Abstract
Objective
To examine the association between medial meniscal extrusion and structural progression in adults with symptomatic knee osteoarthritis (OA).
Methods
This prospective cohort study examined 176 participants with symptomatic knee OA recruited into a randomised controlled trial. The participants underwent magnetic resonance imaging (MRI) of the study knee at baseline and approximately 2 years later. Meniscal extrusion, tibial cartilage volume, and tibiofemoral bone marrow lesions (BMLs) were measured from MRI using validated methods.
Results
Participants with medial meniscal extrusion ≥ 3 mm had a higher prevalence of lateral tibiofemoral BMLs at baseline (OR = 2.21, 95% CI 1.06–4.61, p = 0.035), and those with medial meniscal extrusion 2–3 mm had a higher likelihood of lateral BML worsening over 2 years (OR = 3.76, 95% CI 1.35–10.52, p = 0.011), compared with those with medial meniscal extrusion < 2 mm. Participants with stable medial meniscal extrusion had a lower likelihood of lateral BML worsening compared with those with regression of medial meniscal extrusion over 2 years (OR = 0.20, 95% CI 0.07–0.56, p = 0.002). There were no associations between medial meniscal extrusion and tibial cartilage volume or medial tibiofemoral BMLs.
Conclusions
Our study showed associations between medial meniscal extrusion and baseline prevalence and worsening over 2 years of lateral tibiofemoral BMLs in people with symptomatic knee OA. Although the reasons for the lack of associations in the medial compartment are not clear, our results suggest a role of medial meniscal extrusion in predicting structural progression in lateral knee OA and that meniscal extrusion might be a potential target in the management of knee OA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Knee osteoarthritis (OA) is the most common chronic joint disease, affecting over 300 million people worldwide [1]. It affects the whole joint and is characterised by progressive cartilage loss accompanied by subchondral bone modelling, synovial proliferation, and deterioration of tendons and ligaments. These structural changes result in pain, stiffness, loss of function, and decreased mobility [2]. In knee OA, the meniscus can undergo degenerative changes, including loss of volume and extrusion.
The medial meniscus is a crescent-shaped fibrocartilage structure which plays a key role in shock absorption, distributing mechanical loads on the articular cartilage and stabilising the knee joint [3]. Meniscal extrusion refers to the displacement of the meniscus beyond the edge of the tibial plateau from its normal position within the knee joint [4], being either partially or totally displaced from the tibial cartilage surface [5]. It is a common finding in individuals with knee OA and has been associated with an increased risk of structural progression in knee OA, evidenced by accelerated cartilage loss and increased bone marrow lesions (BMLs) [6, 7]. The general idea is that a displaced meniscus affects the weight-bearing and load distribution within the knee joint, which results in damage to articular cartilage and subchondral bone, ultimately leading to the development and progression of knee OA [8,9,10]. Previous studies have confirmed the relationship between medial meniscal extrusion and cartilage loss and BMLs in the ipsilateral compartment [9,10,11]. There is evidence from biomechanical analysis that damage of the medial meniscus leads to high deformation and stress on the lateral meniscus, therefore increasing stress application on the cartilages and bone structures [12]. However, no previous studies have investigated whether there is a link between medial meniscal extrusion and cartilage damage and BMLs in the lateral tibiofemoral compartment.
Therefore, the aim of our study was to comprehensively investigate the associations of medial meniscal extrusion and its changes with knee structural progression over 2 years in the medial and lateral compartment separately in a cohort of adults with symptomatic knee OA. It was hypothesised that the presence of medial meniscal extrusion at baseline and its progression over 2 years would be associated with knee structural progression in both medial and lateral compartments.
Methods
Study participants
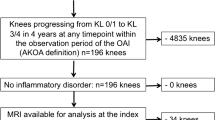
The osteoarthritis of the knee statin (OAKS) study was a randomised controlled trial examining the effect of atorvastatin on the progression of knee OA, with 304 participants recruited in Melbourne, Hobart, and Adelaide, Australia [13, 14]. Eligible participants were aged 40–70 years with symptomatic knee OA which fulfilled the American College of Rheumatology clinical criteria [15] and with a pain score of ≥ 20 mm on a 100-mm visual analogue scale. Participants were excluded if they had severe radiographic knee OA (grade 3 joint space narrowing according to Altman’s atlas [16]); severe knee pain; inflammatory arthritis; significant knee injury; accepted indications for statin therapy; current use of lipid-lowering therapy, or previous adverse reaction to statins; absolute cardiovascular risk estimated using the Framingham risk equation of > 15% within the next 5 years; fasting total cholesterol level > 7.5 mmol/L; clinically significant renal disease or abnormal liver function; arthroscopy or open surgery or intra-articular therapy in the index knee in the last 12 months; concomitant use of potent analgesics including opiates; comorbidity limiting participation; relocation; contraindication to magnetic resonance imaging (MRI) scanning; pregnancy, breastfeeding, or women trying to become pregnant, or inability to give informed consent [13, 14]. The trial was registered with the Australian New Zealand Clinical Trials Registry (ACTRN12613000190707). Ethics approval was obtained from the Alfred Hospital Ethics Committee, Monash University Human Research Ethics Committee, Tasmania Health and Medical Human Research Ethics Committee, and The Queen Elizabeth Hospital Human Research Ethics Committee. Written informed consent was obtained from all the participants. This current study included 176 participants recruited in Melbourne who had coronal MRI performed for meniscal extrusion measurement. Among these participants, 152 underwent a follow-up MRI approximately two years later (Fig. 1).
