Abstract
Background
Recently, semiquantitative time-intensity curve (TIC) analysis based on DCE-MRI and apparent diffusion coefficient (ADC) value-based diffusion-weighted imaging (DWI) were used to improve the diagnostic efficiency when diagnosing parotid tumors (PTs). However, quantitative DCE-MRI biomarkers have not been emphasized previously.
Purpose
To explore the diagnostic efficiency of perfusion parameters alone or in combination based on quantitative DCE-MRI and DWI in the differential diagnosis of PTs.
Methods
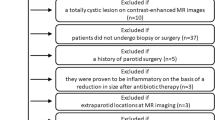
In total, 112 patients with parotid masses were prospectively recruited in our hospital from August 2013 to March 2017. All patients were evaluated with DCE-MRI and DWI before surgery. TIC and quantitative parameters based on DCE MRI and ADCs were analyzed. Receiver operating characteristic analysis and linear discriminant analysis (LDA) was used to determine their diagnostic performance.
Results
In total, 87% (27/31) of pleomorphic adenoma (PA) showed type A TIC, 74% (65/88) of Warthin’s tumors showed type B TIC, and 95% (19/20) of malignant tumors showed TIC type C. Pearson X2 test showed a significant difference between TIC patterns in benign and malignant tumors (X2 = 38.78, p < 0.001). ROC analysis revealed that ADC achieved the best diagnostic performance for distinguishing PA and Warthin’s tumor from others, with area under the curve (AUC) values of 0.945 and 0.925 (p < 0.01), respectively. Furthermore, the TIC type was the only useful biomarker for distinguishing malignant from benign PTs, with an AUC of 0.846 (p < 0.01). Concerning the accuracy of the combined application of multiple parameters of DCE-MRI and ADC values, a combination of TIC pattern and extracellular volume ratio (Ve) provided the best results among five protocols, producing the highest accuracy of 0.75, followed by the combined use of the TIC pattern and ADC (accuracy was 0.70).
Conclusion
TIC pattern in combination with the Ve biomarker based on DCE-MRI could achieve optimal diagnostic accuracy in the differential diagnosis of PTs.






Similar content being viewed by others
Change history
04 February 2020
Figure captions of Figures 2, 3, and 4 were incorrect in the original version of this article.
04 February 2020
Figure captions of Figures��2, 3, and 4 were incorrect in the original version of this article.
References
Xu ZF, Yong F, Yu T, Chen YY, Gao Q, Zhou T, et al. Different histological subtypes of parotid gland tumors: CT findings and diagnostic strategy[J]. World J Radiol. 2013;5(8):313–20. https://doi.org/10.4329/wjr.v5.i8.313.
Xu Z, Rong F, Yu T, Chen YY, Gao Q, Zhou T, et al. Pleomorphic adenoma versus Warthin tumor of the parotid gland: diagnostic value of CT perfusion imaging and its pathologic explanation:CT perfusion of pleomorphic adenoma versus Warthin[J]. J Tumor. 2016;4(2):419–25. https://doi.org/10.17554/j.issn.1819-6187.2016.04.74.
Matsusue E, Fujihara Y, Matsuda E, Tokuyasu Y, Nakamoto S, Nakamura K, et al. Vanishing Parotid Tumors on MR Imaging[J]. Yonago Acta Med. 2018;61(1):33–9 eCollection 2018 Mar. 2018;61:033–039.
Eida S, Sumi M, Nakamura T. Multiparametric magnetic resonance imaging for the differentiation between benign and malignant salivary gland tumors[J]. JMRI. 2010;31:673–9. https://doi.org/10.1002/jmri.22091.
Sumi M, Van Cauteren M, Sumi T, Obara M, Ichikawa Y, Nakamura T. Salivary gland tumors: use of intravoxel incoherent motion MR imaging for assessment of diffusion and perfusion for the differentiation of benign from malignant tumors[J]. Radiology. 2012;263(3):770–7. https://doi.org/10.1148/radiol.12111248.
Kitamoto E, Chikui T, Kawano S, Ohga M, Kobayashi K, Matsuo Y, et al. The application of dynamic contrast-enhanced MRI and diffusion-weighted MRI in patients with maxillofacial tumors[J]. Acad Radiol. 2015;22(2):210–6. https://doi.org/10.1016/j.acra.2014.08.016.
