Abstract
Purpose
Fibroblast-like synoviocytes (FLSs) are key effector cells in the inflamed joints of patients with rheumatoid arthritis (RA). Previous studies have suggested that fibroblast activation protein (FAP) is highly expressed in RA-derived FLSs and is a specific marker of activated RA FLSs. In this study, we developed aluminum-[18F]-labeled 1,4,7-triazacyclononane-N,N′,N″-triacetic acid–conjugated FAP inhibitor 04 ([18F]AlF-NOTA-FAPI-04) to image RA-FLSs in vitro and arthritic joints in collagen-induced arthritis (CIA) mice and RA patients.
Methods
RA FLSs and NIH3T3 cells transfected with FAP were used to perform in vitro–binding studies. Biodistribution was conducted in normal DBA1 mice. Collagen-induced arthritis (CIA) models with different arthritis scores were subjected to [18F]AlF-NOTA-FAPI-04 and 18F-FDG PET imaging. Histological examinations were performed to evaluate FAP expression and Cy3 dye–labeled FAPI-04(Cy3-FAPI-04) uptake. Blocking studies with excess unlabeled FAPI-04 in CIA mice and NIH3T3 xenografts in immunocompromised mice were used to evaluate the binding specificity of [18F]AlF-NOTA-FAPI-04. Additionally, [18F]AlF-NOTA-FAPI-04 PET imaging was performed on two RA patients.
Results
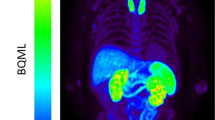
The binding of [18F]AlF-NOTA-FAPI-04 increased significantly in RA FLSs and NIH3T3 cells overexpressing FAP compared to their parental controls (FAP-GFP-NIH3T3 vs. GFP-NIH3T3, 2.40 ± 0.078 vs. 0.297 ± 0.05% AD/105 cells; RA FLSs vs. OA FLSs, 1.54 ± 0.064 vs. 0.343 ± 0.056% AD/105 cells). Compared to 18F-FDG imaging, [18F]AlF-NOTA-FAPI-04 showed high uptake in inflamed joints in the early stage of arthritis, which was positively correlated with the arthritic scores (Pearson r=0.834, P<0.001). In addition, the binding of [18F]AlF-NOTA-FAPI-04 to cells with high FAP expression and the uptake of [18F]AlF-NOTA-FAPI-04 in arthritic joints both could be blocked by excessive unlabeled FAPI-04. Fluorescent staining showed that the intensity of Cy3-FAPI-04 binding to FAP increased accordingly as the expression of FAP protein increased in cells and tissue sections. Furthermore, the uptake of [18F]AlF-NOTA-FAPI-04 in FAP-GFP-NIH3T3 xenografts was significantly higher than that in GFP-NIH3T3 xenograft (35.44 ± 4.27 vs 7.92 ± 1.83% ID/mL). Finally, [18F]AlF-NOTA-FAPI-04 PET/CT imaging in RA patients revealed nonphysiologically high tracer uptake in the synovium of arthritic joints.
Conclusion
[18F]AlF-NOTA-FAPI-04 is a promising radiotracer for imaging RA FLSs and could potentially complement the current noninvasive diagnostic parameters.






