Abstract
Purpose
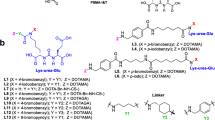
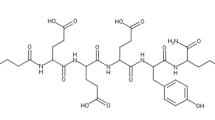
Peptide-based prostate-specific membrane antigen (PSMA) targeted radionuclide therapy (TRT) agent [177Lu]-PSMA-617 has emerged as leading TRT candidate for treatment of castration-resistant prostate cancer (mCRPC). [177Lu]-PSMA-617 and other small molecule–based PSMA ligands have shown efficacy in reducing the tumor burden in mCRPC patients but irradiation to the salivary gland and kidneys is a concern and dose-limiting factor. Therefore, methods to reduce non-target organ toxicity are needed to safely treat patients and preserve their quality of life. Herein, we report that addition of cold PSMA ligand PSMA-11 can aid in reducing the uptake of [177Lu]-PSMA-617 in the salivary glands and kidneys.
Methods
Groups of athymic nude mice (n = 4) bearing PC3-PIP (PSMA+) tumor xenografts were administered with [177Lu]-PSMA-617 along with 0, 5, 100, 500, 1000, and 2000 pmoles of PSMA-11 and biodistribution studies were performed at 1 h.
Results
Biodistribution studies at 1 h post-administration revealed that [177Lu]-PSMA-617 uptake in PC3-PIP tumors was 21.71 ± 6.13, 18.7 ± 2.03, 26.44 ± 2.94, 16.21 ± 3.5, 13.52 ± 3.68, and 12.03 ± 1.96 %ID/g when 0, 5, 100, 500, 1000, and 2000 pmoles of PSMA-11 were added, respectively. Corresponding uptake values in kidney were 123.14 ± 52.52, 132.31 ± 47.4, 84.29 ± 78.25, 2.12 ± 1.88, 1.16 ± 0.36, and 0.64 ± 0.23 %ID/g, respectively. Corresponding salivary gland uptake values were 0.48 ± 0.11, 0.45 ± 0.15, 0.38 ± 0.3, 0.08 ± 0.03, 0.09 ± 0.07, and 0.05 ± 0.02 % ID/g, respectively.
Conclusion
The uptake of [177Lu]-PSMA-617 in the salivary gland and kidney can be substantially reduced without significantly impacting tumor uptake by adding cold PSMA-11.



Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70:7–30. https://doi.org/10.3322/caac.21590.
Kratochwil C, Haberkorn U, Giesel FL. Radionuclide therapy of metastatic prostate cancer. Semin Nucl Med. 2019;49:313–25. https://doi.org/10.1053/j.semnuclmed.2019.02.003.
O’Keefe DS, Bacich DJ, Heston WD. Comparative analysis of prostate-specific membrane antigen (PSMA) versus a prostate-specific membrane antigen-like gene. Prostate. 2004;58:200–10. https://doi.org/10.1002/pros.10319.
Evans MJ, Smith-Jones PM, Wongvipat J, Navarro V, Kim S, Bander NH, et al. Noninvasive measurement of androgen receptor signaling with a positron-emitting radiopharmaceutical that targets prostate-specific membrane antigen. Proc Natl Acad Sci U S A. 2011;108:9578–82. https://doi.org/10.1073/pnas.1106383108.
Uchida A, O’Keefe DS, Bacich DJ, Molloy PL, Heston WDW. In vivo suicide gene therapy model using a newly discovered prostate-specific membrane antigen promoter/enhancer: a potential alternative approach to androgen deprivation therapy. Urology. 2001;58:132–9. https://doi.org/10.1016/S0090-4295(01)01256-0.
Yu YP, Landsittel D, Jing L, Nelson J, Ren B, Liu L, et al. Gene expression alterations in prostate cancer predicting tumor aggression and preceding development of malignancy. J Clin Oncol. 2004;22:2790–9. https://doi.org/10.1200/JCO.2004.05.158.
Kawakami M, Nakayama J. Enhanced expression of prostate-specific membrane antigen gene in prostate cancer as revealed by in situ hybridization. Cancer Res. 1997;57:2321–4.
Denmeade SR, Sokoll LJ, Dalrymple S, Rosen DM, Gady AM, Bruzek D, et al. Dissociation between androgen responsiveness for malignant growth vs. expression of prostate specific differentiation markers PSA, hK2, and PSMA in human prostate cancer models. Prostate. 2003;54:249–57. https://doi.org/10.1002/pros.10199.
