Abstract
Purpose
To compare diagnostic performance for prediction of malignant potential in IPMNs between EUS, contrast-enhanced CT and MRI.
Materials and methods
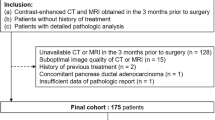
76 patients with IPMN (benign = 37, malignant = 39) underwent EUS, contrast-enhanced CT, and MRI. EUS was analyzed based on formal reports and contrast-enhanced CT and MRI were retrospectively analyzed by two radiologists according to the consensus guidelines 2012. Diagnostic performance and imaging features of malignant IPMNs were analyzed using ROC analysis and multivariate analyses.
Results
Diagnostic performance of contrast-enhanced CT (AUC = 0.792 in R1, 0.830 in R2), MRI (AUC = 0.742 in R1, 0.776 in R2), and EUS (AUC = 0.733) for predicting malignant IPMNs were comparable without significant difference (p > 0.05). In multivariable analysis, enhancing solid component in contrast-enhanced CT and MRI and mural nodule in EUS (OR 1.8 in CT, 1.36 in MRI, 1.47 in EUS), MPD diameter ≥ 10 mm (OR 1.3 in CT, 1.4 in MRI, 1.66 in EUS), MPD diameter of 5–9 mm (OR 1.23 in CT, 1.31 in MRI), and thickened septa or wall (OR 1.3 in CT and MRI) were significant variables (p < 0.05). Interobserver agreement of thickened cyst septa or wall (k = 0.579–0.617) and abrupt caliber change of MPD (k = 0.689–0.788) was lower than other variables (k > 0.80).
Conclusion
Diagnostic performance of contrast-enhanced CT, MRI, and EUS for predicting malignant IPMNs was comparable with each modalities without significant difference.




Similar content being viewed by others
Abbreviations
- IPMN:
-
Intraductal papillary mucinous neoplasm
- MPD:
-
Main pancreatic duct
- MRI:
-
Magnetic resonance imaging
- MRCP:
-
Magnetic resonance cholangiopancreatography
- CT:
-
Computed tomography
- EUS:
-
Endoscopic ultrasound
References
Lee KS, Sekhar A, Rofsky NM, Pedrosa I (2010) Prevalence of incidental pancreatic cysts in the adult population on MR imaging. Am J Gastroenterol 105(9):2079–2084. doi:10.1038/ajg.2010.122
Zhang XM, Mitchell DG, Dohke M, et al. (2002) Pancreatic cysts: depiction on single-shot fast spin-echo MR images. Radiology 223(2):547–553. doi:10.1148/radiol.2232010815
Kent TS Jr, Vollmer CM, Callery MP (2010) Intraductal papillary mucinous neoplasm and the pancreatic incidentaloma. World J Gastrointest Surg 2(10):319–323. doi:10.4240/wjgs.v2.i10.319
Bosman FT, Carneiro F, Hruban RH, Theise ND (2010) WHO classification of tumours of the digestive system, vol. 4. Geneva: World Health Organization
Ogawa H, Itoh S, Ikeda M, et al. (2008) Intraductal papillary mucinous neoplasm of the pancreas: assessment of the likelihood of invasiveness with multisection CT. Radiology 248(3):876–886. doi:10.1148/radiol.2482071578
Manfredi R, Graziani R, Motton M, et al. (2009) Main pancreatic duct intraductal papillary mucinous neoplasms: accuracy of MR imaging in differentiation between benign and malignant tumors compared with histopathologic analysis. Radiology 253(1):106–115. doi:10.1148/radiol.2531080604
Nakajima Y, Yamada T, Sho M (2010) Malignant potential of intraductal papillary mucinous neoplasms of the pancreas. Surg Today 40(9):816–824. doi:10.1007/s00595-009-4227-y
Do RK, Katz SS, Gollub MJ, et al. (2014) Interobserver agreement for detection of malignant features of intraductal papillary mucinous neoplasms of the pancreas on MDCT. AJR Am J Roentgenol 203(5):973–979. doi:10.2214/AJR.13.11490
Tanaka M, Chari S, Adsay V, et al. (2006) International consensus guidelines for management of intraductal papillary mucinous neoplasms and mucinous cystic neoplasms of the pancreas. Pancreatology 6(1–2):17–32. doi:10.1159/000090023
Tanaka M, Fernandez-del Castillo C, Adsay V, et al. (2012) International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology 12(3):183–197. doi:10.1016/j.pan.2012.04.004
Kim SH, Lee JM, Lee ES, et al. (2015) Intraductal papillary mucinous neoplasms of the pancreas: evaluation of malignant potential and surgical resectability by using MR imaging with mr cholangiography. Radiology 274(3):723–733. doi:10.1148/radiol.14132960
Kim KW, Park SH, Pyo J, et al. (2014) Imaging features to distinguish malignant and benign branch-duct type intraductal papillary mucinous neoplasms of the pancreas: a meta-analysis. Ann Surg 259(1):72–81. doi:10.1097/SLA.0b013e31829385f7
Kamata K, Kitano M, Kudo M, et al. (2014) Value of EUS in early detection of pancreatic ductal adenocarcinomas in patients with intraductal papillary mucinous neoplasms. Endoscopy 46(1):22–29. doi:10.1055/s-0033-1353603
Koito K, Namieno T, Nagakawa T, et al. (1997) Solitary cystic tumor of the pancreas: EUS-pathologic correlation. Gastrointest Endosc 45(3):268–276