Similar content being viewed by others

Data availability
The data sets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
N/A.
References
Wei K, Korsunsky I, Marshall JL, Gao A, Watts GFM, Major T, Croft AP, Watts J, Blazar PE, Lange JK, et al. Notch signalling drives synovial fibroblast identity and arthritis pathology. Nature. 2020;582:259–64. https://doi.org/10.1038/s41586-020-2222-z.
You S, Koh JH, Leng L, Kim WU, Bucala R. The Tumor-Like Phenotype of Rheumatoid Synovium: Molecular Profiling and Prospects for Precision Medicine. Arthritis Rheum. 2018;70:637–52. https://doi.org/10.1002/art.40406.
Orange DE, Agius P, DiCarlo EF, Mirza SZ, Pannellini T, Szymonifka J, Jiang CS, Figgie MP, Frank MO, Robinson WH, et al. Histologic and Transcriptional Evidence of Subclinical Synovial Inflammation in Patients With Rheumatoid Arthritis in Clinical Remission. Arthritis Rheum. 2019;71:1034–41. https://doi.org/10.1002/art.40878.
Nguyen H, Ruyssen-Witrand A, Gandjbakhch F, Constantin A, Foltz V, Cantagrel A. Prevalence of ultrasound-detected residual synovitis and risk of relapse and structural progression in rheumatoid arthritis patients in clinical remission: a systematic review and meta-analysis. Rheumatology (Oxford). 2014;53:2110–8. https://doi.org/10.1093/rheumatology/keu217.
Mathew AJ, Danda D, Conaghan PG. MRI and ultrasound in rheumatoid arthritis. Curr Opin Rheumatol. 2016;28:323–9. https://doi.org/10.1097/bor.0000000000000282.
Nosrati Z, Bergamo M, Rodríguez-Rodríguez C, Saatchi K, Häfeli UO. Refinement and validation of infrared thermal imaging (IRT): a non-invasive technique to measure disease activity in a mouse model of rheumatoid arthritis. Arthritis Res Ther. 2020;22:281. https://doi.org/10.1186/s13075-020-02367-w.
Fitzgerald AA, Weiner LM. The role of fibroblast activation protein in health and malignancy. Cancer Metastasis Rev. 2020;39:783–803. https://doi.org/10.1007/s10555-020-09909-3.
Bauer S, Jendro MC, Wadle A, Kleber S, Stenner F, Dinser R, Reich A, Faccin E, Gödde S, Dinges H, et al. Fibroblast activation protein is expressed by rheumatoid myofibroblast-like synoviocytes. Arthritis Res Ther. 2006;8:R171. https://doi.org/10.1186/ar2080.
Croft AP, Campos J, Jansen K, Turner JD, Marshall J, Attar M, Savary L, Wehmeyer C, Naylor AJ, Kemble S, et al. Distinct fibroblast subsets drive inflammation and damage in arthritis. Nature. 2019;570:246–51. https://doi.org/10.1038/s41586-019-1263-7.
Syed M, Flechsig P, Liermann J, Windisch P, Staudinger F, Akbaba S, Koerber SA, Freudlsperger C, Plinkert PK, Debus J, et al. Fibroblast activation protein inhibitor (FAPI) PET for diagnostics and advanced targeted radiotherapy in head and neck cancers. Eur J Nucl Med Mol Imaging. 2020;47:2836–45. https://doi.org/10.1007/s00259-020-04859-y.
Altmann A, Haberkorn U, Siveke J. The Latest Developments in Imaging of Fibroblast Activation Protein. J Nucl Med. 2021;62:160–7. https://doi.org/10.2967/jnumed.120.244806.
Song G, Feng T, Zhao R, Lu Q, Diao Y, Guo Q, Wang Z, Zhang Y, Ge L, Pan J, et al. CD109 regulates the inflammatory response and is required for the pathogenesis of rheumatoid arthritis. Ann Rheum Dis. 2019;78:1632–41. https://doi.org/10.1136/annrheumdis-2019-215473.
Zhang F, Wei K, Slowikowski K, Fonseka CY, Rao DA, Kelly S, Goodman SM, Tabechian D, Hughes LB, Salomon-Escoto K, et al. Defining inflammatory cell states in rheumatoid arthritis joint synovial tissues by integrating single-cell transcriptomics and mass cytometry. Nat Immunol. 2019;20:928–42. https://doi.org/10.1038/s41590-019-0378-1.
Winer J, Jung CK, Shackel I, Williams PM. Development and validation of real-time quantitative reverse transcriptase-polymerase chain reaction for monitoring gene expression in cardiac myocytes in vitro. Anal Biochem. 1999;270:41–9. https://doi.org/10.1006/abio.1999.4085.
Liao KP, Batra KL, Chibnik L, Schur PH, Costenbader KH. Anti-cyclic citrullinated peptide revised criteria for the classification of rheumatoid arthritis. Ann Rheum Dis. 2008;67:1557–61. https://doi.org/10.1136/ard.2007.082339.
Wagner L, Klemann C, Stephan M, von Hörsten S. Unravelling the immunological roles of dipeptidyl peptidase 4 (DPP4) activity and/or structure homologue (DASH) proteins. Clin Exp Immunol. 2016;184:265–83. https://doi.org/10.1111/cei.12757.
Hamson EJ, Keane FM, Tholen S, Schilling O, Gorrell MD. Understanding fibroblast activation protein (FAP): substrates, activities, expression and targeting for cancer therapy. Proteomics Clin Appl. 2014;8:454–63. https://doi.org/10.1002/prca.201300095.
Laverman P, van der Geest T, Terry SY, Gerrits D, Walgreen B, Helsen MM, Nayak TK, Freimoser-Grundschober A, Waldhauer I, Hosse RJ, et al. Immuno-PET and Immuno-SPECT of Rheumatoid Arthritis with Radiolabeled Anti-Fibroblast Activation Protein Antibody Correlates with Severity of Arthritis. J Nucl Med. 2015;56:778–83. https://doi.org/10.2967/jnumed.114.152959.
van der Geest T, Roeleveld DM, Walgreen B, Helsen MM, Nayak TK, Klein C, Hegen M, Storm G, Metselaar JM, van den Berg WB, et al. Imaging fibroblast activation protein to monitor therapeutic effects of neutralizing interleukin-22 in collagen-induced arthritis. Rheumatology (Oxford). 2018;57:737–47. https://doi.org/10.1093/rheumatology/kex456.
