Abstract
Objective
This study sought to evaluate the role of diffusion-weighted imaging (DWI) in differentiation between obstructed and unobstructed bile ducts in patients undergoing magnetic resonance imaging (MRI).
Methods
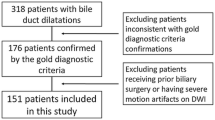
Eighty-four patients, 40 males and 44 females (mean age: 56.4 ± 15.1 years), undergoing MRI with DWI (0–50–500–700) were evaluated and divided into two groups: 58 with abnormal laboratory tests (obstructed group) and 26 with normal laboratory values (unobstructed group). Laboratory tests were total bilirubin, alkaline phosphatase, and gamma-glutamyltransferase. Median ADC values were calculated and correlated with laboratory tests and degree of bile-duct dilatation (absent, moderate, or severe). The persistence of signal on DWI (b500 and b700) in the biliary tract was evaluated. Bilirubin values were tested for correlation with bile-duct ADC values and persistence of b700 signal. For statistical analysis, Student t test, chi-square test and Wilcoxon–Mann–Whitney test were used. ADC maps were plotted for three levels of the biliary tree, and a receiver operating characteristic (ROC) curve was calculated.
Results
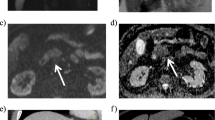
In the obstructed group, 15 patients had severe dilatation, 24 had moderate dilatation, and 19 had no appreciable dilatation; 38 patients had persistent signal on b700 images. In the unobstructed group, 23 patients had no dilatation and 3 had moderate dilatation; 4 patients had persistent signal on b700 images. Correlation was found between degree of bile-duct dilatation, bilirubin levels, persistence of b700 signal, and ADC map values. The calculated ADC map cutoff value (353 10–6 mm2/s) was able to differentiate the obstructed and unobstructed groups with 92.3% sensitivity, 81% specificity, and 91.9% accuracy.
Conclusions
DWI is able to distinguish patients with obstructed versus unobstructed bile ducts, regardless of the degree of dilatation, correlating with clinical and laboratory findings.








Similar content being viewed by others
Abbreviations
- ERCP:
-
Endoscopic retrograde cholangiopancreatography
- MRCP:
-
Magnetic resonance cholangiopancreatography
- MRI:
-
Magnetic resonance Imaging
- SNR:
-
Signal-to-noise ratio
- DWI:
-
Diffusion-weighted imaging
- ADC:
-
Apparent diffusion coefficient
- ROI:
-
Region-of-interest imaging
- NOG:
-
Unobstructed group
- OG:
-
Obstruction group
- TR:
-
Repetition time
- TE:
-
Echo time
- FOV:
-
Field of view
- CSF:
-
Cerebrospinal fluid
References
Mincis M (2002) Gastroenterologia e hepatologia – diagnóstico e tratamento, 3ª ed. Lemos Editorial, São Paulo: Lemos Editorial
Pérez Fernández T, López Serrano P, Tomás E, et al (2004) Diagnostic and therapeutic approach to cholestatic liver disease. Rev Esp Enferm Dig. https://doi.org/10.4321/s1130-01082004000100008
Rege RV(1995) Adverse effects of biliary obstruction: implications for treatment of patients with obstructive jaundice. AJR Am J Roentgenol. https://doi.org/10.2214/ajr.164.2.7839957
Singh A, Mann HS, Thukral CL, et al (2014) Diagnostic Accuracy of MRCP as Compared to Ultrasound/CT in Patients with Obstructive Jaundice. J Clin Diagn Res. https://doi.org/10.7860/JCDR/2014/8149.4120
Hünerbein M, Stroszczynski C, Ulmer C, et al (2003) Prospective comparison of transcutaneous 3-dimensional US cholangiography, magnetic resonance cholangiography, and direct cholangiography in the evaluation of malignant biliary obstruction. Gastrointest Endosc. https://doi.org/10.1016/S0016-5107(03)02302-2
EASL (2016) Clinical Practice Guidelines on the prevention, diagnosis and treatment of gallstones. J Hepatol. https://doi.org/10.1016/j.jhep.2016.03.005
Kujawski K, Stasiak M, Rysz J (2015) Qualification for endoscopic retrograde cholangiopancreatography in the diagnosis and treatment of extrahepatic cholestasis caused by choledocholithiasis. Arch Med Sci. https://doi.org/10.5114/aoms.2015.56347
Brugge WR, Van Dam J (1999) Pancreatic and biliary endoscopy. N Engl J Med. https://doi.org/10.1056/NEJM199912093412406
Borges AC, Almeida PC, Furlani SMT, et al (2018) ERCP performance in a tertiary brasilian center: Focus on new risk factors, complications and quality indicators. Arq Bras Cir Dig. https://doi.org/10.1590/0102-672020180001e1348
