Abstract
Purpose
The coronavirus disease 2019 (COVID-19) pandemic reshaped the usual risk: benefit equilibrium that became a trade-off between the infection exposure risk for the patient (and for staff) and the risk associated with delaying or cancelling the nuclear medicine examination. This study aimed at quantifying the impact of the first COVID-19 lockdown in France on nuclear medicine examination volume together with volume of examination cancellation and non-attendance.
Methods
We retrospectively assessed the volume of planned examinations from 1 month before to 1 month after the first lockdown in French high-volume nuclear medicine departments (NMD) sharing the same information management system including both university hospitals, UH (n = 7), and cancer centres, CC (n = 2).
Results
The study enrolled 31,628 consecutive patients referred for a nuclear medicine examination performed or not (NMEP or NMEnP). The total volume of NMEP significantly dropped by 43.4% between the 4 weeks before and after the starting of the lockdown. The comparison of the percentage of NMEP and NMEnP between UH and CC is significantly different (p < 0.001). The percentage of NMEP during the study was 67.9% in UH vs 84.7% in CC. Percentages of NMEnP in UH and CC were due respectively to cancellation by the patient (14.9 vs 7.4%), cancellation by the NMD (9.5 vs 3.4%), cancellation by the referring physician (5.1 vs 4.4%) and non-attender patients (2.7 vs 0.2%).
Conclusion
The study underlines the public health issue caused by COVID-19 above the pandemic itself and should be useful in preparing for potential resource utilisation and staffing requirements.
Similar content being viewed by others
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has largely impaired the access to healthcare providers and is still hampering the management of patients with elective problems. Different countries experienced a lockdown that had a major impact on the volume and processes of care for patients without COVID-19 [1,2,3,4,5]. The nuclear medicine community which deals with both in- and outpatients suffering from various conditions had to reconsider its practice globally [6,7,8,9]. This unique situation allowed to reveal the potential of using 2-deoxy-2-[18F]fluoro-D-glucose ([18F]FDG) positron emission tomography combined with computed tomography (PET/CT) to incidentally detect asymptomatic patients suspected of COVID-19 infection. Also, the prevalence of incidental findings suggestive of COVID-19 detected with [18F]FDG PET/CT was directly related to the prevalence of COVID-19 locally [10, 11]. This pandemic and ultimately the associated lockdown situations reshaped the usual risk: benefit equilibrium that became a trade-off between the infection exposure risk for the patient (and for staff) and the risk associated with delaying or cancelling the nuclear medicine examination. Different teams assessed the impact of the pandemic on nuclear medicine either quantitatively together with the other medical imaging volumes [12, 13] either qualitatively but with details regarding the nuclear medicine subspecialties [14,15,16]. The authors of these studies reported an important drop in volumes of nuclear medicine scans globally. However, among the different nuclear medicine examinations, PET/CT, that is, predominantly indicated in oncology had a declared average decline inferior to conventional nuclear medicine and nuclear cardiology. So far, the different published studies and surveys conducted were unable to differentiate whether reduced numbers of nuclear medicine studies and interventions were due to the patient, the prescriber or the nuclear medicine physician to postpone or cancel examinations. We aimed to evaluate and quantify the impact of the COVID-19 nationwide lockdown in France on nuclear medicine departments in both university hospitals and cancer centres. This study (named the CORALINE study) especially assessed the volume of nuclear medicine examinations and applicant of cancelled examinations together with patient non-attendance.