Kratochwil C, Giesel FL, Stefanova M, Benesova M, Bronzel M, Afshar-Oromieh A, et al. PSMA-targeted radionuclide therapy of metastatic castration-resistant prostate cancer with 177Lu-labeled PSMA-617. J Nucl Med. 2016;57:1170–6. https://doi.org/10.2967/jnumed.115.171397.
Han M, Partin AW. Current clinical applications of the in-capromab pendetide scan (ProstaScint(R) Scan, Cyt-356). Rev Urol. 2001;3:165–71.
Pandit-Taskar N, O’Donoghue JA, Durack JC, Lyashchenko SK, Cheal SM, Beylergil V, et al. A phase I/II study for analytic validation of 89Zr-J591 immunoPET as a molecular imaging agent for metastatic prostate cancer. Clin Cancer Res. 2015;21:5277–85. https://doi.org/10.1158/1078-0432.CCR-15-0552.
Pandit-Taskar N, O’Donoghue JA, Divgi CR, Wills EA, Schwartz L, Gonen M, et al. Indium 111-labeled J591 anti-PSMA antibody for vascular targeted imaging in progressive solid tumors. EJNMMI Res. 2015;5:28. https://doi.org/10.1186/s13550-015-0104-4.
Tagawa ST, Milowsky MI, Morris M, Vallabhajosula S, Christos P, Akhtar NH, et al. Phase II study of Lutetium-177-labeled anti-prostate-specific membrane antigen monoclonal antibody J591 for metastatic castration-resistant prostate cancer. Clin Cancer Res. 2013;19:5182–91. https://doi.org/10.1158/1078-0432.CCR-13-0231.
Vallabhajosula S, Goldsmith SJ, Kostakoglu L, Milowsky MI, Nanus DM, Bander NH. Radioimmunotherapy of prostate cancer using Y-90- and Lu-177-labeled J591 monoclonal antibodies: effect of multiple treatments on myelotoxicity. Clin Cancer Res. 2005;11:7195 s–200 s. https://doi.org/10.1158/1078-0432.CCR-1004-0023.
Kiess AP, Banerjee SR, Mease RC, Rowe SP, Rao A, Foss CA, et al. Prostate-specific membrane antigen as a target for cancer imaging and therapy. Q J Nucl Med Mol Imaging. 2015;59:241–68.
Pandit-Taskar N, O’Donoghue JA, Ruan S, Lyashchenko SK, Carrasquillo JA, Heller G, et al. First-in-human imaging with 89Zr-Df-IAB2M anti-PSMA minibody in patients with metastatic prostate cancer: pharmacokinetics, biodistribution, dosimetry, and lesion uptake. J Nucl Med. 2016;57:1858–64. https://doi.org/10.2967/jnumed.116.176206.
Frigerio B, Morlino S, Luison E, Seregni E, Lorenzoni A, Satta A, et al. Anti-PSMA I-124-scFvD2B as a new immuno-PET tool for prostate cancer: preclinical proof of principle. J Exp Clin Cancer Res. 2019:38. https://doi.org/10.1186/S13046-019-1325-6.
Nawaz S, Mullen GED, Sunassee K, Bordoloi J, Blower PJ, Ballinger JR. Simple, mild, one-step labelling of proteins with gallium-68 using a tris(hydroxypyridinone) bifunctional chelator: a Ga-68-THP-scFv targeting the prostate-specific membrane antigen. EJNMMI Res. 2017:7. https://doi.org/10.1186/s13550-017-0336-6.
Foss CA, Mease RC, Fan H, Wang Y, Ravert HT, Dannals RF, et al. Radiolabeled small-molecule ligands for prostate-specific membrane antigen: in vivo imaging in experimental models of prostate cancer. Clin Cancer Res. 2005;11:4022–8. https://doi.org/10.1158/1078-0432.CCR-04-2690.
Rowe SP, Drzezga A, Neumaier B, Dietlein M, Gorin MA, Zalutsky MR, et al. Prostate-specific membrane antigen-targeted radiohalogenated PET and therapeutic agents for prostate cancer. J Nucl Med. 2016;57:90S–6S. https://doi.org/10.2967/jnumed.115.170175.
Afshar-Oromieh A, Babich JW, Kratochwil C, Giesel FL, Eisenhut M, Kopka K, et al. The rise of PSMA ligands for diagnosis and therapy of prostate cancer. J Nucl Med. 2016;57:79s–89s. https://doi.org/10.2967/jnumed.115.170720.
Wester HJ, Schottelius M. PSMA-targeted radiopharmaceuticals for imaging and therapy. Semin Nucl Med. 2019;49:302–12. https://doi.org/10.1053/j.semnuclmed.2019.02.008.