Artifon EL, Nakadomari TS, Kashiwagui LY, et al (2016) An innovative ex-vivo model for rapid change oh the papilla for teaching advanced endoscopis retrograde cholangiopancreatography procedures. Arq Bras Cir Dig. https://doi.org/10.1590/0102-6720201600040013
Pannu HK, Fishman EK (2001) Complications of endoscopic retrograde cholangiopancreatography: spectrum of abnormalities demonstrated with CT. Radiographics. https://doi.org/10.1148/radiographics.21.6.g01nv101441
Zuber-Jerger I, Endlicher E, Kullmann F, Gelbmann CM (2009) A new grading system to evaluate the risk of endoscopic retrograde cholangiopancreatography. J Gastroenterol. https://doi.org/10.1007/s00535-008-2295-1
Mine T, Morizane T, Kawaguchi Y, et al (2017) Clinical practice guideline for post-ERCP pancreatitis. J Gastroenterol. https://doi.org/10.1007/s00535-017-1359-5
Hurter D, De Vries C, Potgieter P, Barry R, Botha F, Joubert G (2008) Accuracy of MRCP compared to ERCP in the diagnosis of bile duct disorders. South African J Radiol. https://doi.org/10.4102/sajr.v12i1.580
Osman NM, Mohammad SA, Khalil RM (2016) Diagnostic benefit of MRCP in hepatopancreaticobiliary diseases in children. The Egyptian Journal of Radiology and Nuclear Medicine. https://doi.org/10.1016/j.ejrnm.2015.10.012
Watanabe Y, Nagayama M, Okumura A, et al (2007) MR imaging of acute biliary disorders. Radiographics. https://doi.org/10.1148/rg.272055148
Ressureição J, Batista L, Almeida AT, Monteiro D, Almeida N (2014) [“Biliary map”: a review of normal anatomy and main anatomic variants of the biliary tree at MRCP]. Acta Radiol Portuguesa. 103:37-42.
Joo I, Lee JM, Yoon JH (2018) Imaging Diagnosis of Intrahepatic and Perihilar Cholangiocarcinoma: Recent Advances and Challenges. Radiology. https://doi.org/10.1148/radiol.2018171187
Katabathina VS, Dasyam AK, Dasyam N, et al (2014) Adult Bile Duct Strictures: Role of MR Imaging and MR Cholangiopancreatography in Characterization. Radiographics. https://doi.org/10.1148/rg.343125211
Romagnuolo J, Bardou M, Rahme E, et al (2003) Magnetic resonance cholangiopancreatography: a meta-analysis of test performance in suspected biliary disease. Ann Intern Med. https://doi.org/10.7326/0003-4819-139-7-200310070-00006
Ferrucci JT (1999) MRI and MRCP in pancreaticobiliary malignancy. Ann Oncol. https://doi.org/10.1023/a:1008364130766
Pavone P, Laghi A, Passariello R (1999) MR cholangiopancreatography in malignant biliary obstruction. Semin Ultrasound CT MR. 1999;20:317-23.
Vitellas KM, Keogan MT, Spritzer CE (2000) MR cholangiopancreatography of bile and pancreatic duct abnormalities with emphasis on the single-shot fast spin-echo technique. Radiographics. https://doi.org/10.1148/radiographics.20.4.g00jl23939
Hyodo T, Kumano S, Kushihata F, et al (2012) CT and MR cholangiography: advantages and pitfalls in perioperative evaluation of biliary tree. Br J Radiol. https://doi.org/10.1259/bjr/21209407
Watanabe Y, Dohke M, Ishimori T, et al (2000) Pseudo-obstruction of the extrahepatic bile duct due to artifact from arterial pulsatile compression: a diagnostic pitfall of MR cholangiopancreatography. Radiology. https://doi.org/10.1148/radiology.214.3.r00mr09856
Watanabe Y, Dohke M, Ishimori T, et al (1999) Diagnostic pitfalls of MR cholangiopancreatography in the evaluation of the biliary tract and gallbladder. Radiographics. https://doi.org/10.1148/radiographics.19.2.g99mr02415
Irie H, Honda H, Kuroiwa T, et al (2001) Pitfalls in MR cholangiopancreatographic interpretation. Radiographics. https://doi.org/10.1148/radiographics.21.1.g01ja0523
Walser EM, Runyan BR, Heckman MG, et al (2011) Extrahepatic portal biliopathy: proposed etiology on the basis of anatomic and clinical features. Radiology. https://doi.org/10.1148/radiol.10090923
Mortelé KJ, Ros PR (2001) Anatomic variants of the biliary tree: MR cholangiographic findings and clinical applications. AJR Am J Roentgenol. https://doi.org/10.2214/ajr.177.2.1770389
Dohke M, Watanabe Y, Okumura A, et al (1999) Anomalies and anatomic variants of the biliary tree revealed by MR cholangiopancreatography. AJR Am J Roentgenol. 173:1251-4.
