computed diffusion weighted imaging for the diagnosis of hepatocellular carcinoma at 3 Tesla. J Comput Assist Tomogr 42:373–379. https://doi.org/10.1097/RCT.0000000000000702.
Moribata Y, Kido A, Fujimoto K, et al (2017) Feasibility of computed diffusion weighted imaging and optimization of b-value in cervical cancer. Magn Reson Med Sci 16:66–72. https://doi.org/10.2463/mrms.mp.2015-0161.
Takeuchi M, Matsuzaki K, Harada M (2016) Computed diffusion-weighted imaging for differentiating decidualized endometrioma from ovarian cancer. Eur J Radiol 85:1016–1019. https://doi.org/10.1016/j.ejrad.2016.03.009.
Yamashita K, Hiwatashi A, Togao O, et al (2019) Improved visualization of middle ear cholesteatoma with computed diffusion-weighted imaging. Magn Reson Med Sci 18:233–237. https://doi.org/10.2463/mrms.tn.2018-0068.
Fukukura Y, Kumagae Y, Hakamada H, et al (2017) Computed diffusion-weighted MR imaging for visualization of pancreatic adenocarcinoma: Comparison with acquired diffusion-weighted imaging. Eur J Radiol 95:39–45. https://doi.org/10.1016/j.ejrad.2017.07.022.
Tokunaga K, Arizono S, Shimizu H, et al (2020) Optimizing b-values for accurate depiction of pancreatic cancer with tumor-associated pancreatitis on computed diffusion-weighted imaging. Clin Imaging 61:20–26. https://doi.org/10.1016/j.clinimag.2020.01.007.
Shimosegawa T, Working Group Members of the Japan Pancreas S, Research Committee for Intractable Pancreatic Disease by the Ministry of Labor H, Welfare of J (2012) The amendment of the Clinical Diagnostic Criteria in Japan (JPS2011) in response to the proposal of the International Consensus of Diagnostic Criteria (ICDC) for autoimmune pancreatitis. Pancreas 41:1341–1342. https://doi.org/10.1097/MPA.0b013e3182706ed5.
Moore WA, Khatri G, Madhuranthakam AJ, Sims RD, Pedrosa I (2014) Added value of diffusion-weighted acquisitions in MRI of the abdomen and pelvis. AJR Am J Roentgenol 202:995–1006. https://doi.org/10.2214/AJR.12.9563.
Koh DM, Lee JM, Bittencourt LK, Blackledge M, Collins DJ (2016) Body diffusion-weighted MR imaging in oncology: imaging at 3 T. Magn Reson Imaging Clin N Am 24:31–44. https://doi.org/10.1016/j.mric.2015.08.007.
Kamisawa T, Takuma K, Anjiki H, et al (2010) Differentiation of autoimmune pancreatitis from pancreatic cancer by diffusion-weighted MRI. Am J Gastroenterol 105:1870–1875. https://doi.org/10.1097/MD.0000000000018039.
Majumder S, Takahashi N, Chari ST (2017) Autoimmune pancreatitis. Dig Dis Sci 62:1762–1769. https://doi.org/10.1007/s10620-017-4541-y.
Hart PA, Zen Y, Chari ST (2015) Recent Advances in autoimmune pancreatitis. Gastroenterology 149:39–51. https://doi.org/10.1053/j.gastro.2015.03.010.
Funding
This research received no specific grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ichikawa, S., Kromrey, ML., Motosugi, U. et al. Optimal target b-value on computed diffusion-weighted magnetic resonance imaging for visualization of pancreatic ductal adenocarcinoma and focal autoimmune pancreatitis. Abdom Radiol 46, 636–646 (2021). https://doi.org/10.1007/s00261-020-02695-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-020-02695-0