Abstract
Introduction
[18F]PSMA-1007 has potential advantages over [68 Ga]Ga-PSMA-11, although limited prospective data evaluating diagnostic performance exist. The aims of this study are to describe the concordance of [18FPSMA-1007 and [68 Ga]Ga-PSMA-11 for TNM with the American Joint Committee on Cancer (AJCC) prognostic stage and assess differences in tracer uptake.
Methods
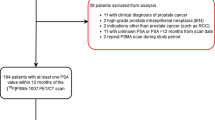
Fifty men (mean age 71.8) were imaged with [68 Ga]Ga-PSMA-11 and [18F]PSMA-1007 < 4 weeks apart. Images were independently reported according to TNM by two experienced nuclear medicine specialists blinded to the other scan and prior imaging. Discordant results were resolved by a third independent nuclear medicine specialist. Quantitative analysis of lesion uptake and physiologic tissue for each tracer was performed by one experienced reader.
Results
Scan indications were initial staging (n = 12), biochemical recurrence (n = 27) and metastatic disease evaluation (n = 11). Most patients had ISUP grade group 3 or higher. Median PSA value was 2.7 ng/ml (IQR 0.7–12.0), and a minority of patients (28%) were currently treated with androgen deprivation therapy. [18F]PSMA-1007 uptake was significantly higher than [68Ga]Ga-PSMA-11 in local recurrence, nodal and distant metastases and most physiologic sites (including bone) except for urinary bladder which was significantly lower. [18F]PSMA-1007 upstaged local prostate staging in 5/17 patients, local recurrence in 3/33 patients, regional nodal disease in 3/50 patients and 1 distant metastasis (bladder). [68Ga]Ga-PSMA-11 upstaged regional nodal disease in 1/50 patients and distant metastasis in one patient (right adrenal). Overall AJCC prognostic stage was concordant in 46/50 (92%) patients, with two patients upstaged for both [18F]PSMA-1007 and [68Ga]Ga-PSMA-11. [18F]PSMA-1007 had more equivocal results (one regional node; six equivocal bone lesions, one of which was subsequently confirmed metastatic) than [68Ga]Ga-PSMA-11 (one equivocal local recurrence).
Conclusion
Overall AJCC prognostic stage was similar (92%) between [18F]PSMA-1007 and [68Ga]Ga-PSMA-11. [18F]PSMA-1007 demonstrates higher uptake within involved nodes and distant metastases and most physiologic sites except urinary bladder which aided [18F]PSMA-1007 local staging of the prostate primary/local recurrence and regional nodal disease adjacent ureters. However, [18F]PSMA-1007 liver uptake obscured a solitary right adrenal metastasis, and more equivocal bone lesions were identified.
Trial registration
The study was registered with Australia New Zealand Clinical Trials Registry (ACTRN12618000665235) on 24 April 2018.






Similar content being viewed by others
Availability of data and material
Available upon reasonable request.
Code availability
Not applicable.
Change history
03 November 2021
A Correction to this paper has been published: https://doi.org/10.1007/s00259-021-05548-0
References
Fitzmaurice C, Allen C, Barber RM, Barregard L, Bhutta ZA, Brenner H, et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015. JAMA Oncol. 2017;3(4):524.
Hupe MC, Philippi C, Roth D, Kümpers C, Ribbat-Idel J, Becker F, et al. 2018 Expression of prostate-specific membrane antigen (PSMA) on biopsies is an independent risk stratifier of prostate cancer patients at time of initial diagnosis. Frontiers in Oncology 8.
Roberts MJ, Morton A, Donato P, Kyle S, Pattison DA, Thomas P, et al. (68)Ga-PSMA PET/CT tumour intensity pre-operatively predicts adverse pathological outcomes and progression-free survival in localised prostate cancer. Eur J Nucl Med Mol Imaging. 2021;48(2):477–82.
Hofman M, Lawrentschuk N, Francis R, Tang C, Vela I, Thomas P, et al. Prostate-specific membrane antigen PET-CT in patients with high-risk prostate cancer before curative-intent surgery or radiotherapy (proPSMA): a prospective, randomised, multicentre study. The Lancet. 2020;395(10231):1208–16.
Perera M, Papa N, Christidis D, Wetherell D, Hofman MS, Murphy DG, et al. Sensitivity, specificity, and predictors of positive (68)Ga-prostate-specific membrane antigen positron emission tomography in advanced prostate cancer: a systematic review and meta-analysis. Eur Urol. 2016;70(6):926–37.