Afshar-Oromieh A, Haberkorn U, Eder M, Eisenhut M, Zechmann CM. [Ga-68]Gallium-labelled PSMA ligand as superior PET tracer for the diagnosis of prostate cancer: comparison with F-18-FECH. Eur J Nucl Med Mol Imaging. 2012;39:1085–6. https://doi.org/10.1007/s00259-012-2069-0.
Afshar-Oromieh A, Malcher A, Eder M, Eisenhut M, Linhart HG, Hadaschik BA, et al. PET imaging with a [68Ga]gallium-labelled PSMA ligand for the diagnosis of prostate cancer: biodistribution in humans and first evaluation of tumour lesions. Eur J Nucl Med Mol Imaging. 2013;40:486–95. https://doi.org/10.1007/s00259-012-2298-2.
Zechmann CM, Afshar-Oromieh A, Armor T, Stubbs JB, Mier W, Hadaschik B, et al. Radiation dosimetry and first therapy results with a (124)I/(131)I-labeled small molecule (MIP-1095) targeting PSMA for prostate cancer therapy. Eur J Nucl Med Mol Imaging. 2014;41:1280–92. https://doi.org/10.1007/s00259-014-2713-y.
Hofman MS, Hicks RJ, Maurer T, Eiber M. Prostate-specific membrane antigen PET: clinical utility in prostate cancer, normal patterns, pearls, and pitfalls. Radiographics. 2018;38:200–17. https://doi.org/10.1148/rg.2018170108.
Hofman MS, Violet J, Hicks RJ, Ferdinandus J, Thang SP, Akhurst T, et al. [(177)Lu]-PSMA-617 radionuclide treatment in patients with metastatic castration-resistant prostate cancer (LuPSMA trial): a single-centre, single-arm, phase 2 study. Lancet Oncol. 2018;19:825–33. https://doi.org/10.1016/S1470-2045(18)30198-0.
Fendler WP, Reinhardt S, Ilhan H, Delker A, Boning G, Gildehaus FJ, et al. Preliminary experience with dosimetry, response and patient reported outcome after 177Lu-PSMA-617 therapy for metastatic castration-resistant prostate cancer. Oncotarget. 2017;8:3581–90. https://doi.org/10.18632/oncotarget.12240.
Pillarsetty N, Kalidindi T, Carlin S, Easwaramoorthy B, Abbasi A, Larson S, et al. Effect of specific activity on the uptake of 68Ga -DKFZ-PSMA11 in tumor and other organs. J Nucl Med. 2016;57:2.
Ahad A, Easwaroorthy B, Zhang HW, Pillarsetty N, Alidindi T, Punzalan B, et al. Cyclotron produced Ga-68 for PET imaging of prostate cancer. J Nucl Med. 2018;59:2.
Sartor AO, Morris MJ, Krause BJ. VISION: An international, prospective, open-label, multicenter, randomized phase 3 study of 177Lu-PSMA-617 in the treatment of patients with progressive PSMA-positive metastatic castration-resistant prostate cancer (mCRPC). J Clin Oncol. 2019;37:TPS5099-TPS. https://doi.org/10.1200/JCO.2019.37.15_suppl.TPS5099.
Sathekge M, Bruchertseifer F, Knoesen O, Reyneke F, Lawal I, Lengana T, et al. (225)Ac-PSMA-617 in chemotherapy-naive patients with advanced prostate cancer: a pilot study. Eur J Nucl Med Mol Imaging. 2019;46:129–38. https://doi.org/10.1007/s00259-018-4167-0.
Kratochwil C, Bruchertseifer F, Giesel FL, Weis M, Verburg FA, Mottaghy F, et al. 225Ac-PSMA-617 for PSMA-targeted a-radiation therapy of metastatic castration-resistant prostate cancer. J Nucl Med. 2016;57:1941–4. https://doi.org/10.2967/jnumed.116.178673.
Assadi M, Rezaei S, Jafari E, Rekabpour SJ, Ravanbod MR, Zohrabi F, et al. Potential application of lutetium-177-labeled prostate-specific membrane antigen-617 radioligand therapy for metastatic castration-resistant prostate cancer in a limited resource environment: Initial clinical experience after 2 years. World J Nucl Med. 2020;19:15–20. https://doi.org/10.4103/wjnm.WJNM_20_19.
Rousseau E, Lau J, Kuo HT, Zhang Z, Merkens H, Hundal-Jabal N, et al. Monosodium glutamate reduces (68)Ga-PSMA-11 uptake in salivary glands and kidneys in a preclinical prostate cancer model. J Nucl Med. 2018;59:1865–8. https://doi.org/10.2967/jnumed.118.215350.