Methods
Study design
The CORALINE study retrospectively enrolled all patients referred for a nuclear medicine examination at nine French high-volume centres (usually more than 6000 patients per year) including university hospitals (Caen Normandie, Grenoble Alpes, Hospices Civils Lyon Est, Hospices Civils Lyon Sud, Nantes, Saint-Etienne and Bichat-Claude-Bernard Hospital Assistance Publique-Hôpitaux de Paris) and cancer centres (Nantes Institut de cancérologie de l’Ouest and Rennes Centre Eugène Marquis). In France, university hospitals provide care in a wide range of disciplines including oncology whereas cancer centres are only focused on oncological diseases. The study was approved by the local research ethics committee (Comité local d’éthique de la recherche en santé, CHU de CAEN Normandie – Université de CAEN Normandie) under registration number 1565. Dates of interest in France were as follows: March 17, 2020, lockdown; March 18, 2020, guidelines of the French Society for Nuclear Medicine; March 27, 2020, first extension of lockdown; April 13, 2020, second extension of lockdown; May 11, 2020, end of lockdown. Inclusion criteria consisted of all patients who had a scheduled nuclear medicine examination without exclusion criteria. Data were collected using the nuclear medicine information management software GERA (Thélème, Angers, France) including the following: date of scheduled examination, type of examination (conventional nuclear medicine, nuclear cardiology, positron emission tomography), group of examination (diagnostic or therapeutic), gender (male of female), age, status of patient (inpatient or outpatient), venue of the patient to the scheduled examination (yes or no), cancellation of the examination: attenders, cancellers and non-attenders (cancelled by the patient, cancelled by the referring physician, cancelled by the nuclear medicine physician, not cancelled and the patient came, not cancelled and the patient did not come also called non-attenders), and centre where the nuclear medicine examination was scheduled. Each centre investigator was asked about their local policies regarding the management of patients and scheduling of nuclear medicine examination during lockdown with open-ended questions.
Statistical analysis
Data are summarised as mean and standard deviation (SD) for continuous variables and percentage for categorical variables. Means were compared using the Student t test after testing the assumption of homoscedasticity by the Levene test and percentages by the chi-square test or Fisher’s exact test.
A 2-tailed p value of less than 0.05 was considered as statistically significant. All statistical analyses were performed using IBM Corp. Released 2015. IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY, IBM Corp.
Results
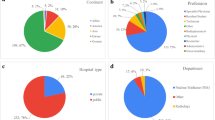
Between February the 17th 2020 (1 month before the starting of the lockdown in France) and the 11th of June 2020 (1 month after the end of the lockdown), the CORALINE study retrospectively enrolled 31,628 consecutive patients referred for a nuclear medicine examination at nine high-volume centres (7 university hospitals and 2 cancer centres). The total volume of examinations performed was 23,307 (30,779 at the same period in 2019); it significantly dropped by 43.4% between weeks 8–11 and weeks 12–15 (i.e. 4 weeks before and 4 weeks after the March 17, 2020, lockdown in France). Then, decreased by 43.0% between weeks 8–11 and weeks 16–19 (i.e. 4 weeks before the lockdown and the 4 weeks between the second extension and the end of the lockdown) before a volume recovery (+2.9%) between weeks 8–11 and weeks 20–24 (i.e. 4 weeks before and after the lockdown) as shown in Fig. 1. Also, the observed decrease of examinations was not on the same order of magnitude depending on the type of examination performed (−52.8%, −76.5% and − 13.4% for conventional nuclear medicine, nuclear cardiology and positron emission tomography, respectively) between weeks 8–11 and weeks 12–15 as shown in Fig. 2. Then, a progressive partial recovery in examinations volume occurred in the following weeks. Conversely, the number of examinations not performed (including cancellation and missed appointments) followed an inverse evolution over time (Figs. 1 and 2) with an increase by 138.67% between weeks 8–11 and weeks 12–15, 22.9% between weeks 8–11 and weeks 16–19, and 9.2% between weeks 8–11 and weeks 20–24. The percentage of patients who attended their nuclear medicine examination during the study was 67.9% in university hospitals and 84.7% in cancer centres (p < 0.001) as shown in Fig. 3. The proportions of non-performed examinations in university hospitals and cancer centres were significantly different and due to cancellation by the patient (14.9 vs 7.4%), cancellation by the nuclear medicine department (9.5 vs 3.4%), cancellation by the referring physician (5.1 vs 4.4%) and non-attenders patients (2.7 vs 0.2%). Major age categories were 31–65 and 66–80 for attenders (46.8 and 37.7%), and cancellers and non-attenders patients (42.2 and 39.6%) as shown in Fig. 4 and Table 1. Patient characteristics of the studied population for attenders on one hand and cancellers and non-attenders on the other hand are summarised in Table 1. Briefly, non-attenders and canceller patients were significantly overrepresented in the following characteristics: hospitalised, male, over 66 years old and referred for a diagnostic examination especially a nuclear cardiology procedure compared with attenders. The volume of examinations performed and not performed over time differed between centres as depicted in Fig. 5 (supplemental file) and Table 2. Most university hospitals experienced a drop in examinations performed in the first weeks following the lockdown combined with a rise in non-performed examinations that exceeded the number of examinations performed (Fig. 5; 1, 2, 3, 4, 5 and 6). Interestingly, cancer centres (Fig. 5; 7 and 8) and a university hospital that has a major cancer diagnosis and treatment activity (Fig. 5; 9) displayed a relatively stable amount of examination volume over time.
