Abstract
Objectives
To determine to what extent low-energy CT imaging affects attenuation of gastrointestinal tract (GIT) opacified with positive oral contrast media (OCM). Second, to establish optimal OCM concentrations for low-energy diagnostic CT exams.
Methods
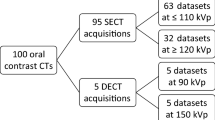
One hundred patients (38 men and 62 women; age 62 ± 11 years; BMI 26 ± 5) with positive OCM-enhanced 120-kVp single-energy CT (SECT), and follow-up 100-kVp acquisitions (group A; n = 50), or 40–70-keV reconstructions from rapid kV switching-single-source dual-energy CT (ssDECT) (group B; n = 50) were included. Luminal attenuation from different GIT segments was compared between exams. Standard dose of three OCM and diluted solutions (75%, 50%, and 25% concentrations) were introduced serially in a gastrointestinal phantom and scanned using SECT (120, 100, and 80 kVp) and DECT (80/140 kVp) acquisitions on a ssDECT scanner. Luminal attenuation was obtained on SECT and DECT images (40–70 keV), and compared to 120-kVp scans with standard OCM concentrations.
Results
Luminal attenuation was higher on 100-kVp (328 HU) and on 40–60-keV images (410–924 HU) in comparison to 120-kVp scans (298 HU) in groups A and B (p < 0.05). Phantom: There was an inverse correlation between luminal attenuation and X-ray energy, increasing up to 527 HU on low-kVp and 999 HU on low-keV images (p < 0.05). 25% and 50% diluted OCM solutions provided similar or higher attenuation than 120 kVp, at low kVp and keV, respectively.
Conclusions
Low-energy CT imaging increases the attenuation of GIT opacified with positive OCM, permitting reduction of 25%–75% OCM concentration.




Similar content being viewed by others
References
Garrett PR, Meshkov SL, Perlmutter GS (1984) Oral contrast agents in CT of the abdomen. Radiology 153(2):545–546
Ruijs SH (1979) A simple procedure for patient preparation in abdominal CT. AJR Am J Roentgenol 133(3):551–552
O’Malley ME, et al. (2000) Helical CT protocols for the abdomen and pelvis: a survey. AJR Am J Roentgenol 175(1):109–113
Megibow AJ, Bosniak MA (1980) Dilute barium as a contrast agent for abdominal CT. AJR Am J Roentgenol 134(6):1273–1274
Pickhardt PJ, et al. (2003) Computed tomographic virtual colonoscopy to screen for colorectal neoplasia in asymptomatic adults. N Engl J Med 349(23):2191–2200
Lee CH, et al. (2013) Use of positive oral contrast agents in abdominopelvic computed tomography for blunt abdominal injury: meta-analysis and systematic review. Eur Radiol 23(9):2513–2521
Buttigieg EL, et al. (2014) An evaluation of the use of oral contrast media in abdominopelvic CT. Eur Radiol 24(11):2936–2944
Kammerer S, et al. (2015) Abdominal and pelvic CT: is positive enteric contrast still necessary? Results of a retrospective observational study. Eur Radiol 25(3):669–678
Berther R, et al. (2008) Comparison of neutral oral contrast versus positive oral contrast medium in abdominal multidetector CT. Eur Radiol 18(9):1902–1909
Therasse P, et al. (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92(3):205–216
Kim YE, et al. (2010) Clinical implication of positive oral contrast computed tomography for the evaluation of postoperative leakage after gastrectomy for gastric cancer. J Comput Assist Tomogr 34(4):537–542
Nakayama Y, et al. (2005) Abdominal CT with low tube voltage: preliminary observations about radiation dose, contrast enhancement, image quality, and noise. Radiology 237(3):945–951
Horton KM, Fishman EK, Gayler B (2008) The use of iohexol as oral contrast for computed tomography of the abdomen and pelvis. J Comput Assist Tomogr 32(2):207–209
Lonnemark M, Magnusson A (1995) Oral contrast media in CT of the abdomen. Iohexol of different concentrations as a gastrointestinal contrast medium. Acta Radiol 36(4):396–398
Fuentes-Orrego JM, et al. (2013) Dose-modified 256-MDCT of the abdomen using low tube current and hybrid iterative reconstruction. Acad Radiol 20(11):1405–1412
Nakaura T, et al. (2014) Low-dose abdominal CT protocols with a tube voltage setting of 100 kVp or 80 kVp: performance of radiation dose reduction and influence on visual contrast. Clin Radiol 69(8):804–811
Kanematsu M, et al. (2014) Whole-body CT angiography with low tube voltage and low-concentration contrast material to reduce radiation dose and iodine load. AJR Am J Roentgenol 202(1):W106–W116
Kanematsu M, et al. (2015) Low-iodine-load and low-tube-voltage CT angiographic imaging of the kidney by using bolus tracking with saline flushing. Radiology 275(3):832–840
Marin D, et al. (2009) Hypervascular liver tumors: low tube voltage, high tube current multidetector CT during late hepatic arterial phase for detection–initial clinical experience. Radiology 251(3):771–779
