Abstract
Purpose
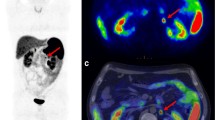
Metastatic gastroenteropancreatic neuroendocrine neoplasms (mGEP-NEN) are indolent malignancies which undergo frequent imaging follow-up. Hepatocellular phase (HCP) MR with hepatocellular-specific contrast agent is widely used to evaluate mGEP-NEN liver metastases but is commonly performed after a 20-min delay which prolongs scan time. The purpose of this study was to evaluate if HCP MR at 15 min offers comparable performance to 20-min delay for patients with mGEP-NEN undergoing routine imaging surveillance.
Materials and methods
In this IRB-approved retrospective study, we evaluated 52 patients with mGEP-NEN who were imaged for routine surveillance with gadoxetate disodium (Eovist®)-enhanced MR including 15- and 20-min delayed HCP. Two readers (R1, R2), blinded to HCP timing, independently reviewed each set of images in random order at least 1 month apart. Readers assessed presence and conspicuity of metastases, and subjective image quality using 5-point scales. Readers quantified the number of metastases and diameter of the largest lesion. Statistical analysis was performed to determine individual-reader and inter-reader differences for qualitative and quantitative data.
Results
No differences were observed for subjective image quality (R1 p = 0.86, R2 p = 0.17) or lesion conspicuity (R1 p = 0.56, R2 p = 0.74) at 15 min and 20 min for either reader. Individual-reader concordance correlation coefficient between 15 and 20 min was high for number of metastases detected (R1 = 0.9842, R2 = 0.9579) and diameter of largest metastasis (R1 = 0.9629, R2 = 0.8859).
Conclusion
HCP imaging at 15 min provides similar diagnostic yield to standard 20-min delay, which may help reduce the scan time and costs, and improve throughput and patient satisfaction.






Similar content being viewed by others
References
Yao JC, Hassan M, Phan A, Dagohoy C, Leary C, Mares JE, et al. One Hundred Years After “Carcinoid”: Epidemiology of and Prognostic Factors for Neuroendocrine Tumors in 35,825 Cases in the United States. Journal of Clinical Oncology. 2008 Jun 20;26(18):3063–72.
Sahani DV, Bonaffini PA, Fernández–Del Castillo C, Blake MA. Gastroenteropancreatic Neuroendocrine Tumors: Role of Imaging in Diagnosis and Management. Radiology. 2013 Jan 1;266(1):38–61.
King J, Quinn R, Glenn DM, Janssen J, Tong D, Liaw W, et al. Radioembolization with selective internal radiation microspheres for neuroendocrine liver metastases. Cancer. 2008;113(5):921–9.
Henn AR, Levine EA, McNulty W, Zagoria RJ. Percutaneous Radiofrequency Ablation of Hepatic Metastases for Symptomatic Relief of Neuroendocrine Syndromes. American Journal of Roentgenology. 2003 Oct 1;181(4):1005–10.
Janson ET, Holmberg L, Stridsberg M, Eriksson B, Theodorsson E, Wilander E, et al. Carcinoid tumors: analysis of prognostic factors and survival in 301 patients from a referral center. Ann Oncol. 1997 Jul;8(7):685–90.
Morin C, Drolet S, Daigle C, Deshaies I, Ouellet J-F, Ball CG, et al. Additional value of gadoxetic acid-enhanced MRI to conventional extracellular gadolinium-enhanced MRI for the surgical management of colorectal and neuroendocrine liver metastases. HPB [Internet]. 2019 Oct 19 [cited 2020 Mar 9]; Available from: http://www.sciencedirect.com/science/article/pii/S1365182X1930721X
Sundin A, Arnold R, Baudin E, Cwikla JB, Eriksson B, Fanti S, et al. ENETS Consensus Guidelines for the Standards of Care in Neuroendocrine Tumors: Radiological, Nuclear Medicine and Hybrid Imaging. NEN [Internet]. 2017 Mar 30 [cited 2017 May 6];(0). Available from: http://www.karger.com.ezp-prod1.hul.harvard.edu/Article/Abstract/471879
Howe JR, Merchant NB, Conrad C, Keutgen XM, Hallet J, Drebin JA, et al. The North American Neuroendocrine Tumor Society Consensus Paper on the Surgical Management of Pancreatic Neuroendocrine Tumors. Pancreas. 2020 Jan;49(1):1–33.