Timeline of nuclear medicine examinations volume in the French participating centres, before, during and after the first COVID-19 lockdown from February 17 to June 11, 2020. Weekly planned examination volumes that were performed (green bars) and not performed (red bars) are represented. *SFMN is the French acronym for French Society of Nuclear Medicine
Timeline of nuclear medicine examinations volume by type of planned procedure in the French participating centres, before, during and after the first COVID-19 lockdown from February 17 to June 11, 2020. Weekly planned examination volumes that were performed (up) and not performed (down) of positron emission tomography (blue), conventional nuclear medicine (green) and nuclear cardiology (red) are represented
Comparison of the percentage of nuclear medicine examinations performed (attenders) and not performed (cancellation by the patient, cancellation by the department, cancellation by the referring physician and non-attenders) between university hospitals (n = 7) and cancer centres (n = 2) from February 17 to June 11, 2020
Timeline of nuclear medicine examination volume by age of patients in the French participating centres before, during and after the first COVID-19 lockdown from February 17 to June 11, 2020. Weekly planned examination volumes that were not performed (up) and performed (down) are represented. Age categories in years were 0–17 (blue), 18–30 (green), 31–65 (yellow), 66–80 (purple) and over 80 (red)
Discussion
Nuclear medicine has been one of the imaging modalities that exhibited the greatest degree of volume reduction during the COVID-19 pandemic [12, 13, 17, 18]. In our study, we observed a reduction of around 43% in nuclear medicine examinations volume between the periods directly before and during the lockdown. Then, the volume of examinations almost recovered when comparing 4 weeks before the lockdown and 4 weeks after the end of the lockdown. Depending on the type of nuclear medicine examinations, the drop/recovery in imaging volume was of different magnitude between conventional nuclear medicine, nuclear cardiology and positron emission tomography. The provided quantitative results regarding the drop in nuclear medicine imaging volume are consistent with the global qualitative assessment published so far [14]. Our results are in line with those from the global declarative study of Freudenberg et al. study that reported an average decline of 54% (36% for PET and 66% for nuclear cardiology) [14] or the quantitative results from Madhuripan et al. who found a maximum 44% decrease compared to baseline (37% for PET and 76% for other nuclear medicine examinations) in a large centre in the USA [12]. We also observed a drop of nearly 24.5% of examinations performed between 2019 and 2020 at the same period. Furthermore, the trend in examination volume drop and recovery were temporally related to national public health announcements such as depicted by Lang et al. [17].