Agrawal MD, et al. (2014) Oncologic applications of dual-energy CT in the abdomen. Radiographics 34(3):589–612
Mileto A, et al. (2014) Dual-energy MDCT in hypervascular liver tumors: effect of body size on selection of the optimal monochromatic energy level. AJR Am J Roentgenol 203(6):1257–1264
McNamara MM, et al. (2015) Multireader evaluation of lesion conspicuity in small pancreatic adenocarcinomas: complimentary value of iodine material density and low keV simulated monoenergetic images using multiphasic rapid kVp-switching dual energy CT. Abdom Imaging 40(5):1230–1240
Horton KM, Eng J, Fishman EK (2000) Normal enhancement of the small bowel: evaluation with spiral CT. J Comput Assist Tomogr 24(1):67–71
Hamlin DJ, Burgener FA (1981) Positive and negative contrast agents in CT evaluation of the abdomen and pelvis. J Comput Tomogr 5(2):82–90
Keyzer C, et al. (2009) MDCT for suspected acute appendicitis in adults: impact of oral and IV contrast media at standard-dose and simulated low-dose techniques. AJR Am J Roentgenol 193(5):1272–1281
Wang ZJ, et al. (2011) Positive enteric contrast material for abdominal and pelvic CT with automatic exposure control: what is the effect on patient radiation exposure? Eur J Radiol 79(2):e58–e62
Patino M, et al. (2015) A quantitative comparison of noise reduction across five commercial (hybrid and model-based) iterative reconstruction techniques: an anthropomorphic phantom study. AJR Am J Roentgenol 204(2):W176–W183
Nyman, U., G. Dinnetz, and I. Andersson, E-Z-CAT. An oral contrast medium for use in computed tomography of the abdomen. Acta Radiol Diagn, 1984. 25(2): p. 121–124.
Hwang I, et al. (2015) Low tube voltage computed tomography urography using low-concentration contrast media: comparison of image quality in conventional computed tomography urography. Eur J Radiol 84(12):2454–2463
Harieaswar S, et al. (2009) Routine use of positive oral contrast material is not required for oncology patients undergoing follow-up multidetector CT. Radiology 250(1):246–253
Quagliano PV, Austin RF Jr (1997) Oral contrast agents for CT: a taste test survey. J Comput Assist Tomogr 21(5):720–722
Hara AK, et al. (2013) Reducing body CT radiation dose: beyond just changing the numbers. AJR Am J Roentgenol 201(1):33–40
McNamara MM, et al. (2010) Oral contrast media for body CT: comparison of diatrizoate sodium and iohexol for patient acceptance and bowel opacification. AJR Am J Roentgenol 195(5):1137–1141
Megibow AJ, et al. (2006) Evaluation of bowel distention and bowel wall appearance by using neutral oral contrast agent for multi-detector row CT. Radiology 238(1):87–95
Mongan J, et al. (2012) In vivo differentiation of complementary contrast media at dual-energy CT. Radiology 265(1):267–272
Cai W, et al. (2015) Electronic cleansing in fecal-tagging dual-energy CT colonography based on material decomposition and virtual colon tagging. IEEE Trans Biomed Eng 62(2):754–765
Birnbaum BA, et al. (2007) Multi-detector row CT attenuation measurements: assessment of intra- and interscanner variability with an anthropomorphic body CT phantom. Radiology 242(1):109–119
Grant KL, et al. (2014) Assessment of an advanced image-based technique to calculate virtual monoenergetic computed tomographic images from a dual-energy examination to improve contrast-to-noise ratio in examinations using iodinated contrast media. Invest Radiol 49(9):586–592
Husarik DB, et al. (2015) Advanced virtual monoenergetic computed tomography of hyperattenuating and hypoattenuating liver lesions: ex-vivo and patient experience in various body sizes. Invest Radiol 50(10):695–702
Acknowledgements
The authors are extremely grateful and sincerely acknowledge the involvement of Jerry Jones, Luis Colon, Vyoma Sahani, Srishti Lulla, Olivia Long, and Maxeem Abedi-Tari during the CT scanning of the anthropomorphic phantom and data analysis. We also acknowledge Dr. Rodrigo Canellas M.D for his collaboration with the statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this study.
Conflict of interest
Dushyant V. Sahani has received research grants from General Electric Healthcare. The other authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors. Institutional Review Board approval was obtained for this study.
Informed consent
Statement of informed consent was not applicable since the manuscript does not contain any patient data.
Rights and permissions
About this article
Cite this article
Patino, M., Murcia, D.J., Iamurri, A.P. et al. Impact of low-energy CT imaging on selection of positive oral contrast media concentration. Abdom Radiol 42, 1298–1309 (2017). https://doi.org/10.1007/s00261-016-0993-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-016-0993-3