Abstract
Purpose
According to the ACRIN 6668/RTOG 0235 trial, pretreatment metabolic tumour volume (MTV) as detected by 18F-fluorodeoxyglucose PET/CT is a prognostic factor in patients with stage III non-small-cell lung cancer (NSCLC) after definitive radiochemotherapy (RCT). To validate the prognostic value of MTV in patients with stage III NSCLC after RCT, we analysed mature survival data from the German phase III trial ESPATUE.
Methods
This analysis included patients who were staged by PET/CT and who were enrolled in the ESPATUE trial, a randomized study comparing definitive RCT (arm A) with surgery (arm B) after induction chemotherapy and RCT in patients with resectable stage IIIA/IIIB NSCLC. Patients refusing surgery and those with nonresectable disease were scheduled to receive definitive RCT. MTV was measured using a fixed threshold-based approach and a model-based iterative volume thresholding approach. Data were analysed using proportional hazards models and Kaplan-Meier survival functions.
Results
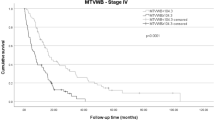
MTV as a continuous variable did not reveal differences in survival between the 117 patients scheduled to receive definitive RCT and all 169 enrolled patients who underwent pretreatment PET/CT (p > 0.5). Five-year survival rates were 33% (95% CI 17–49%) in patients scheduled for definitive RCT with a high MTV (>95.4 ml) and 32% (95% CI: 22–42%) in those with a low MTV. The hazard ratio for survival was 0.997 (95% CI 0.973–1.022) per 10-ml increase in MTV and the slope was significantly shallower than that in the ACRIN 6668/RTOG 0235 trial (random effects model, p = 0.002). There were no differences in MTV size distributions between the ACRIN and ESPATUE trials (p = 0.97).
Conclusion
Patients with stage III NSCLC and a large MTV in whom definitive RCT had a particularly good survival in the ESPATUE trial. Treatment individualization according to MTV is not supported by this study. The ESPATUE and ACRIN trials differed by the use of cisplatin-containing induction chemotherapy and an intensified radiotherapy regimen that were particularly effective in patients with large MTV disease.



Similar content being viewed by others
References
Chee KG, Nguyen DV, Brown M, Gandara DR, Wun T, Lara PN Jr. Positron emission tomography and improved survival in patients with lung cancer: the Will Rogers phenomenon revisited. Arch Intern Med. 2008;168:1541–9.
Ohri N, Duan F, Machtay M, Gorelick JJ, Snyder BS, Alavi A, et al. Pretreatment FDG-PET metrics in stage III non-small cell lung cancer: ACRIN 6668/RTOG 0235. J Natl Cancer Inst. 2015;107(4). https://doi.org/10.1093/jnci/djv004.
Bazan JG, Duan F, Snyder BS, Horng D, Graves EE, Siegel BA, et al. Metabolic tumor volume predicts overall survival and local control in patients with stage III non-small cell lung cancer treated in ACRIN 6668/RTOG0235. Eur J Nucl Med Mol Imaging. 2017;44:17–24.
Salavati A, Duan F, Snyder BS, Wei B, Houshmand S, Khiewvan B, et al. Optimal FDG PET/CT volumetric parameters for risk stratification in patients with locally advanced non-small cell lung cancer: results from the ACRIN 6668/RTOG 0235 trial. Eur J Nucl Med Mol Biol. 2017;44:1969–83.
Bradley JD, Hu C, Komaki RU, Masters G, Blumenschein GR, Schild SE, et al. Long-term results of RTOG 0617: a randomized phase 3 comparison of standard dose versus high dose conformal chemoradiation therapy +/− cetuximab for stage III NSCLC. Int J Radiat Oncol Biol Phys. 2017;99(Suppl):S105.
Eberhardt WE, Pöttgen C, Gauler TC, Friedel G, Veit S, Heinrich V, et al. Phase III study of surgery versus definitive concurrent chemoradiotherapy boost in patients with resectable stage IIIA(N2) and selected IIIB non-small-cell lung cancer after induction chemotherapy and concurrent chemoradiotherapy (ESPATUE). J Clin Oncol. 2015;33:4194–201.
Senan S, Brade A, Wang LH, Vansteenkiste J, Dakhil S, Biesma B, et al. PROCLAIM: randomized phase III trial of pemetrexed-cisplatin or etoposide-cisplatin plus thoracic radiation therapy followed by consolidation chemotherapy in locally advanced nonsquamous non-small-cell lung cancer. J Clin Oncol. 2016;34:953–62.
Goeckenjan G, Sitter H, Thomas M, Branscheid D, Flentje M, Griesinger F, et al. Prevention, diagnosis, therapy, and follow-up of lung cancer: interdisciplinary guideline of the German Respiratory Society and the German Cancer Society. Pneumologie. 2011;65:39–59.