van der Geest T, Laverman P, Gerrits D, Walgreen B, Helsen MM, Klein C, Nayak TK, Storm G, Metselaar JM, Koenders MI, et al. Liposomal Treatment of Experimental Arthritis Can Be Monitored Noninvasively with a Radiolabeled Anti-Fibroblast Activation Protein Antibody. J Nucl Med. 2017;58:151–5. https://doi.org/10.2967/jnumed.116.177931.
Niemeijer AN, Leung D, Huisman MC, Bahce I, Hoekstra OS, van Dongen G, Boellaard R, Du S, Hayes W, Smith R, et al. Whole body PD-1 and PD-L1 positron emission tomography in patients with non-small-cell lung cancer. Nat Commun. 2018;9:4664. https://doi.org/10.1038/s41467-018-07131-y.
Fanti S, Goffin K, Hadaschik BA, Herrmann K, Maurer T, MacLennan S, Oprea-Lager DE, Oyen WJ, Rouvière O, Mottet N, et al. Consensus statements on PSMA PET/CT response assessment criteria in prostate cancer. Eur J Nucl Med Mol Imaging. 2021;48:469–76. https://doi.org/10.1007/s00259-020-04934-4.
Keyaerts M, Xavier C, Heemskerk J, Devoogdt N, Everaert H, Ackaert C, Vanhoeij M, Duhoux FP, Gevaert T, Simon P, et al. Phase I Study of 68Ga-HER2-Nanobody for PET/CT Assessment of HER2 Expression in Breast Carcinoma. J Nucl Med. 2016;57:27–33. https://doi.org/10.2967/jnumed.115.162024.
Sharma P, Singh SS, Gayana S. Fibroblast Activation Protein Inhibitor PET/CT: A Promising Molecular Imaging Tool. Clin Nucl Med. 2021;46:e141–50. https://doi.org/10.1097/rlu.0000000000003489.
Meyer C, Dahlbom M, Lindner T, Vauclin S, Mona C, Slavik R, Czernin J, Haberkorn U, Calais J. Radiation Dosimetry and Biodistribution of (68)Ga-FAPI-46 PET Imaging in Cancer Patients. J Nucl Med. 2020;61:1171–7. https://doi.org/10.2967/jnumed.119.236786.
Kubota K, Yamashita H, Mimori A. Clinical Value of FDG-PET/CT for the Evaluation of Rheumatic Diseases: Rheumatoid Arthritis, Polymyalgia Rheumatica, and Relapsing Polychondritis. Semin Nucl Med. 2017;47:408–24. https://doi.org/10.1053/j.semnuclmed.2017.02.005.
Irmler IM, Opfermann T, Gebhardt P, Gajda M, Bräuer R, Saluz HP, Kamradt T. In vivo molecular imaging of experimental joint inflammation by combined (18)F-FDG positron emission tomography and computed tomography. Arthritis Res Ther. 2010;12:R203. https://doi.org/10.1186/ar3176.
van der Geest T, Metselaar JM, Gerrits D, van Lent PL, Storm G, Laverman P, Boerman OC. [(18)]F FDG PET/CT imaging to monitor the therapeutic effect of liposome-encapsulated prednisolone in experimental rheumatoid arthritis. J Control Release. 2015;209:20–6. https://doi.org/10.1016/j.jconrel.2015.04.019.
Chung SJ, Yoon HJ, Youn H, Kim MJ, Lee YS, Jeong JM, Chung JK, Kang KW, Xie L, Zhang MR, et al. (18)F-FEDAC as a Targeting Agent for Activated Macrophages in DBA/1 Mice with Collagen-Induced Arthritis: Comparison with (18)F-FDG. J Nucl Med. 2018;59:839–45. https://doi.org/10.2967/jnumed.117.200667.
Elzinga EH, van der Laken CJ, Comans EF, Lammertsma AA, Dijkmans BA, Voskuyl AE. 2-Deoxy-2-[F-18]fluoro-D-glucose joint uptake on positron emission tomography images: rheumatoid arthritis versus osteoarthritis. Mol Imaging Biol. 2007;9:357–60. https://doi.org/10.1007/s11307-007-0113-4.
Wong KP, Sha W, Zhang X, Huang SC. Effects of administration route, dietary condition, and blood glucose level on kinetics and uptake of 18F-FDG in mice. J Nucl Med. 2011;52:800–7. https://doi.org/10.2967/jnumed.110.085092.
Dorst DN, Rijpkema M, Buitinga M, Walgreen B, Helsen MMA, Brennan E, Klein C, Laverman P, Ramming A, Schmidkonz C, et al. Targeting of fibroblast activation protein in rheumatoid arthritis patients: imaging and ex vivo photodynamic therapy. Rheumatology (Oxford). 2021. https://doi.org/10.1093/rheumatology/keab664.
Schmidkonz C, Rauber S, Atzinger A, Agarwal R, Götz TI, Soare A, Cordes M, Prante O, Bergmann C, Kleyer A, et al. Disentangling inflammatory from fibrotic disease activity by fibroblast activation protein imaging. Ann Rheum Dis. 2020;79:1485–91. https://doi.org/10.1136/annrheumdis-2020-217408.
Acknowledgments
We would like to thank the staff at PET/CT center, Shandong Cancer Hospital, for their contributions to tracer preparation and PET/CT imaging.
Funding
This work was supported by the National Natural Science Foundation of China (Grant No. 81772760, 82072850, 81901666, 82101903), The Shandong Taishan Scholarship (Grant NO. tsqn20161076), Natural Science Foundation of Shandong Province (Grant No. ZR2020YQ55), Key Research and Development project of Shandong Province (No. 2021ZDSYS27), The Innovation Project of Shandong Academy of Medical Sciences (2021), The Youth Innovation Technology Plan of Shandong University (Grant No. 2019KJK003), and Academic Promotion Programme of Shandong First Medical University (Grant No. 2019LJ001).
Author information
Authors and Affiliations
Contributions
Conception and design: LW, KC.
Acquiring data: LG, FZ, YW, DS, SL, HS, GS, JP.
Analyzing data: HF, YZ, YG, SW, RZ.
Drafting manuscript: LG, KC.
Revising the manuscript: ZF, LG, YW, LW.
Approving the final content of the manuscript: All authors.
Corresponding authors
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent for publication
All authors approved the article for publication.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Translational research
Supplementary Information

