Abstract
Purpose
To determine whether a navigator-gated three-dimensional T1-weighted gradient-echo sequence (T1W-GRE, navigated LAVA) can improve diagnostic performance for the detection of focal liver lesions (FLLs) compared to standard breath-hold (BH) T1W-GRE breath-hold LAVA (BH-LAVA) during the hepatobiliary phase (HBP) of gadoxetic acid liver magnetic resonance imaging (MRI) in patients with limited breath-holding capacity.
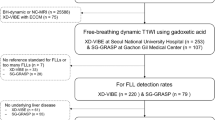
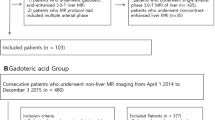
Materials and methods
This retrospective study was approved by our institutional review board and the requirement for informed consent was waived. We included 372 patients who underwent liver MRI including both navigated LAVA and BH-LAVA sequences. Overall image quality of the two HBP image sets was compared. In patients with limited breath-holding capacity, diagnostic performances in detecting FLLs on the two HBP images were compared using jackknife-alternative free-response receiver-operating characteristic (JAFROC) analysis by two reviewers.
Results
There were 13 cases (13/372; 3.5%) of image acquisition failure using the navigated LAVA sequence due to severe irregular breathing, and 50 of 359 patients had limited breath-holding capacity. In these patients, overall image quality of navigated LAVA (2.78 ± 0.95) was significantly better than that of BH-LAVA (2.42 ± 0.81, P < 0.005), and both readers showed significantly higher JAFROC figure-of-merit values with navigated LAVA compared to BH-LAVA (0.94 and 0.86 in reviewer 1, respectively; 0.89 and 0.83 in reviewer 2, respectively, P < 0.005). Overall image quality of navigated LAVA was also better than that of BH-LAVA in patients with sufficient breath-holding capacity (n = 309, 3.96 ± 0.88, 3.81 ± 0.66, respectively, P < 0.001).
Conclusion
The navigated LAVA sequence could provide better image quality and diagnostic performance in detecting FLLs than BH-LAVA in patients with limited breath-holding capacity during HBP of gadoxetic acid MRI.





Similar content being viewed by others
References
Ayuso C, Rimola J, García-Criado Á (2012) Imaging of HCC. Abdom Imaging 37:215–230
Mainenti PP, Mancini M, Mainolfi C, et al. (2010) Detection of colo-rectal liver metastases: prospective comparison of contrast enhanced US, multidetector CT, PET/CT, and 1.5 Tesla MR with extracellular and reticulo-endothelial cell specific contrast agents. Abdom Imaging 35:511–521
Gore R, Thakrar K, Wenzke D, et al. (2012) That liver lesion on MDCT in the oncology patient: is it important? Cancer Imaging 12:373–384
Becker-Weidman DJ, Kalb B, Sharma P, et al. (2011) Hepatocellular carcinoma lesion characterization: single-institution clinical performance review of multiphase gadolinium-enhanced MR imaging—comparison to prior same-center results after MR systems improvements. Radiology 261:824–833
Lee JM, Zech CJ, Bolondi L, et al. (2011) Consensus report of the 4th International Forum for gadolinium-ethoxybenzyl-diethylenetriamine pentaacetic acid magnetic resonance imaging. Korean J Radiol 12:403–415
Lee KH, Lee JM, Park JH, et al. (2013) MR imaging in patients with suspected liver metastases: value of liver-specific contrast agent gadoxetic acid. Korean J Radiol 14:894–904
Berger-Kulemann V, Schima W, Baroud S, et al. (2012) Gadoxetic acid-enhanced 3.0 T MR imaging versus multidetector-row CT in the detection of colorectal metastases in fatty liver using intraoperative ultrasound and histopathology as a standard of reference. Eur J Surg Oncol (EJSO) 38:670–676
Martin DR, Semelka RC (2005) Magnetic resonance imaging of the liver: review of techniques and approach to common diseases Seminars in Ultrasound, CT, and MRI. Elsevier, Philadelphia, pp 116–131
Wile GE, Leyendecker JR (2010) Magnetic resonance imaging of the liver: sequence optimization and artifacts. Magn Reson Imaging Clin N Am 18:525–547
Ringe KI, Husarik DB, Gupta RT, Boll DT, Merkle EM (2011) Hepatobiliary transit times of gadoxetate disodium for protocol optimization of comprehensive MR imaging of the biliary system—what is normal? Eur J Radiol 79:201–205
Yu MH, Lee JM, Yoon JH, et al. (2013) Clinical application of controlled aliasing in parallel imaging results in a higher acceleration (CAIPIRINHA)-volumetric interpolated breathhold (VIBE) sequence for gadoxetic acid-enhanced liver MR imaging. J Magn Reson Imaging 38:1020–1026
Yoon JH, Lee JM, Yu MH, et al. (2014) High-resolution T1-weighted gradient echo imaging for liver MRI using parallel imaging at high-acceleration factors. Abdom Imaging 39:711–721
Nagle SK, Busse RF, Brau AC, et al. (2012) High resolution navigated three-dimensional T1-weighted hepatobiliary MRI using gadoxetic acid optimized for 1.5 tesla. J Magn Reson Imaging 36:890–899
Tran PV, Jhaveri KS (2013) Comparison of high spatial resolution respiratory triggered inversion recovery-prepared spoiled gradient echo sequence with standard breathhold T1 sequence MRI of the liver using gadoxetic acid. J Magn Reson Imaging 37:700–706
Young PM, Brau AC, Iwadate Y, et al. (2010) Respiratory navigated free breathing 3D spoiled gradient-recalled echo sequence for contrast-enhanced examination of the liver: diagnostic utility and comparison with free breathing and breath-hold conventional examinations. Am J Roentgenol 195:687–691