Babazadeh NT, Schlund DJ, Cornelius T, Singh JS, Tierney JF, Chen M, et al. Should 68 Ga-DOTATATE PET/CT be Performed Routinely in Patients with Neuroendocrine Tumors Before Surgical Resection? World J Surg. 2020 Feb 1;44(2):604–11.
Tirumani SH, Jagannathan JP, Braschi-Amirfarzan M, Qin L, Balthazar P, Ramaiya NH, et al. Value of hepatocellular phase imaging after intravenous gadoxetate disodium for assessing hepatic metastases from gastroenteropancreatic neuroendocrine tumors: comparison with other MRI pulse sequences and with extracellular agent. Abdom Radiol. 2018 Feb 22;1–11.
Cruite I, Schroeder M, Merkle EM, Sirlin CB. Gadoxetate Disodium–Enhanced MRI of the Liver: Part 2, Protocol Optimization and Lesion Appearance in the Cirrhotic Liver. American Journal of Roentgenology. 2010 Jul 1;195(1):29–41.
Muhi A, Ichikawa T, Motosugi U, Sou H, Sano K, Araki T. Diffusion- and T2-weighted MR Imaging of the Liver: Effect of Intravenous Administration of Gadoxetic Acid Disodium. MRMS. 2012 Sep 1;11(3):185–91.
Lee D, Cho E-S, Kim DJ, Kim JH, Yu J-S, Chung J-J. Validation of 10-Minute Delayed Hepatocyte Phase Imaging with 30° Flip Angle in Gadoxetic Acid-Enhanced MRI for the Detection of Liver Metastasis. PLOS ONE. 2015 Oct 7;10(10):e0139863.
Lee SE, An C, Hwang SH, Choi J-Y, Han K, Kim M-J. Extracellular contrast agent-enhanced MRI: 15-min delayed phase may improve the diagnostic performance for hepatocellular carcinoma in patients with chronic liver disease. Eur Radiol. 2018 Apr 1;28(4):1551–9.
van Kessel CS, Veldhuis WB, van den Bosch M a. a. J, van Leeuwen MS. MR liver imaging with Gd-EOB-DTPA: a delay time of 10 minutes is sufficient for lesion characterisation. Eur Radiol. 2012 Oct;22(10):2153–60.
Bashir MR, Breault SR, Braun R, Do RK, Nelson RC, Reeder SB. Optimal Timing and Diagnostic Adequacy of Hepatocyte Phase Imaging with Gadoxetate-Enhanced Liver MRI. Academic Radiology. 2014 Jun 1;21(6):726–32.
Liang M, Zhao J, Xie B, Li C, Yin X, Cheng L, et al. MR liver imaging with Gd-EOB-DTPA: The need for different delay times of the hepatobiliary phase in patients with different liver function. European Journal of Radiology. 2016 Mar 1;85(3):546–52.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: Revised RECIST guideline (version 1.1). European Journal of Cancer. 2009 Jan 1;45(2):228–47.
McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb). 2012 Oct 15;22(3):276–82.
Lin LI. A concordance correlation coefficient to evaluate reproducibility. Biometrics. 1989 Mar;45(1):255–68.Lin LI. A concordance correlation coefficient to evaluate reproducibility. Biometrics. 1989 Mar;45(1):255–68.
Giavarina D. Understanding Bland Altman analysis. Biochem Med (Zagreb). 2015;25(2):141–51.