Pöttgen C, Eberhardt W, Stamatis G, Stuschke M. Definitive radiochemotherapy versus surgery within multimodality treatment in stage III non-small cell lung cancer (NSCLC) – a cumulative meta-analysis of the randomized evidence. Oncotarget. 2017;8:41670–8.
Patel AP, Crabtree TD, Bell JM, Guthrie TJ, Robinson CG, Morgensztern D, et al. National patterns of care and outcomes after combined modality therapy for stage IIIA non-small-cell lung cancer. J Thorac Oncol. 2014;9:612–21.
www.onkozert.de/aktuelles_180309.htm. Accessed 19 January 2019.
Rami-Porta R, Bolejack V, Crowley J, Ball D, Kim J, Lyons G, et al. The IASLC Lung Cancer Staging Project: proposals for the revisions of the T descriptors in the forthcoming eighth edition of the TNM classification for lung cancer. J Thorac Oncol. 2015;10:990–1003.
Chiang A, Thibault I, Warner A, Rodrigues G, Palma D, Soliman H, et al. A comparison between accelerated hypofractionation and stereotactic ablative radiotherapy (SABR) for early-stage non-small cell lung cancer (NSCLC): results of a propensity score-matched analysis. Radiother Oncol. 2016;118:478–84.
Pöttgen C, Gauler T, Bellendorf A, Guberina M, Bockisch A, Schwenzer N, et al. Standardized uptake decrease on [18F]-fluorodeoxyglucose positron emission tomography after neoadjuvant chemotherapy is a prognostic classifier for long-term outcome after multimodality treatment: secondary analysis of a randomized trial for resectable stage IIIA/B non-small-cell lung cancer. J Clin Oncol. 2016;34:2526–33.
Erdi YE, Mawlawi O, Larson SM, Imbriaco M, Yeung H, Finn R, et al. Segmentation of lung lesion volume by adaptive positron emission tomography image thresholding. Cancer. 1997;80(12 Suppl):2505–9.
Jentzen W. An improved iterative thresholding method to delineate PET volumes using the delineation-averaged signal instead of the enclosed maximum signal. J Nucl Med Technol. 2015;43:28–35.
Machtay M, Duan F, Siegel BA, Snyder BS, Gorelick JJ, Reddin JS, et al. Prediction of survival by [18F]fluorodeoxyglucose positron emission tomography in patients with locally advanced non-small-cell lung cancer undergoing definitive chemoradiation therapy: results of the ACRIN 6668/RTOG 0235 trial. J Clin Oncol. 2013;31(30):3823–30.
Faraggi D, Simon R. A simulation study of cross-validation for selecting an optimal cutpoint in univariate survival analysis. Stat Med. 1996;15:2203–13.
Schwarzer G, Carpenter JR, Rücker G. Meta-analysis with R (use-R!). Heidelberg: Springer; 2015.
Cheebsumon P, Boellaard R, de Ruysscher D, van Elmpt W, van Baardwijk A, Yaqub M, et al. Assessment of tumour size in PET/CT lung cancer studies: PET- and CT-based methods compared to pathology. EJNMMI Res. 2012;2:56.
Koo TR, Moon SH, Lim YJ, Kim JY, Kim Y, Kim TH, et al. The effect of tumor volume and its change on survival in stage III non-small cell lung cancer treated with definitive concurrent chemoradiotherapy. Radiat Oncol. 2014;9:283.
Warner A, Dahele M, Hu B, Palma DA, Senan S, Oberije C, et al. Factors associated with early mortality in patients treated with concurrent chemoradiation therapy for locally advanced non-small cell lung cancer. Int J Radiat Oncol Biol Phys. 2015;94:612–20.
Stinchcombe TE, Morris DE, Moore DT, Bechtel JH, Halle JS, Mears A, et al. Post-chemotherapy gross tumor volume is predictive of survival in patients with stage III non-small cell lung cancer treated with combined modality therapy. Lung Cancer. 2006;52:67–74.
Ahmed I, Ferro A, Baby R, Malhotra J, Cohler A, Langenfeld J, et al. Modern induction chemotherapy before chemoradiation for bulky locally-advanced nonsmall cell lung cancer improves survival. J Cancer Res Ther. 2016;12:952–8.
Belani CP, Choy H, Bonomi P, Scott C, Travis P, Haluschak J, et al. Combined chemoradiotherapy regimens of paclitaxel and carboplatin for locally advanced non-small-cell lung cancer: a randomized phase II locally advanced multi-modality protocol. J Clin Oncol. 2005;23:5883–91.
Vokes EE, Herndon JE 2nd, Kelley MJ, Cicchetti MG, Ramnath N, Neill H, et al. Induction chemotherapy followed by chemoradiotherapy compared with chemoradiotherapy alone for regionally advanced unresectable stage III non-small-cell lung cancer: Cancer and Leukemia Group B. J Clin Oncol. 2007;25:1698–704.