de Freitas Tertulino F, Schraibman V, Ardengh JC, et al (2015) Diffusion-weighted magnetic resonance imaging indicates the severity of acute pancreatitis. Abdom Imaging. https://doi.org/10.1007/s00261-014-0205-y
Lee NK, Kim S, Kim GH, et al (2012) Diffusion-weighted imaging of biliopancreatic disorders: correlation with conventional magnetic resonance imaging. World J Gastroenterol. https://doi.org/10.3748/wjg.v18.i31.4102
Wang J, Liu JJ, Liang YY, et al (2012) Could diffusion-weighted imaging detect injured bile ducts of ischemic-type biliary lesions after orthotopic liver transplantation? AJR Am J Roentgenol. https://doi.org/10.2214/AJR.11.8147
Lee NK, Kim S, Kim DU, et al (2015) Diffusion-weighted magnetic resonance imaging for non-neoplastic conditions in the hepatobiliary and pancreatic regions: pearls and potential pitfalls in imaging interpretation. Abdom Imaging. https://doi.org/10.1007/s00261-014-0235-5
Ogawa T, Horaguchi J, Fujita N, et al (2012) High b-value diffusion-weighted magnetic resonance imaging for gallbladder lesions: differentiation between benignity and malignancy. J Gastroenterol. https://doi.org/10.1007/s00535-012-0604-1
Francisco FA, de Araujo AL, Oliveira Neto JA, Parente DB (2014) Hepatobiliary contrast agents: differential diagnosis of focal hepatic lesions, pitfalls and other indications. Radiol Bras. https://doi.org/10.1590/0100-3984.2013.1867
Sheppard D, Allan L, Martin P, et al (2004) Contrast-enhanced magnetic resonance cholangiography using mangafodipir compared with standard T2W MRC sequences: a pictorial essay. J Magn Reson Imaging. https://doi.org/10.1002/jmri.20114
Lee NK, Kim S, Lee JW, et al (2009) Biliary MR imaging with Gd-EOB-DTPA and its clinical applications. Radiographics. https://doi.org/10.1148/rg.296095501
Gupta RT, Brady CM, Lotz J, et al (2010) Dynamic MR imaging of the biliary system using hepatocyte-specific contrast agents. AJR Am J Roentgenol. https://doi.org/10.2214/AJR.09.3641
Fayad LM, Kamel IR, Mitchell DG, et al (2005) Functional MR cholangiography: diagnosis of functional abnormalities of the gallbladder and biliary tree. AJR Am J Roentgenol. https://doi.org/10.2214/ajr.184.5.01841563
Van Beers BE, Pastor CM, Hussain HK (2012) Primovist, Eovist: what to expect? J Hepatol. https://doi.org/10.1016/j.jhep.2012.01.031
Marckmann P, Skov L, Rossen K, et al (2006) Nephrogenic systemic fibrosis: suspected causative role of gadodiamide used for contrast-enhanced magnetic resonance imaging. J Am Soc Nephrol. https://doi.org/10.1681/ASN.2006060601
de Campos RO, Heredia V, Ramalho M, et al (2011) Quarter-dose (0.025 mmol/kg) gadobenate dimeglumine for abdominal MRI in patients at risk for nephrogenic systemic fibrosis: preliminary observations. AJR Am J Roentgenol. https://doi.org/10.2214/AJR.10.4500.
Song KD, Kim SH, Lee J, et al (2015) Half-dose gadoxetic acid-enhanced liver magnetic resonance imaging in patients at risk for nephrogenic systemic fibrosis. Eur J Radiol. https://doi.org/10.1016/j.ejrad.2014.12.010
Prince MR, Zhang HL, Prowda JC, et al (2009) Nephrogenic systemic fibrosis and its impact on abdominal imaging. Radiographics. https://doi.org/10.1148/rg.296095517
Lauenstein T, Ramirez-Garrido F, Kim YH, et al (2015) Nephrogenic systemic fibrosis risk after liver magnetic resonance imaging with gadoxetate disodium in patients with moderate to severe renal impairment: results of a prospective, open-label, multicenter study. Invest Radiol. https://doi.org/10.1097/RLI.0000000000000145
Schwope RB, May LA, Reiter MJ, et al (2015) Gadoxetic acid: pearls and pitfalls. Abdom Imaging. https://doi.org/10.1007/s00261-015-0354-7
Goodwin MD, Dobson JE, Sirlin CB, et al (2011) Diagnostic challenges and pitfalls in MR imaging with hepatocyte-specific contrast agents. Radiographics. https://doi.org/10.1148/rg.316115528
Acknowledgements
This study was financed in part by Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), Brazil (funding code 001).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Paro, E.D.L., Puchnick, A., Szejnfeld, J. et al. Use of diffusion-weighted imaging in the noninvasive diagnostic of obstructed biliary ducts. Abdom Radiol 46, 268–279 (2021). https://doi.org/10.1007/s00261-020-02636-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-020-02636-x