To our knowledge, no prior publications have quantified the cancellation of nuclear medicine examinations and composition mix during the COVID-19 pandemic stratified by applicant of the cancellation and identification of non-attenders. As expected, we observed an inverse trend in the volume of cancelled nuclear medicine examinations compared to performed examinations characterised by an increase followed by a normalisation that were also temporally related to national public health announcements. Interestingly, patients were the most frequent applicants to examinations cancellation in both university hospitals and cancer centres with nearly 15% and 8% of global cancellation rate respectively. These findings suggest public health awareness of the population regarding the infection transmission risk together with a potential level of stress related to the COVID-19 pandemic that was shown to be particularly high during lockdown [19] and might have affected the way patients have used healthcare facilities. We found that inpatients, male, referred for a diagnostic examination were statistically more represented in the cancelled nuclear medicine examinations. Over-representation of inpatients may be attributed to hospitals’ policies to avoid nosocomial infections in the pandemic context. Naidich et al. [18] observed in a large integrated healthcare system a decline of around 50% in nuclear medicine examinations volume between the pre- and post-COVID-19 periods for inpatients. Diagnostic examinations were more cancelled or non-attended compared to therapeutic nuclear medicine procedures probably because the latter are dedicated to treat oncological diseases. Male were more inclined to cancel or non-attend their planned examination, this observation with previously published data [20]. Non-attendance is well known as a major cause of inefficiency in healthcare delivery with substantial monetary costs for the health system that lead to delays in diagnosis and appropriate treatment [20]. In our study, non-attenders represented 2.7% and 0.2% (p < 0.001) of planned examinations for university hospitals and cancer centres, respectively; this difference might be explained by patients’ perception regarding their conditions giving priority to oncological diseases. However, the non-attendance rate can be considered low compared with previous studies conducted in outpatient departments [21,22,23]. Rosenbaum et al. observed the rate of no-show visits in 2.9 million outpatients scheduled for an imaging examination including radiology and nuclear medicine over 16 years; they found that modality type and scheduling lead time were the most predictive factors of no-show [23]. Patients’ forgetfulness is known to be one of the main reasons for missed appointments [24] and can be related to scheduling lead time but it remains to assess if other important associated factors may explain missed appointments in the context of a pandemic. For instance, during the first lockdown in France, patients were allowed to travel with a specific authorisation for different needs including: “Consultations and care that cannot be provided remotely and cannot be postponed”. However, we may probably assume that the restrictive policies of the lockdown may have led patients to cancel their nuclear medicine examinations. We reported herein a significant difference of trend between university hospitals and cancer centres that was not previously assessed. The French COVID-19 guidelines regarding nuclear medicine may be able to explain why the imaging volume in cancer centres was less affected than in most of the university hospitals. Indeed, the French society for nuclear medicine especially advised to maintain examinations planned for oncological indications [25]. These guidelines were followed by all participating centres of the study. University hospitals mostly cancelled non-oncological examinations explaining the difference of volume evolution with cancer centres. So far, the hospital size was identified as a factor positively associated with volume of examination during the pandemic. Indeed, Lang et al. compared imaging volumes between a large academic urban hospital and its affiliated imaging centre in which they found a decrease to a greater degree than in the main hospital campus and showed a slower rate of recovery [17]. Our presented data support that the kind of medical activity practiced is also to consider as an important factor associated with the trend of examinations volume. Therefore, a scoring system to rank the timeframe of examinations may be proposed and conducted by local committees of experts.
The main limitations of this work are the use of a retrospective study design analysing aggregated and anonymised data. Although the overwhelming majority of PET examinations were dedicated to oncological explorations, they are not restricted to these indications and included patients referred for non-oncological diseases. The study did not assess if cancellers and non-attenders were systematically rescheduled for a new appointment. Also, the reason of cancellation is not tracked in our nuclear medicine information software. As radiopharmaceuticals’ supply in France during the first lockdown was well maintained, as attested by the authors’ experience, this reason can be considered very minor. Further studies are needed to assess if an activity rebound able to compensate cancelled examinations is observed and to quantify patient outcomes in terms of delayed treatment, morbidity/mortality and patient satisfaction. Studies aiming at to correlate the presented data with the local COVID-19 prevalence rate are ongoing.
The results from this study reflect the impact of the COVID-19 pandemic on practice and may have significant implications for health authorities preparing for management of the COVID-19 crisis. These real-world data underline the major public health issue caused by COVID-19 above the pandemic itself and should be useful in preparing for potential resource utilisation and staffing requirements.
References
Laccourreye O, Mirghani H, Evrard D, Bonnefont P, Brugel L, Tankere F, et al. Impact of the first month of Covid-19 lockdown on oncologic surgical activity in the Ile de France region university hospital otorhinolaryngology departments. Eur Ann Otorhinolaryngol Head Neck Dis. 2020;137:273–6. https://doi.org/10.1016/j.anorl.2020.06.007.
Mesnier J, Cottin Y, Coste P, Ferrari E, Schiele F, Lemesle G, et al. Hospital admissions for acute myocardial infarction before and after lockdown according to regional prevalence of COVID-19 and patient profile in France: a registry study. Lancet Public Health. 2020;5:e536–42. https://doi.org/10.1016/S2468-2667(20)30188-2.
