Abstract
Purpose
To retrospectively assess the relative diagnostic utility of radiologist-recommended ultrasound (US) following emergency department (ED) abdominal and pelvic computed tomography (CT) in patients with non-traumatic abdominal and/or pelvic pain.
Methods
Blinded to clinical outcomes, two radiology residents and an attending radiologist reviewed radiology reports and relevant medical records for all adult patients from EDs at two academic medical centers from one institution over a 3-year time period, who underwent abdominal/pelvic US within 72 h of an initial IV contrast-enhanced abdominal and pelvic CT for non-traumatic abdominal and/or pelvic pain. Incremental diagnostic utility of subsequent US was deemed present when (1) US findings were discordant with those at CT, or (2) findings were concordant, but US yielded additional relevant diagnostic information. Diagnostic utility was stratified by whether examinations were radiologist-recommended or independently ordered by treating physicians.
Results
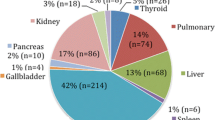
319 encounters satisfied the inclusion criteria, including 194 female patients (18–98 years of age, mean of 59.8 years) and 125 male patients (20–90 years of age, mean of 63.2 years). 7 (2.2%) subsequent US examinations were discordant with the initial CT, 100 (31.3%) were concordant but provided relevant additional information, and 212 (66.5%) were concordant without providing additional information, for an overall diagnostic utility of 33.5%. Of subsequent radiologist-recommended US examinations, 70.0% (63/90) yielded incremental diagnostic utility vs. 19.2% (44/229) ordered independently by treating physicians (OR 3.65; 95% CI 2.31–5.75). For those encounters in which US provided incremental diagnostic utility, the most commonly assessed anatomical areas were the biliary system and the female adnexal region.
Conclusion
In ED patients with non-traumatic abdominal and/or pelvic pain undergoing abdominal and pelvic CT, follow-up US examinations recommended by radiologists are more likely to provide incremental diagnostic utility than those independently ordered by their treating physicians. In order to optimize the value of advanced imaging, radiologists should assume greater roles in team-based utilization management.


Similar content being viewed by others
References
Rosenkrantz AB, Ayoola A, Duszak R Jr (2017) Abdominal imaging ordering patterns by referring provider specialty. Abdom Radiol 42(9):2363–2368
Rosenkrantz AB, Hanna TN, Babb JS, Duszak R Jr (2017) Changes in emergency department imaging: perspectives from national patient surveys over two decades. J Am Coll Radiol 14(10):1282–1290
Pinto A, Reginelli A, Cagini L, et al. (2013) Accuracy of ultrasonography in the diagnosis of acute calculous cholecystitis: review of the literature. Crit Ultrasound J 5:S11
Anderson SW, Lucey BC, Varghese JC, Soto JA (2006) Accuracy of MDCT in the diagnosis of choledocholithiasis. AJR 187:174–180
Harris RD, Javitt MC, Brown DL, et al. (2013) ACR appropriateness criteria: clinically suspected adnexal mass. Ultrasound Q 29:79–86
Pinto Leite N, Pereira JM, Cunha R, Pinto P, Sirlin C (2005) CT evaluation of appendicitis and its complications: imaging techniques and key diagnostic findings. AJR Am J Roentgenol 185:406–417
Paulson EK, Thompson WM (2015) Review of small-bowel obstruction: the diagnosis and when to worry. Radiology 275(2):332–342
Cho KC, Morehouse HT, Alterman DD, Thornhill BA (1990) Sigmoid diverticulitis: diagnostic role of CT—comparison with barium enema studies. Radiology 176(1):111–115
Laméris W, van Randen A, van Es HW, et al. (2009) Imaging strategies for detection of urgent conditions in patients with acute abdominal pain: diagnostic accuracy study. BMJ 338:b2431
Welch HG, Hayes KJ, Frost C (2012) Repeat testing among medicare beneficiaries. Arch Intern Med 172(22):1745–1751
Ip IK, Mortele KJ, Prevedello LM, Khorasani R (2012) Repeat abdominal imaging examinations in a tertiary care hospital. Am J Med 125:155–161
Duszak R Jr, Berlin JW (2012) Utilization management in radiology, part 1: rationale, history, and current status. J Am Coll Radiol 9:694–699
Duszak R Jr, Berlin JW (2012) Utilization management in radiology, part 2: perspectives and future directions. J Am Coll Radiol 9:700–703
Levin DC, Rao VM (2004) Turf wars in radiology: other causes of overutilization and what can be done about it. J Am Coll Radiol 1:317–321
Levine D, et al. (2010) Management of asymptomatic ovarian and other adnexal cysts imaged at US: Society of Radiologists in Ultrasound consensus conference statement. Radiology 256(3):943–954
Riddell AM, Khalili K (2006) Assessment of acute abdominal pain: utility of a second cross-sectional imaging examination. Radiology 238:570–577
Yitta S, Mausner EV, Kim A, et al. (2011) Pelvic ultrasound immediately following MDCT in female patients with abdominal/pelvic pain: is it always necessary? Emerg Radiol 18:371
Patel MD, Dubinsky TJ (2007) Reimaging the female pelvis with ultrasound after CT: general principles. Ultrasound Q 23(3):177–187
Rao VM, Levin DC (2012) The overuse of diagnostic imaging and the choosing wisely initiative. Ann Intern Med 157:574–576
Hillman BJ, Joseph CA, Mabry MR, et al. (1990) Frequency and costs of diagnostic imaging in office practice—a comparison of self-referring and radiologist-referring physicians. N Engl J Med 323:1604–1608
Radecki SE, Steele JP (1990) Effect of on-site facilities on use of diagnostic radiology by non-radiologists. Invest Radiol 25:190–193
Allen B Jr, Carrol LV, Hughes DR, et al. (2017) Downstream imaging utilization after emergency department ultrasound interpreted by radiologists versus nonradiologists: a medicare claims-based study. J Am Coll Radiol 14:475–481
Durand DJ, McGinty G, Duszak R (2015) From gatekeeper to steward: the evolving concept of radiologist accountability for imaging utilization. J Am Coll Radiol 12:1446–1448
American College of Radiology (2017) ACR Appropriateness Criteria®. https://acsearch.acr.org/list. Accessed Sept 2017.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Li, D., Patlas, M., Mclean, K. et al. Relative diagnostic utility of radiologist-recommended abdominal ultrasound following emergency department abdominal and pelvic computed tomography. Abdom Radiol 43, 3176–3183 (2018). https://doi.org/10.1007/s00261-018-1576-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-018-1576-2