Hofman MS, Violet J, Hicks RJ, Ferdinandus J, Thang SP, Akhurst T, et al. [(177)Lu]-PSMA-617 radionuclide treatment in patients with metastatic castration-resistant prostate cancer (LuPSMA trial): a single-centre, single-arm, phase 2 study. Lancet Oncol. 2018;19(6):825–33.
Fendler WP, Calais J, Allen-Auerbach M, Bluemel C, Eberhardt N, Emmett L, et al. 68Ga-PSMA-11 PET/CT interobserver agreement for prostate cancer assessments: an international multicenter prospective study. J Nucl Med. 2017;58(10):1617–23.
Violet J, Jackson P, Ferdinandus J, Sandhu S, Akhurst T, Iravani A, et al. Dosimetry of 177Lu-PSMA-617 in metastatic castration-resistant prostate cancer: correlations between pretherapeutic imaging and whole-body tumor dosimetry with treatment outcomes. J Nucl Med. 2019;60(4):517–23.
Rodnick ME, Sollert C, Stark D, Clark M, Katsifis A, Hockley BG, et al. Cyclotron-based production of (68)Ga, [(68)Ga]GaCl(3), and [(68)Ga]Ga-PSMA-11 from a liquid target. EJNMMI Radiopharm Chem. 2020;5(1):25.
Iravani A, Hofman MS, Mulcahy T, Williams S, Murphy D, Parameswaran BK, et al. 68Ga PSMA-11 PET with CT urography protocol in the initial staging and biochemical relapse of prostate cancer. Cancer Imaging. 2017;17(1):31.
Heußer T, Mann P, Rank CM, Schäfer M, Dimitrakopoulou-Strauss A, Schlemmer HP, et al. Investigation of the halo-artifact in 68Ga-PSMA-11-PET/MRI. PLoS ONE. 2017;12(8):e0183329.
Bailey DL, Hofman MS, Forwood NJ, O’Keefe GJ, Scott AM, Van Wyngaardt WM, et al. Accuracy of dose calibrators for 68Ga PET imaging: unexpected findings in a multicenter clinical pretrial assessment. J Nucl Med. 2018;59(4):636–8.
Giesel FL, Hadaschik B, Cardinale J, Radtke J, Vinsensia M, Lehnert W, et al. F-18 labelled PSMA-1007: biodistribution, radiation dosimetry and histopathological validation of tumor lesions in prostate cancer patients. Eur J Nucl Med Mol Imaging. 2017;44(4):678–88.
Kesch C, Vinsensia M, Radtke JP, Schlemmer HP, Heller M, Ellert E, et al. Intraindividual comparison of18F-PSMA-1007 PET/CT, multiparametric MRI, and radical prostatectomy specimens in patients with primary prostate cancer: a retrospective, proof-of-concept study. J Nucl Med. 2017;58(11):1805–10.
Giesel FL, Knorr K, Spohn F, Will L, Maurer T, Flechsig P, et al. Detection efficacy of 18F-PSMA-1007 PET/CT in 251 Patients with biochemical recurrence of prostate cancer after radical prostatectomy. J Nucl Med. 2019;60(3):362–8.
Rahbar K, Afshar-Oromieh A, Seifert R, Wagner S, Schäfers M, Bögemann M, et al. Diagnostic performance of 18F-PSMA-1007 PET/CT in patients with biochemical recurrent prostate cancer. Eur J Nucl Med Mol Imaging. 2018;45(12):2055–61.
Giesel FL, Cardinale J, Schäfer M, Neels O, Benešová M, Mier W, et al. 18F-Labelled PSMA-1007 shows similarity in structure, biodistribution and tumour uptake to the theragnostic compound PSMA-617. Eur J Nucl Med Mol Imaging. 2016;43(10):1929–30.
Rauscher I, Krönke M, König M, Gafita A, Maurer T, Horn T, et al. Matched-pair comparison of 68Ga-PSMA-11 PET/CT and 18F-PSMA-1007 PET/CT: frequency of pitfalls and detection efficacy in biochemical recurrence after radical prostatectomy. J Nucl Med. 2020;61(1):51–7.
Kuten J, Fahoum I, Savin Z, Shamni O, Gitstein G, Hershkovitz D, et al. Head-to-head comparison of 68Ga-PSMA-11 with 18F-PSMA-1007 PET/CT in staging prostate cancer using histopathology and immunohistochemical analysis as a reference standard. J Nucl Med. 2020;61(4):527–32.
Dietlein F, Kobe C, Hohberg M, Zlatopolskiy BD, Krapf P, Endepols H, et al. Intraindividual comparison of 18F-PSMA-1007 with renally excreted PSMA ligands for PSMA PET imaging in patients with relapsed prostate cancer. J Nucl Med. 2020;61(5):729–34.