Cransac-Miet A, Zeller M, Chagué F, Faure AS, Bichat F, Danchin N, et al. Impact of COVID-19 lockdown on lifestyle adherence in stay-at-home patients with chronic coronary syndromes: towards a time bomb. Int J Cardiol. 2020. https://doi.org/10.1016/j.ijcard.2020.08.094.
Pignon B, Gourevitch R, Tebeka S, Dubertret C, Cardot H, Masson VD-L, et al. Dramatic reduction of psychiatric emergency consultations during lockdown linked to COVID-19 in Paris and suburbs. Psychiatry Clin Neurosci. 2020;74:557–9. https://doi.org/10.1111/pcn.13104.
Helissey C, Cessot A, Boudin L, Romeo E, Prieux C, Ghebriou D, et al. Evaluation of medical practices in oncology in the context of the COVID-19 pandemic in France: physicians’ point of view: the PRATICOVID study. Cancer Med. https://doi.org/10.1002/cam4.3503.
Skali H, Murthy VL, Paez D, Choi EM, Keng FYJ, Iain MA, et al. Guidance and best practices for reestablishment of non-emergent care in nuclear cardiology laboratories during the coronavirus disease 2019 (COVID-19) pandemic: an information statement from ASNC, IAEA, and SNMMI. J Nucl Med. 2020;61:1534–9. https://doi.org/10.2967/jnumed.120.251355.
Paez D, Gnanasegaran G, Fanti S, Bomanji J, Hacker M, Sathekge M, et al. COVID-19 pandemic: guidance for nuclear medicine departments. Eur J Nucl Med Mol Imaging. 2020;47:1615–9. https://doi.org/10.1007/s00259-020-04825-8.
Vigne J, Aide N, Peyronnet D, Nganoa C, Agostini D, Barbey P. When nuclear medicine radiological protection meets biological COVID-19 protection. Eur J Nucl Med Mol Imaging. 2020;47:1802–5. https://doi.org/10.1007/s00259-020-04806-x.
Cutler CS, Bailey EA, Kumar V, Schwarz SW, Bom HH-S, Hatazawa J, et al. Global issues of radiopharmaceutical access and availability: a nuclear medicine global initiative project. J Nucl Med Off Publ Soc Nucl Med. 2020. https://doi.org/10.2967/jnumed.120.247197.
Albano D, Bertagna F, Alongi P, Baldari S, Baldoncini A, Bartolomei M, et al. Prevalence of interstitial pneumonia suggestive of COVID-19 at 18 F-FDG PET/CT in oncological asymptomatic patients in a high prevalence country during pandemic period: a national multi-centric retrospective study. Eur J Nucl Med Mol Imaging. 2021. https://doi.org/10.1007/s00259-021-05219-0.
Annunziata S, Delgado Bolton RC, Kamani C-H, Prior JO, Albano D, Bertagna F, et al. Role of 2-[18F]FDG as a radiopharmaceutical for PET/CT in patients with COVID-19: a systematic review. Pharmaceuticals. 2020;13:377. https://doi.org/10.3390/ph13110377.
Madhuripan N, Cheung HMC, Alicia Cheong LH, Jawahar A, Willis MH, Larson DB. Variables influencing radiology volume recovery during the next phase of the coronavirus disease 2019 (COVID-19) pandemic. J Am Coll Radiol. 2020;17:855–64. https://doi.org/10.1016/j.jacr.2020.05.026.
Naidich JJ, Boltyenkov A, Wang JJ, Chusid J, Hughes D, Sanelli PC. Impact of the coronavirus disease 2019 (COVID-19) pandemic on imaging case volumes. J Am Coll Radiol. 2020;17:865–72. https://doi.org/10.1016/j.jacr.2020.05.004.
Freudenberg LS, Paez D, Giammarile F, Cerci J, Modiselle M, Pascual TNB, et al. Global impact of COVID-19 on nuclear medicine departments: an international survey in April 2020. J Nucl Med. 2020;61:1278–83. https://doi.org/10.2967/jnumed.120.249821.