Ahmad NA, Kochman ML, Lewis JD, Ginsberg GG (2001) Can EUS alone differentiate between malignant and benign cystic lesions of the pancreas&quest. Am J Gastroenterol 96(12):3295–3300
Kubo H, Nakamura K, Itaba S, et al. (2009) Differential diagnosis of cystic tumors of the pancreas by endoscopic ultrasonography. Endoscopy 41(8):684–689. doi:10.1055/s-0029-1214952
Ohno E, Hirooka Y, Itoh A, et al. (2009) Intraductal papillary mucinous neoplasms of the pancreas: differentiation of malignant and benign tumors by endoscopic ultrasound findings of mural nodules. Ann Surg 249(4):628–634. doi:10.1097/SLA.0b013e3181a189a8
Tanaka M (2011) Controversies in the management of pancreatic IPMN. Nat Rev Gastroenterol Hepatol 8(1):56–60. doi:10.1038/nrgastro.2010.193
Seo N, Byun JH, Kim JH, et al. (2015) Validation of the 2012 international consensus guidelines using computed tomography and magnetic resonance imaging: branch duct and main duct intraductal papillary mucinous neoplasms of the pancreas. Ann Surg . doi:10.1097/SLA.0000000000001217
Kim JH, Eun HW, Kim KW, et al. (2013) Intraductal papillary mucinous neoplasms with associated invasive carcinoma of the pancreas: imaging findings and diagnostic performance of MDCT for prediction of prognostic factors. AJR Am J Roentgenol 201(3):565–572. doi:10.2214/AJR.12.9511
Schmidt CM, White PB, Waters JA, et al. (2007) Intraductal papillary mucinous neoplasms: predictors of malignant and invasive pathology. Ann Surg 246(4):644–651 (discussion 651–644). doi:10.1097/SLA.0b013e318155a9e5
Aso T, Ohtsuka T, Matsunaga T, et al. (2014) “High-risk stigmata” of the 2012 international consensus guidelines correlate with the malignant grade of branch duct intraductal papillary mucinous neoplasms of the pancreas. Pancreas 43(8):1239–1243. doi:10.1097/MPA.0000000000000199
Jang JY, Park T, Lee S, et al. (2014) Validation of international consensus guidelines for the resection of branch duct-type intraductal papillary mucinous neoplasms. Br J Surg 101(6):686–692. doi:10.1002/bjs.9491
Yamashita Y, Ueda K, Itonaga M, et al. (2013) Usefulness of contrast-enhanced endoscopic sonography for discriminating mural nodules from mucous clots in intraductal papillary mucinous neoplasms: a single-center prospective study. J Ultrasound Med 32(1):61–68
Palmucci S, Trombatore C, Foti PV, et al. (2014) The utilization of imaging features in the management of intraductal papillary mucinous neoplasms. Gastroenterol Res Pract 2014:765451. doi:10.1155/2014/765451
Efthymiou A, Podas T, Zacharakis E (2014) Endoscopic ultrasound in the diagnosis of pancreatic intraductal papillary mucinous neoplasms. World J Gastroenterol 20(24):7785–7793. doi:10.3748/wjg.v20.i24.7785
Barron M, Roch A, Waters J, et al. (2014) Does preoperative cross-sectional imaging accurately predict main duct involvement in intraductal papillary mucinous neoplasm? J Gastrointest Surg 18(3):447–456
Sugiyama M, Izumisato Y, Abe N, et al. (2003) Predictive factors for malignancy in intraductal papillary-mucinous tumours of the pancreas. Br J Surg 90(10):1244–1249. doi:10.1002/bjs.4265
Nagai K, Doi R, Ito T, et al. (2009) Single-institution validation of the international consensus guidelines for treatment of branch duct intraductal papillary mucinous neoplasms of the pancreas. J Hepatobiliary Pancreat Surg 16(3):353–358. doi:10.1007/s00534-009-0068-8
Augustin T, Vandermeer TJ (2010) Intraductal papillary mucinous neoplasm: a clinicopathologic review. Surg Clin N Am 90(2):377–398. doi:10.1016/j.suc.2009.12.008
Goh BK, Thng CH, Tan DM, et al. (2014) Evaluation of the Sendai and 2012 International Consensus Guidelines based on cross-sectional imaging findings performed for the initial triage of mucinous cystic lesions of the pancreas: a single institution experience with 114 surgically treated patients. Am J Surg 208(2):202–209. doi:10.1016/j.amjsurg.2013.09.031
Acknowledgements
We would like to thank Bonnie Hami, MA (USA) for her editorial assistance in the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this study.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Our institutional review board approved this retrospective study and waived the requirement for informed consent. For this type of study, formal consent is not required.
Informed consent
Statement of informed consent was not applicable since the manuscript does not contain any patient data.
Rights and permissions
About this article
Cite this article
Choi, SY., Kim, J.H., Yu, M.H. et al. Diagnostic performance and imaging features for predicting the malignant potential of intraductal papillary mucinous neoplasm of the pancreas: a comparison of EUS, contrast-enhanced CT and MRI. Abdom Radiol 42, 1449–1458 (2017). https://doi.org/10.1007/s00261-017-1053-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-017-1053-3