Eissa L, Seif SA, Desooky SE, Eid M, Koraitim T. Accuracy assessment of combined diffusion weighed and dynamic gadolinium MR sequences in characterization of salivary gland tumors[J]. Egypt J Radiol Nucl Med. 2016;47:127–39. https://doi.org/10.1016/j.ejrnm.2015.11.011.
Takashima S, Noguchi Y, Okumura T, Aruga H, Kobayashi T. Dynamic MR imaging in the head and neck[J]. Radiology. 1993;189:813–21. https://doi.org/10.1148/radiology.189.3.8234709.
Zheng SY, Xu ZF, Wu XH, Pan AZ. Use-fullness of dynamic contrast-enhanced MR imaging and diffusion weighted MR imaging for differentiation of benign and malignant parotid tumors[J]. J Clin Med Imag. 2018;1(1):1–6.
Abdel Razek AAK, Samir S, Ashmalla GA. Characterization of parotid tumors with dynamic susceptibility contrast perfusion-weighted magnetic resonance imaging and diffusion-weighted MR imaging[J]. J Comput Assist Tomogr. 2017;41(1):131–6. https://doi.org/10.1097/RCT.0000000000000486.
Yerli H, Agildere AM, Aydin E, Geyik E, Haberal N, Kaskati T, et al. Value of apparent diffusion coefficient calculation in the differential diagnosis of parotid gland tumors[J]. Acta Radiol. 2007;48(9):980–7. https://doi.org/10.1080/02841850701501717.
Yuan Y, Tang W, Tao X. Parotid gland lesions: separate and combined diagnostic value of conventional MRI, diffusion-weighted imaging and dynamic contrast-enhanced MRI[J]. Br J Radiol. 2016;89(1060):20150912. https://doi.org/10.1259/bjr.20150912.
Habermann CR, Arndt C, Graessner J, Diestel L, Petersen KU, Reitmeier F, et al. Diffusion-weighted echo-planar MR imaging of primary parotid gland tumors: is a prediction of different histologic subtypes possible?[J]. AJNR Am J Neuroradiol. 2009;30(3):591–6. https://doi.org/10.3174/ajnr.A1412.
Assili S, Fathi Kazerooni A, Aghaghazvini L, Saligheh Rad HR, Pirayesh Islamian J. Dynamic contrast magnetic resonance imaging (DCE-MRI) and diffusion weighted MR imaging (DWI) for differentiation between benign and malignant salivary gland tumors[J]. J Biomed Phys Eng. 2015;5(4):157–68 eCollection 2015 Dec.
Yabuuchi H, Matsuo Y, Kamitani T, Setoguchi T, Okafuji T, Soeda H, et al. Parotid gland tumors: can addition of diffusion-weighted MR imaging to dynamic contrast-enhanced MR imaging improve diagnostic accuracy in characterization?[J]. Radiology. 2008;249(3):909–16. https://doi.org/10.1148/radiol.2493072045.
Li L, Wang K, Sun X, Wang K, Sun Y, Zhang G, et al. Parameters of dynamic contrast-enhanced MRI as imaging markers for angiogenesis and proliferation in human breast cancer [J]. Med Sci Monit. 2015;21:376–82. https://doi.org/10.12659/MSM.892534.
Tofts PS, Brix G, Buckley DL, Evelhoch JL, Henderson E, Knopp MV, et al. Estimating kinetic parameters from dynamic contrast-enhanced t1-weighted MRI of a diffusable tracer: standardized quantities and symbols[J]. JMRI. 1999;10(3):223–32. https://doi.org/10.1002/(sici)1522-2586(199909)10:3<223:aid-jmri2>3.0.co;2-s.
Ger R, Awan M, Mohamed A, Ding Y, Frank S, Howell R, et al. WE-FG-202-12: investigation of longitudinal salivary gland DCE-MRI changes[J]. Med Phys. 2016;43(6):3829. https://doi.org/10.1118/1.4957924.
Acknowledgments
The authors thank Jin-Yabin from the First People’s Hospital of Foshan for the help in figure editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This prospective study was approved by the institutional review board (Ethics committee of Foshan First People’s Hospital and Ethics Committee of Shantou Central Hospital) and performed between August 2013 and March 2017. Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Oncology—Head and Neck
Rights and permissions
About this article
Cite this article
Xu, Z., Zheng, S., Pan, A. et al. A multiparametric analysis based on DCE-MRI to improve the accuracy of parotid tumor discrimination. Eur J Nucl Med Mol Imaging 46, 2228–2234 (2019). https://doi.org/10.1007/s00259-019-04447-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-019-04447-9