Rathke H, Kratochwil C, Hohenberger R, Giesel FL, Bruchertseifer F, Flechsig P, et al. Initial clinical experience performing sialendoscopy for salivary gland protection in patients undergoing (225)Ac-PSMA-617 RLT. Eur J Nucl Med Mol Imaging. 2019;46:139–47. https://doi.org/10.1007/s00259-018-4135-8.
Yilmaz B, Nisli S, Ergul N, Gursu RU, Acikgoz O, Cermik TF. Effect of external cooling on (177)Lu-PSMA uptake by the parotid glands. J Nucl Med. 2019;60:1388–93. https://doi.org/10.2967/jnumed.119.226449.
Kalidindi TM, Lee SG, Punzalan B, Veach D, Jou K, Chakraborty G, et al. Effect of reducing specific activity of [177Lu]-DKFZ-PSMA617 on uptake in the tumor, salivary gland and kidney. J Nucl Med. 2020;61:230.
Zang J, Fan X, Wang H, Liu Q, Wang J, Li H, et al. First-in-human study of (177)Lu-EB-PSMA-617 in patients with metastatic castration-resistant prostate cancer. Eur J Nucl Med Mol Imaging. 2019;46:148–58. https://doi.org/10.1007/s00259-018-4096-y.
Heck MM, Tauber R, Schwaiger S, Retz M, D’Alessandria C, Maurer T, et al. Treatment outcome, toxicity, and predictive factors for radioligand therapy with (177)Lu-PSMA-I&T in metastatic castration-resistant prostate cancer. Eur Urol. 2019;75:920–6. https://doi.org/10.1016/j.eururo.2018.11.016.
Kalidindi TM, Lee S-G, Lewis J, Larson S, Pillarsetty N. Novel radioiodinated theranostic agent targeting PSMA for Prostate cancer. J Nucl Med. 2020;61:383.
Kalidindi TM, Lee S-G, Jou K, Chakraborty G, Skafida M, Tagawa ST, et al. A simple strategy to reduce the salivary gland and kidney uptake of PSMA targeting small molecule radiopharmaceuticals. bioRxiv. 2020. https://doi.org/10.1101/2020.07.24.220277.
Nicolas GP, Mansi R, McDougall L, Kaufmann J, Bouterfa H, Wild D, et al. Biodistribution, pharmacokinetics, and dosimetry of (177)Lu-, (90)Y-, and (111)In-labeled somatostatin receptor antagonist OPS201 in comparison to the agonist (177)Lu-DOTATATE: the mass effect. J Nucl Med. 2017;58:1435–41. https://doi.org/10.2967/jnumed.117.191684.
Moroz A, Lee CY, Wang YH, Hsiao JC, Sevillano N, Truillet C, et al. A preclinical assessment of (89)Zr-atezolizumab identifies a requirement for carrier added formulations not observed with (89)Zr-C4. Bioconjug Chem. 2018;29:3476–82. https://doi.org/10.1021/acs.bioconjchem.8b00632.
Meibohm B, Zhou H. Characterizing the impact of renal impairment on the clinical pharmacology of biologics. J Clin Pharmacol. 2012;52:54S–62S. https://doi.org/10.1177/0091270011413894.
Funding
This study was financially supported by NIH/NCI R01CA207645-0 (JO, NP), DoD PCRP Idea Award W81XWH-19-1-0536 (NP), and NIH/NCI R35 CA232130 (JSL) grants. Technical and facility services provided by the Center of Comparative Medicine & Pathology were supported in part by NIH Grant P30 CA008748. Dr. Chakraborty is supported by PCF young investigator award.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
Dr. Tagawa has served as a consultant for Endocyte and Advanced Accelerator Applications/Novartis and has received institutional research funding from Advanced Accelerator Applications/Novartis. Cornell University holds the intellectual rights for anti-PSMA antibody technology invented by Dr. Bander, that has have been licensed to BZL Biologics, LLC. NB holds equity in BZL biologics and Telix Pharmaceuticals (also serves as uncompensated SAB). All other authors declare no conflict of interest.
Ethical approval
All animal studies were approved by MSKCC-IACUC that ensures that all international, national, and institutional guidelines for the care and use of animals were followed. This study does not contain any studies with human participants.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Translational research
Rights and permissions
About this article
Cite this article
Kalidindi, T.M., Lee, SG., Jou, K. et al. A simple strategy to reduce the salivary gland and kidney uptake of PSMA-targeting small molecule radiopharmaceuticals. Eur J Nucl Med Mol Imaging 48, 2642–2651 (2021). https://doi.org/10.1007/s00259-020-05150-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-020-05150-w