Fig. S1
Structural formula and quality control of the probe used in this study. (a) Synthesis of [18F]AlF-NOTA-FAPI-04. (b) Analytical HPLC chromatogram of purified [18F]AlF-NOTA-FAPI-04 at 220 nm. (c) Structural formula of Cy3-FAPI-04. (PNG 155 kb)

Fig. S2
In vitro stability of [18F]AlF-NOTA-FAPI-04. Radiochemical purity of [18F]AlF-NOTA-FAPI-04 in saline and 5% HSA. HSA, human serum albumin. The data are expressed as the mean ± SEM (n=6). (PNG 36 kb)

Fig. S3
Characterization of NIH3T3 cells stably transfected with FAP overexpression or negative control adenovirusd. (a) GFP fluorescence was observed by confocal microscopy (400×). The FAP and DPP4 expression levels were determined by qPCR (b, c) and western blotting (d). The data are expressed as the mean ± SEM (n=6). ***P<0.001. (PNG 162 kb)

Fig. S4
The expression of FAP in different cells. (a) The expression of FAP in OA-derived FLSs and RA-derived FLSs obtained from disaggregated synovial tissue. (b) The expression of FAP in RA-derived FLSs, monocytes, B cells and T cells. The data are expressed as the mean ± SEM (n=6). ***P<0.001. (PNG 38 kb)

Fig. S5
Specificity of FAPI-04. (a) FAP expression and the fluorescence intensity of Cy3-FAPI-04 in GFP-NIH3T3 and FAP-GFP-NIH3T3 cells (400×). (b) DPP4 expression and the fluorescence intensity of Cy3-FAPI-04 in FAP-GFP-NIH3T3 cells (400×). (PNG 610 kb)

Fig. S6
Organ uptake of [18F]AlF-NOTA-FAPI-04 in healthly DBA/1 mice and CIA mice. (a) Normal DBA/1 mice were intravenously injected with [18F]AlF-NOTA-FAPI-04 (4.2 MBq). The organs of interest were collected at 30 min, 1 h, 2 h, and 4 h, and radioactivity was measured with a gamma counter. (b) The uptake of [18F]AlF-NOTA-FAPI-04 in CIA mice during dynamic scanning was acquired by automatic delineation of target area. The data were converted to the percentage of injected dose per mL (% ID/mL). Joint/muscle (c) and joint/blood uptake ratios (d) were calculated. The data are expressed as the mean±SEM (n=3). ***P<0.001. (PNG 316 kb)
Supplementary Table 1
Primer sequences used in this study. (DOCX 13 kb)
Supplementary Table 2
Quality control analysis of [18F]AlF-NOTA-FAPI-04. (DOCX 13 kb)
Supplementary Table 3
Clinical data of the two patients. (DOCX 12 kb)
Rights and permissions
About this article
Cite this article
Ge, L., Fu, Z., Wei, Y. et al. Preclinical evaluation and pilot clinical study of [18F]AlF-NOTA-FAPI-04 for PET imaging of rheumatoid arthritis. Eur J Nucl Med Mol Imaging 49, 4025–4036 (2022). https://doi.org/10.1007/s00259-022-05836-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-022-05836-3