Amin MB ES, Greene F, Byrd DR, Brookland RK, Washington MK, et al. AJCC cancer staging manual. 8th ed. Cancer AJCo, editor. New York: Springer International Publishing; 2017.
Yu JB, Makarov DV, Gross C. A new formula for prostate cancer lymph node risk. Int J Radiat Oncol Biol Phys. 2011;80(1):69–75.
Wang YJ, Huang CY, Hou WH, Wang CC, Lan KH, Chen CH, et al. The outcome and prognostic factors for lymph node recurrence after node-sparing definitive external beam radiotherapy for localized prostate cancer. World J Surg Oncol. 2015;13:312.
D’Amico AV, Chen MH, Renshaw A, Loffredo M, Kantoff PW. Long-term follow-up of a randomized trial of radiation with or without androgen deprivation therapy for localized prostate cancer. JAMA. 2015;314(12):1291–3.
Wondergem M, Van Der Zant FM, Broos WA, Knol RJ. Matched-pair comparison of 18F-DCFPyL PET/CT and 18F-PSMA-1007 PET/CT in 240 prostate cancer patients; inter-reader agreement and lesion detection rate of suspected lesions. Journal of Nuclear Medicine. 2021:jnumed.120.2585.
Giesel FL, Will L, Kesch C, Freitag M, Kremer C, Merkle J, et al. Biochemical recurrence of prostate cancer: initial results with [18F]PSMA-1007 PET/CT. J Nucl Med. 2018;59(4):632–5.
Ende JAA, Sheehan-Dare G, Cusick T, Ho B, Keane J, et al. Pilot trial comparing the performance of 68Ga-PSMA-11 PET/CT to 18F-PSMA-1008 PET/CT in the detection of prostate cancer recurrence in men with rising PSA following radical prostatectomy. J Radiol Med Imaging. 2021;4(1):1039.
Hartrampf PE, Seitz AK, Krebs M, Buck AK, Lapa C. False-negative 18F-PSMA-1007 PET/CT in metastatic prostate cancer related to high physiologic liver uptake. Eur J Nucl Med Mol Imaging. 2020;47(8):2044–6.
Chiu LW, Lawhn-Heath C, Behr SC, Juarez R, Perez PM, Lobach I, et al. Factors predicting metastatic disease in 68Ga-PSMA-11 PET–positive osseous lesions in prostate cancer. J Nucl Med. 2020;61(12):1779–85.
Arnfield EG, Thomas PA, Roberts MJ, Pelecanos AM, Ramsay SC, Lin CY, et al. Clinical insignificance of [18F]PSMA-1007 avid non-specific bone lesions: a retrospective evaluation. European Journal of Nuclear Medicine and Molecular Imaging. 2021.
Acknowledgements
We would like to acknowledge the effort of nuclear medicine technologists, nursing and medical staff at Royal Brisbane and Women’s Hospital and Q-TRaCE (QLD—The Radiopharmaceutical Centre of Excellence) radiochemistry staff who supported and contributed to the running of this trial, in addition to the enthusiastic participation of our patients. We are also grateful to Marita Prior for assistance with trial administration.
Funding
No funding was received for conducting this study. Matthew J Roberts is supported by a Clinician Research Fellowship from the Metro North Office of Research, Queensland Health, and a Doctor in Training Research Scholarship from Avant Mutual Group Pty Ltd.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design, or acquiring data, or analysing and interpreting data. Material preparation, data collection and analysis were performed by Maciej Debowski, Brook Gulhane, Evyn Arnfield, David Pattison, Stuart Ramsay and Paul Thomas. The first draft of the manuscript was written by David Pattison, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This trial was approved by the institutional review board of the Royal Brisbane and Women’s Hospital Human Research Ethics Committee and was conducted in accordance with 1964 Helsinki Declaration. Written informed consent for participation and publication was provided.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Oncology–Genitourinary
Stuart C. Ramsay and Paul A. Thomas contributed equally to this work
The original online version of this article was revised: The authors regret that the figure legends in the original article are correct but the images for Figure 5 and Figure 6 need to be swapped.
The original article has been corrected.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Pattison, D.A., Debowski, M., Gulhane, B. et al. Prospective intra-individual blinded comparison of [18F]PSMA-1007 and [68 Ga]Ga-PSMA-11 PET/CT imaging in patients with confirmed prostate cancer. Eur J Nucl Med Mol Imaging 49, 763–776 (2022). https://doi.org/10.1007/s00259-021-05520-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-021-05520-y