Abstract
Purpose
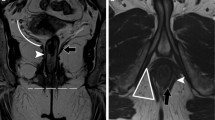
The purpose of this study was to evaluate the diagnostic efficacies of CT fistulography and MRI, in the diagnostic work-up of perianal fistula patients.
Materials and methods
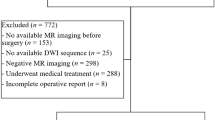
All 41 patients who were included in the study (36 males and 5 females, with an average age of 41 years) underwent CT fistulography and MRI examinations prior to surgery. The fistula characteristics obtained from these examinations were compared with the surgical findings. The comparative results were evaluated by means of the Kappa analysis method.
Results
CT fistulography predicted the correct perianal fistula classification in 30 (73.1%) of the 41 patients, whereas MRI correctly defined fistula classification in 38 (92.7%) of these patients (the K values were 0.621 and 0.896, respectively; with p < 0.001). CT fistulography depicted 29 secondary extensions in 16 patients, whereas MR imaging revealed 28 secondary extensions in 15 patients. A substantial agreement was found between surgical findings and two modalities (K value was 0.789 and 0.793 for CT fistulography and MRI, respectively, with a p value < 0.001). In terms of locations of internal openings, CT fistulography was able to detect the locations in 28 patients (68.2%), whereas MRI was more successful in this aspect, with a number of 35 patients (85.3%). Granulation tissues, inflammation and edema around the fistula, abscesses, and fistular wall fibrosis were also evaluated.
Conclusion
CT fistulography and MRI have different advantages in the diagnosis of perianal fistulas. A good command of knowledge concerning the issue may be a key factor in modality decision.








Similar content being viewed by others
References
Halligan S, Stoker J (2006) Imaging of fistula in ano. Radiology 239:18–33
Rickard MJ (2005) Anal abscesses and fistulas. ANZ J Surg 75:64–72
Kumar N, Agarwal Y, Chawla AS, Jain R, Thukral BB (2015) MRI Perianal Fistulae . doi:10.1016/j.crad.2015.09.001
Ziech M, Felt-Bersma R, Stoker J (2009) Imaging of perianal fistulas. Clin Gastroenterol Hepatol 7:1037–1045
Chowbey PK, Khullar R, Sharma A, et al. (2015) Minimally invasive anal fistula treatment (MAFT)—an appraisal of early results in 416 patients. Indian J Surg 77:716–721
Morren GL, Beets-Tan RGH, van Engelshoven JMA (2001) Anatomy of the anal canal and perianal structures as defined by phased-array magnetic resonance imaging. Br J Surg 88:1506–1512
Liang C, Jiang W, Zhao B, et al. (2013) CT imaging with fistulography for perianal fistula: does it really help the surgeon? Clin Imaging 37:1069–1076. doi:10.1016/j.clinimag.2013.04.014
Sahni VA, Ahmad R, Burling D (2008) Which method is best for imaging of perianal fistula? Abdom Imaging 33:26–30
Liang C, Lu Y, Zhao B, et al. (2014) Imaging of anal fistulas: comparison of computed tomographic fistulography and magnetic resonance imaging. Korean J Radiol 15:712–723. doi:10.3348/kjr.2014.15.6.712
Beets-Tan RGH, Beets GL, van der Hoop AG, et al. (2001) Preoperative MR imaging of anal fistulas: does it really help the surgeon? Radiology 218:75–84
Gourtsoyianni S, Goh V (2014) MRI of anal cancer: assessing response to definitive chemoradiotherapy. Abdom Imaging 39:2–17. doi:10.1007/s00261-013-0032-6
Sudoł-Szopińska I, Kucharczyk A, Kołodziejczak M, et al. (2014) Endosonography and magnetic resonance imaging in the diagnosis of high anal fistulae—a comparison. J Ultrason 14:142–151
Felt-Bersma RJ (2006) Endoanal ultrasound in perianal fistulas and abscesses. Dig Liver Dis 38:537–543
Khati NJ, Lewis NS, Fraizer AA, et al. (2015) CT of acute perianal abscesses and infected fistulae: a pictorial essay. Emerg Radiol 22:329–335. doi:10.1007/s10140-014-1284-3
Barral M, Boudiaf M, Dohan A, et al. (2015) MDCT of acute colitis in adults: an update in current imaging features. Diagn İnterv Imaging 96:133–149. doi:10.1016/j.diii.2014.04.008
Lee MH, Moon MH, Sung CK, Woo H, Oh S (2014) CT findings of acute pelvic inflammatory disease. Abdom Imaging 39:1350–1355. doi:10.1007/s00261-014-0158-1
Mendoza LR, Borobia AR, Gonzalez CZ, Pena T, Ros PR (2004) MR imaging in anal fistulae. Rev Argent Radiol 68:237–244
Bartram C, Buchanan G (2003) Imaging anal fistula. Radiol Clin N Am 41:443–457
Tonolini M, Campari A, Bianco R (2011) Ileal pouch and related complications: spectrum of imaging findings with emphasis on MRI. Abdom Imaging 36:698–706
O’Malley RB, Al-Hawary MM, Kaza RK, et al. (2012) Rectal imaging: part 2, perianal fistula evaluation on pelvic MRI–what the radiologist needs to know. Am J Roentgenol 199:W43–W53
de Miguel Criado J, del Salto LG, Rivas PF, et al. (2012) MR imaging evaluation of perianal fistulas: spectrum of imaging features. Radiographics 32:175–194. doi:10.1148/rg.321115040