Annunziata S, Bauckneht M, Albano D, Argiroffi G, Calabrò D, Abenavoli E, et al. Impact of the COVID-19 pandemic in nuclear medicine departments: preliminary report of the first international survey. Eur J Nucl Med Mol Imaging. 2020:1–10. https://doi.org/10.1007/s00259-020-04874-z.
Annunziata S, Albano D, Laudicella R, Bauckneht M. Surveys on COVID-19 in nuclear medicine: what happened and what we learned. Clin Transl Imaging. 2020:1–3. https://doi.org/10.1007/s40336-020-00391-z.
Lang M, Yeung T, Mendoza DP, Flores EJ, Som A, Lang AL, et al. Imaging volume trends and recovery during the COVID-19 pandemic: a comparative analysis between a large urban academic hospital and its affiliated imaging centers. Acad Radiol. 2020;27:1353–62. https://doi.org/10.1016/j.acra.2020.08.008.
Naidich JJ, Boltyenkov A, Wang JJ, Chusid J, Hughes D, Sanelli PC. Coronavirus disease 2019 (COVID-19) pandemic shifts inpatient imaging utilization. J Am Coll Radiol. 2020;17:1289–98. https://doi.org/10.1016/j.jacr.2020.06.011.
Droit-Volet S, Gil S, Martinelli N, Andant N, Clinchamps M, Parreira L, et al. Time and Covid-19 stress in the lockdown situation: time free, «dying» of boredom and sadness. PLoS One. 2020;15:e0236465. https://doi.org/10.1371/journal.pone.0236465.
Sharp DJ, Hamilton W. Non-attendance at general practices and outpatient clinics. BMJ. 2001;323:1081–2.
Hamilton W, Round A, Sharp D. Effect on hospital attendance rates of giving patients a copy of their referral letter: randomised controlled trial. BMJ. 1999;318:1392–5.
King A, David D, Jones HS, O’Brien C. Factors affecting non-attendance in an ophthalmic outpatient department. J R Soc Med. 1995;88:88–90.
Rosenbaum JI, Mieloszyk RJ, Hall CS, Hippe DS, Gunn ML, Bhargava P. Understanding why patients no-show: observations of 2.9 million outpatient imaging visits over 16 years. J Am Coll Radiol. 2018;15:944–50. https://doi.org/10.1016/j.jacr.2018.03.053.
Car J, Gurol-Urganci I, de Jongh T, Vodopivec-Jamsek V, Atun R. Mobile phone messaging reminders for attendance at healthcare appointments. Cochrane Database Syst Rev. 2012:CD007458. https://doi.org/10.1002/14651858.CD007458.pub2.
la SFMN - COVID-19 n.d. https://www.sfmn.org/index.php/congres-internationaux/402-covid-19. Accessed December 16, 2020.
Acknowledgements
The authors deeply thank the Thélème company (Angers, France) for their help in collecting the data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All procedures performed were in accordance with the ethical standards of our institution. The study was approved by the local research ethics committee (Comité local d’éthique de la recherche en santé, CHU de CAEN Normandie – Université de CAEN Normandie) under registration number 1565.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Miscellanea
Supplementary Information
ESM 1
a Timeline of nuclear medicine examination volume by participating centres (1–9) before during and after the first COVID-19 lockdown from February 17 to June 11, 2020, in France. Weekly planned examination volumes that were performed (green bars) and not performed (red bars) are represented. b Localisation of the seven university hospitals (blue dots) and two cancer centres (red dots) participating to the study. 1, 2, 3, 5, 6 and 9: University hospitals of Caen, Grenoble, Lyon Est, Nantes, Paris Bichat and Saint-Etienne. 7 and 8: Cancer centres of Rennes and Nantes (JPG 18267 kb)
Rights and permissions
About this article
Cite this article
Vigne, J., Peyronnet, D., Leenhardt, J. et al. Quantitative impact of the first COVID-19 lockdown on nuclear medicine in France: the CORALINE study. Eur J Nucl Med Mol Imaging 48, 4331–4338 (2021). https://doi.org/10.1007/s00259-021-05361-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-021-05361-9