Asbach P, Warmuth C, Stemmer A, et al. (2008) High spatial resolution T1-weighted MR imaging of liver and biliary tract during uptake phase of a hepatocyte-specific contrast medium. Invest Radiol 43:809–815
Motosugi U, Ichikawa T, Morisaka H, et al. (2011) Detection of pancreatic carcinoma and liver metastases with gadoxetic acid–enhanced MR imaging: comparison with contrast-enhanced multi-detector row ct. Radiology 260:446–453
Bruix J, Sherman M (2011) Management of hepatocellular carcinoma: an update. Hepatology 53:1020–1022
Ahn SJ, Kim MJ, Hong HS, Kim KA, Song HT (2011) Distinguishing hemangiomas from malignant solid hepatic lesions: a comparison of heavily T2-weighted images obtained before and after administration of gadoxetic acid. J Magn Reson Imaging 34:310–317
Ba-Ssalamah A, Uffmann M, Saini S, et al. (2009) Clinical value of MRI liver-specific contrast agents: a tailored examination for a confident non-invasive diagnosis of focal liver lesions. Eur Radiol 19:342–357
Yun E, Choi B, Han J, et al. (1999) Hepatic hemangioma: contrast-enhancement pattern during the arterial and portal venous phases of spiral CT. Abdom Imaging 24:262–266
Horton KM, Bluemke DA, Hruban RH, Soyer P, Fishman EK (1999) CT and MR imaging of benign hepatic and biliary tumors. Radiographics 19:431–451
Hyodo T, Murakami T, Imai Y, et al. (2013) Hypovascular nodules in patients with chronic liver disease: risk factors for development of hypervascular hepatocellular carcinoma. Radiology 266:480–490
Golfieri R, Grazioli L, Orlando E, et al. (2012) Which is the best MRI marker of malignancy for atypical cirrhotic nodules: hypointensity in hepatobiliary phase alone or combined with other features? Classification after Gd-EOB-DTPA administration. J Magn Reson Imaging 36:648–657
Golfieri R, Renzulli M, Lucidi V, et al. (2011) Contribution of the hepatobiliary phase of Gd-EOB-DTPA-enhanced MRI to dynamic MRI in the detection of hypovascular small (≤2 cm) HCC in cirrhosis. Eur Radiol 21:1233–1242
Kitao A, Matsui O, Yoneda N, et al. (2011) The uptake transporter OATP8 expression decreases during multistep hepatocarcinogenesis: correlation with gadoxetic acid enhanced MR imaging. Eur Radiol 21:2056–2066
Yoon MA, Kim SH, Park HS, et al. (2009) Value of dual contrast liver MRI at 3.0 T in differentiating well-differentiated hepatocellular carcinomas from dysplastic nodules: preliminary results of multivariate analysis. Invest Radiol 44:641–649
Vasanawala SS, Iwadate Y, Church DG, Herfkens RJ, Brau AC (2010) Navigated abdominal T1-W MRI permits free-breathing image acquisition with less motion artifact. Pediatr Radiol 40:340–344
Chakraborty DP (2006) Analysis of location specific observer performance data: validated extensions of the jackknife free-response (JAFROC) method. Acad Radiol 13:1187–1193
Chakraborty DP, Berbaum KS (2004) Observer studies involving detection and localization: modeling, analysis, and validation. Med Phys 31:2313–2330
Zheng B, Chakraborty DP, Rockette HE, Maitz GS, Gur D (2005) A comparison of two data analyses from two observer performance studies using jackknife ROC and JAFROC. Med Phys 32:1031–1034
Sun HY, Lee JM, Shin CI, et al. (2010) Gadoxetic acid-enhanced magnetic resonance imaging for differentiating small hepatocellular carcinomas (≤2 cm in diameter) from arterial enhancing pseudolesions: special emphasis on hepatobiliary phase imaging. Invest Radiol 45:96–103
Knowles B, Welsh FK, Chandrakumaran K, John TG, Rees M (2012) Detailed liver-specific imaging prior to pre-operative chemotherapy for colorectal liver metastases reduces intra-hepatic recurrence and the need for a repeat hepatectomy. HPB 14:298–309
Maniam S, Szklaruk J (2010) Magnetic resonance imaging: review of imaging techniques and overview of liver imaging. World J Radiol 2:309–322
Reiner C, Neville A, Nazeer H, et al. (2013) Contrast-enhanced free-breathing 3D T1-weighted gradient-echo sequence for hepatobiliary MRI in patients with breath-holding difficulties. Eur Radiol 23:3087–3093
Iwadate Y, Brau A, Vasanawala SS, Kabasawa H (2013) Enhancement of respiratory navigator-gated three-dimensional spoiled gradient-recalled echo sequence with variable flip angle scheme. Magn Reson Med 72:172–177
Bashir MR, Merkle EM (2011) Improved liver lesion conspicuity by increasing the flip angle during hepatocyte phase MR imaging. Eur Radiol 21:291–294
Bashir MR, Husarik DB, Ziemlewicz TJ, et al. (2012) Liver MRI in the hepatocyte phase with gadolinium-EOB-DTPA: does increasing the flip angle improve conspicuity and detection rate of hypointense lesions? J Magn Reson Imaging 35:611–616
Acknowledgment
We thank Chris Woo, B.A. (USA), for his editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yoon, J.H., Lee, J.M., Lee, E.S. et al. Navigated three-dimensional T1-weighted gradient-echo sequence for gadoxetic acid liver magnetic resonance imaging in patients with limited breath-holding capacity. Abdom Imaging 40, 278–288 (2015). https://doi.org/10.1007/s00261-014-0214-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-014-0214-x