Morris J, Spencer JA, Ambrose NS (2000) MR imaging classification of perianal fistulas and its implications for patient management. Radiographics 20:623–635
Landis JR, Koch GG (1977) An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers. Biometrics 33:363–374
Buchanan G, Halligan S, Williams A, et al. (2002) Effect of MRI on clinical outcome of recurrent fistula-in-ano. Lancet 360:1661–1662
Buchanan GN, Halligan S, Williams AB, et al. (2003) Magnetic resonance imaging for primary fistula in ano. Br J Surg 90:877–881
Buchanan GN, Halligan S, Bartram CI, et al. (2004) Clinical examination, endosonography, and MR imaging in preoperative assessment of fistula in ano: comparison with outcome-based reference standard. Radiology 233:674–681
Gage KL, Deshmukh S, Macura KJ, Kamel IR, Zaheer A (2013) MRI of perianal fistulas: bridging the radiological-surgical divide. Abdom Imaging 38:1033–1042. doi:10.1007/s00261-012-9965-4
Spencer JA, Chapple K, Wilson D, et al. (1998) Outcome after surgery for perianal fistula: predictive value of MR imaging. Am J Roentgenol 171:403–406
Chapple KS, Spencer JA, Windsor AC, et al. (2000) Prognostic value of magnetic resonance imaging in the management of fistula-in-ano. Dis Colon Rectum 43:511–516
Holzer B, Rosen HR, Urban M, et al. (2000) Magnetic resonance imaging of perianal fistulas: predictive value for Parks classification and identification of the inner opening. Colorectal Dis 2:340–345
Beckingham IJ, Spencer JA, Ward J, et al. (1996) Prospective evaluation of dynamic contrast enhanced magnetic resonance imaging in the evaluation of fistula in ano. Br J Surg 83:1396–1398
Singh K, Singh N, Thukral C, Singh KP, Bhalla V (2014) Magnetic resonance imaging (MRI) evaluation of perianal fistulae with surgical correlation. J Clin Diagn Res 8:1–4
Halligan S, Healy JC, Bartram CI (1998) Magnetic resonance imaging of fistula-in-ano: STIR or SPIR? Br J Radiol 71:141–145
Sabir N, Sungurtekin U, Erdem E, Nessar M (2000) Magnetic resonance imaging with rectal Gd-DTPA: new tool for the diagnosis of perianal fistula. Int J Colorectal Dis 15:317–322
Hori M, Oto A, Orrin S, Suzuki K, Baron RL (2009) Diffusion-weighted MRI: a new tool for the diagnosis of fistula in ano. J Magn Reson Imaging 30:1021–1026
Yildirim N, Gökalp G, Öztürk E, et al. (2012) Ideal combination of MRI sequences for perianal fistula classification and the evaluation of additional findings for readers with varying levels of experience. Diagn Interv Radiol 18:11–19
Kinner S, Blex S, Maderwald S, et al. (2014) Addition of diffusion-weighted imaging can improve diagnostic confidence in bowel MRI. Clin Radiol 69:372–377
Burdan F, Sudol-Szopinska I, Staroslawska E, et al. (2015) Magnetic resonance imaging and endorectal ultrasound for diagnosis of rectal lesions. Eur J Med Res 20:4. doi:10.1186/s40001-014-0078-0
Mahjoubi B, Haizadch Kharazi H, Mirzaei R, Moghimi A, Changizi A (2006) Diagnostic accuracy of body coil MRI in describing the characteristics of perianal fistulas. Colorectal Dis 8:202–207
deSouza NM, Gilderdale DJ, Coutts GA, Puni R, Steiner RE (1998) MRI of fistula-in-ano: a comparison of endoanal coil with external phased array coil techniques. J Comput Assist Tomogr 22:357–363
Stoker J, Hussain SM, van Kempen D, Elevelt AJ, Laméris JS (1996) Endoanal coil in MR imaging of anal fistulas. Am J Roentgenol 166:360–362
deSouza NM, Gilderdale DJ, MacIver DK, Ward HC (1997) High-resolution MR imaging of the anal sphincter in children: a pilot study using endoanal receiver coils. Am J Roentgenol 169:201–206
Stoker J, Rociu E, Schouten WR, Laméris JS (2002) Anovaginal and rectovaginal fistulas: endoluminal sonography versus endoluminal MR imaging. Am J Roentgenol 178:737–741
Robertson WG, Mangione JS (1998) Cutaneous advancement flap closure: alternative method for treatment of complicated anal fistulas. Dis Colon Rectum 41:886–887
Tang CL, Chew SP, Seow-Choen F (1996) Prospective randomized trial of drainage alone vs. drainage and fistulotomy for acute perianal abscesses with proven internal opening. Dis Colon Rectum 39:1415–1417
Li X, Qiang JW, He C, Ji XS, Zhang B (2011) Magnetic resonance imaging study of perianal abscess. Zhonghua Wei Chang Wai Ke Za Zhi 14:868–870
Maruyama R, Noguchi T, Takano M, et al. (2000) Usefulness of magnetic resonance imaging for diagnosing deep anorectal abscesses. Dis Colon Rectum 43:2–5
Caliste X, Nazir S, Goode T, et al. (2011) Sensitivity of computed tomography in detection of perirectal abscess. Am Surg 77:166–168
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Soker, G., Gulek, B., Yilmaz, C. et al. The comparison of CT fistulography and MR imaging of perianal fistulae with surgical findings: a case–control study. Abdom Radiol 41, 1474–1483 (2016). https://doi.org/10.1007/s00261-016-0722-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-016-0722-y