Saber A, Hiltermann TJN, Kok K, Terpstra MM, de Lange K, Timens W, et al. Mutation patterns in small cell and non-small cell lung cancer patients suggest a different level of heterogeneity between primary and metastatic tumors. Carcinogenesis. 2017;38:144–51.
Jamal-Hanjani M, Wilson GA, McGranahan N, Birkbak NJ, Watkins TBK, Veeriah S, et al. Tracking the evolution of non-small-cell lung cancer. N Engl J Med. 2017;376:2109–21.
Even AJG, Reymen B, La Fontaine MD, Das M, Mottaghy FM, Belderbos JSA, et al. Clustering of multi-parametric functional imaging to identify high-risk subvolumes in non-small cell lung cancer. Radiother Oncol. 2017;125:379–84.
Wu J, Gensheimer MF, Dong X, Rubin DL, Napel S, Diehn M, et al. Robust intratumor partitioning to identify high-risk subregions in lung cancer: a pilot study. Int J Radiat Oncol Biol Phys. 2016;95:1504–12.
Pöttgen C, Stuschke M, Graupner B, Theegarten D, Gauler T, Jendrossek V, et al. Prognostic model for long-term survival of locally advanced non-small-cell lung cancer patients after neoadjuvant radiochemotherapy and resection integrating clinical and histopathologic factors. BMC Cancer. 2015;15:363.
Conant RC, Ashby WR. Every good regulator of a system must be a model of that system. Int J Syst Sci. 1970;1:89–97.
Bensch F, van der Veen EL, Lub-de Hooge MN, Jorritsma-Smit A, Boellaard R, Kok IC, et al. 89Zr-atezolizumab imaging as a non-invasive approach to assess clinical response to PD-L1 blockade in cancer. Nat Med. 2018;24:1852–8.
Huang W, Fan M, Liu B, Fu Z, Zhou T, Zhang Z, et al. Value of metabolic tumor volume on repeated 18F-FDG PET/CT for early prediction of survival in locally advanced non-small cell lung cancer treated with concurrent chemoradiotherapy. J Nucl Med. 2014;55:1584–90.
Funding
The ESPATUE trial was supported by grant no. 70-3070-Eb from German Cancer Aid. The West German Cancer Center at University Hospital Essen is supported by the Oncology Centre of Excellence Program of German Cancer Aid (grant no. 110534) and by the German Federal and State governments via the German Cancer Consortium (DKTK).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
W. Eberhardt received honoraria from Eli Lilly, Boehringer Ingelheim, Pfizer, Novartis, Roche, Merck, Bristol-Myers Squibb, Amgen, GlaxoSmithKline, Aestellas, Bayer, Teva, Merck Serono, Daichi Sankyo and Hexal, and is a consultand or advisor to Eli Lilly, Boehringer Ingelheim, Novartis, Pfizer, Roche, Merck, Bristol-Myers Squibb, Aestellas, Bayer, Teva, Daichi Sankyo. Research Funding and Eli Lilly (Inst).
T. Gauler received Honoraria from Eli Lilly, Boehringer Ingelheim, Merck Serono, Novartis, Roche, Pfizer, Bayer, MSD Oncology, Bristol-Myers Squibb, Symphogen and GlaxoSmithKline, is a consultand or advisor to MSD Oncology, Merck Serono, Novartis, and Eli Lilly, and received travel, accommodation and other expenses from Boehringer Ingelheim and Merck Serono.
M. Schuler received honoraria from Alexion Pharmaceuticals, Boehringer Ingelheim, Celgene, GlaxoSmithKline, Eli Lilly, Novartis and Pfizer, is a consultant or advisor to AstraZeneca, Boehringer Ingelheim, Celgene, Bristol-Myers Squibb, Novartis, IQWiG and Eli Lilly, and received research funding from Boehringer Ingelheim (Inst), Novartis (Inst) and Bristol-Myers Squibb (Inst). Patents, Royalties, Other intellectual property: patents (University Hospital Essen).
D. Theegarten is an advisory board member of E. Lilly.
C. Pöttgen received honoraria from Roche Pharma and Boehringer Ingelheim (speakers bureau).
All other authors declare no conflicts of interest.
Ethical approval
All procedures performed were in accordance with the ethical standards of the institutional research committee and with the principles of the 1964 Declaration of Helsinki and its later amendments. This secondary analysis was approved by the lead ethics committee of the Medical Faculty of the University Duisburg-Essen in September 2016.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Guberina, M., Eberhardt, W., Stuschke, M. et al. Pretreatment metabolic tumour volume in stage IIIA/B non-small-cell lung cancer uncovers differences in effectiveness of definitive radiochemotherapy schedules: analysis of the ESPATUE randomized phase 3 trial. Eur J Nucl Med Mol Imaging 46, 1439–1447 (2019). https://doi.org/10.1007/s00259-019-4270-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-019-4270-x