Fukumoto W, Nakamura Y, Higaki T, Tatsugami F, Iida M, Awai K. Additional Value of Diffusion-weighted MRI to Gd-EOB-DTPA-enhanced Hepatic MRI for the Detection of Liver Metastasis: the Difference Depending on the Experience of the Radiologists. Hiroshima J Med Sci. 2015 Jun;64(1–2):15–21.
Besa C, Lewis S, Pandharipande PV, Chhatwal J, Kamath A, Cooper N, et al. Hepatocellular carcinoma detection: diagnostic performance of a simulated abbreviated MRI protocol combining diffusion-weighted and T1-weighted imaging at the delayed phase post gadoxetic acid. Abdominal Radiology. 2017 Jan;42(1):179–90.
Marks RM, Ryan A, Heba ER, Tang A, Wolfson TJ, Gamst AC, et al. Diagnostic Per-Patient Accuracy of an Abbreviated Hepatobiliary Phase Gadoxetic Acid–Enhanced MRI for Hepatocellular Carcinoma Surveillance. American Journal of Roentgenology. 2015 Feb 25;204(3):527–35.
Sofue K, Tsurusaki M, Tokue H, Arai Y, Sugimura K. Gd-EOB-DTPA-enhanced 3.0 T MR imaging: quantitative and qualitative comparison of hepatocyte-phase images obtained 10 min and 20 min after injection for the detection of liver metastases from colorectal carcinoma. Eur Radiol. 2011 Nov 1;21(11):2336.
Motosugi U, Ichikawa T, Tominaga L, Sou H, Sano K, Ichikawa S, et al. Delay before the hepatocyte phase of Gd-EOB-DTPA-enhanced MR imaging: Is it possible to shorten the examination time? Eur Radiol. 2009 Nov 1;19(11):2623.
Jeong HT, Kim M-J, Park M-S, Choi J-Y, Choi JS, Kim KS, et al. Detection of liver metastases using gadoxetic-enhanced dynamic and 10- and 20-minute delayed phase MR imaging. Journal of Magnetic Resonance Imaging. 2012;35(3):635–43.
Forshaw KL, Boyes AW, Carey ML, Hall AE, Symonds M, Brown S, et al. Raised Anxiety Levels Among Outpatients Preparing to Undergo a Medical Imaging Procedure: Prevalence and Correlates. Journal of the American College of Radiology. 2018 Apr 1;15(4):630–8.
Ahmad R, Hu HH, Krishnamurthy R, Krishnamurthy R. Reducing sedation for pediatric body MRI using accelerated and abbreviated imaging protocols. Pediatr Radiol. 2018 Jan 1;48(1):37–49.
Grimm LJ, Soo MS, Yoon S, Kim C, Ghate SV, Johnson KS. Abbreviated Screening Protocol for Breast MRI: A Feasibility Study. Academic Radiology. 2015 Sep 1;22(9):1157–62.
Harvey SC, Di Carlo PA, Lee B, Obadina E, Sippo D, Mullen L. An Abbreviated Protocol for High-Risk Screening Breast MRI Saves Time and Resources. Journal of the American College of Radiology. 2016 Nov 1;13(11, Supplement):R74–80.
Duong P-AT, Pastel DA, Sadigh G, Ballard D, Sullivan JC, Bresnahan B, et al. The Value of Imaging Part II: Value beyond Image Interpretation. Academic Radiology. 2016 Jan 1;23(1):23–9.
Vilgrain V, Esvan M, Ronot M, Caumont-Prim A, Aubé C, Chatellier G. A meta-analysis of diffusion-weighted and gadoxetic acid-enhanced MR imaging for the detection of liver metastases. Eur Radiol. 2016 Dec;26(12):4595–615.
Dromain C, de Baere T, Baudin E, Galline J, Ducreux M, Boige V, et al. MR Imaging of Hepatic Metastases Caused by Neuroendocrine Tumors: Comparing Four Techniques. American Journal of Roentgenology. 2003 Jan 1;180(1):121–8.
Soyer P, Gueye C, Somveille E, Laissy JP, Scherrer A. MR diagnosis of hepatic metastases from neuroendocrine tumors versus hemangiomas: relative merits of dynamic gadolinium chelate-enhanced gradient-recalled echo and unenhanced spin-echo images. American Journal of Roentgenology. 1995 Dec 1;165(6):1407–13.
Davenport MS, Viglianti BL, Al-Hawary MM, Caoili EM, Kaza RK, Liu PSC, et al. Comparison of Acute Transient Dyspnea after Intravenous Administration of Gadoxetate Disodium and Gadobenate Dimeglumine: Effect on Arterial Phase Image Quality. Radiology. 2013 Feb 1;266(2):452–61.
Bhosale P, Kwek JW, Iyer R, Wei W, Bassett R, Kundra V. Follow-Up of Known Carcinoid Liver Metastases: Is Respiratory-Gated T2 Fast Spin-Echo Enough? NEN. 2011;93(4):241–8.
Moalla S, Arfi Rouche J, Foulon S, Caramella C, Ternes N, Planchard D, et al. Are we reproducible in measurement of NET liver metastasis? Digestive and Liver Disease. 2017 Oct 1;49(10):1121–7.
Lavelle LP, O’Neill AC, McMahon CJ, Cantwell CP, Heffernan EJ, Malone DE, et al. Is diffusion-weighted MRI sufficient for follow-up of neuroendocrine tumour liver metastases? Clinical Radiology. 2016 Sep;71(9):863–8.
Sankowski AJ, Ćwikła JB, Nowicki ML, Chaberek S, Pech M, Lewczuk A, et al. The clinical value of MRI using single-shot echoplanar DWI to identify liver involvement in patients with advanced gastroenteropancreatic-neuroendocrine tumors (GEP-NETs), compared to FSE T2 and FFE T1 weighted image after i.v. Gd-EOB-DTPA contrast enhancement. Med Sci Monit. 2012 May 1;18(5):MT33–40.
Razek AAKA, Massoud SMA, Azziz MRA, El-Bendary MM, Zalata K, Motawea EM. Prediction of esophageal varices in cirrhotic patients with apparent diffusion coefficient of the spleen. Abdom Imaging. 2015 Aug 1;40(6):1465–9.
Besa C, Ward S, Cui Y, Jajamovich G, Kim M, Taouli B. Neuroendocrine liver metastases: Value of apparent diffusion coefficient and enhancement ratios for characterization of histopathologic grade. J Magn Reson Imaging. 2016 Dec 1;44(6):1432–41.
Luersen GF, Wei W, Tamm EP, Bhosale PR, Szklaruk J. Evaluation of Magnetic Resonance (MR) Biomarkers for Assessment of Response With Response Evaluation Criteria in Solid Tumors: Comparison of the Measurements of Neuroendocrine Tumor Liver Metastases (NETLM) With Various MR Sequences and at Multiple Phases of Contrast Administration. J Comput Assist Tomogr. 2016 Oct;40(5):717–22.
Morse B, Jeong D, Thomas K, Diallo D, Strosberg JR. Magnetic Resonance Imaging of Neuroendocrine Tumor Hepatic Metastases: Does Hepatobiliary Phase Imaging Improve Lesion Conspicuity and Interobserver Agreement of Lesion Measurements? Pancreas. 2017 Oct;46(9):1219–24.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Caton, M.T., Shinagare, A.B., Lee, B. et al. Optimization of timing of hepatocellular phase imaging after gadoxetate disodium injection for evaluation of patients with neuroendocrine tumor. Abdom Radiol 45, 2358–2369 (2020). https://doi.org/10.1007/s00261-020-02515-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-020-02515-5