Knee MRI acquisition
MRI was conducted on the study knee using a 3.0 T whole-body MR unit utilising a commercial 16-channel transmit-receive knee coil (Achieva, Philips Medical Systems). T1-weighted fat-suppressed 3D gradient recall acquisition in a steady state was employed for the measurement of cartilage volume [14]. Proton density fat-saturated acquisition was used to assess bone marrow lesions (sagittal) and meniscal extrusion (coronal) [14]. Details of MRI units, sequences, and parameters have been published previously [14].
Assessment of medial meniscal extrusion
Medial meniscal extrusion was defined as the displacement of the medial meniscus beyond the innermost border of the tibial plateau, as measured through the knee joint in the coronal plane [17]. The coronal plane for meniscal extrusion measurement was defined as the slice with the largest area of the medial tibial spine. If the maximum area of the medial spine could not be distinguished on two consecutive slices, the slice with the widest tibial plateau was selected [18]. If there were bone spurs present, they were excluded from the measurement [19]. Extrusion of the medial meniscal body was assessed using validated methods [20] using the software RadiAnt DICOM Viewer (Fig. 2). The steps of measurement include (1) dropping a perpendicular line at the point of medial tibial plateau transitioning from horizontal to vertical, (2) dropping another perpendicular line intersecting the outermost edge of the medial meniscus, and (3) measuring meniscal extrusion as the distance between the two perpendicular lines in mm. One trained observer performed the measurement in duplicate, with an intra-observer reproducibility (intra-class correlation coefficient) of 0.99, and the average results were taken as the final measure. The grade of medial meniscal extrusion was defined as 0–2: grade 0: extrusion < 2 mm; grade 1: extrusion 2–3 mm; and grade 2: extrusion ≥ 3 mm [6, 21]. The change in medial meniscal extrusion over 2 years was defined as follows: regression (baseline extrusion grade > follow-up extrusion grade), stable (baseline extrusion grade = follow-up extrusion grade), and progression (baseline extrusion grade < follow-up extrusion grade).
Measurement of medial meniscal extrusion. A Baseline MRI; B follow-up MRI of the same participant. Medial meniscal extrusion was measured on the coronal plane at the slice with the largest area of the medial tibial spine with the steps: (1) drop a perpendicular line at the point of medial tibial plateau transitioning from horizontal to vertical; (2) drop another perpendicular line intersecting the outermost edge of the medial meniscus; (3) measure meniscal extrusion as the distance between the two perpendicular lines
Measurement of tibial cartilage volume
Medial and lateral tibial cartilage volume was measured from sagittal T1-weighted images by manually drawing the disarticulation contours around the cartilage boundaries on a section-by-section basis, using the OsiriX software. Two trained observers independently performed the measurement with an inter-observer intraclass correlation coefficient of 0.91, and the average results were taken as the final measure. The annual percentage change in medial and lateral tibial cartilage volume was calculated separately as (follow-up cartilage volume − baseline cartilage volume)/baseline cartilage volume/years between MRI scans*100 [13].
Assessment of bone marrow lesions
BMLs were defined as areas of increased signal intensity adjacent to the subcortical bone in either the distal femur or the proximal tibia [22]. A lesion was identified as being present if it appeared on two or more adjacent slices. BMLs were graded at medial and lateral tibial and femoral sites (0–3) from sagittal proton density images using the MOAKS [23], where grade 0, none; grade 1, < 33% of subregion; grade 2, 33–66% of subregion; grade 3, > 66% of subregion (Fig. 3). One trained observer performed the measurement, with random cross-check performed by a second observer independently, with intra- and inter-reader intraclass correlation coefficients of 0.88–0.93 [13]. The discrepancy in grading was solved by a discussion between the two observers. The prevalence of BMLs was defined as a grade ≥ 1 in either the tibial or femoral site in the medial and lateral compartments. The worsening of BMLs was defined as any increase in grade in either the tibial site or femoral site over 2 years in the medial and lateral compartments.
Tibial bone area measurement
The cross-sectional areas of the medial and lateral tibial plateau were measured from axial images as previously described [24]. The coefficients of variation for the medial and lateral tibial plateau areas were 2.3% and 2.4%, respectively [24].
Anthropometric measurements
At baseline, height (stadiometer) and weight (electric scale) were measured, and body mass index (BMI, height/weight2) was calculated.
Statistical analyses
With 176 participants, the current study had 80% power to detect a correlation coefficient as low as 0.21 between meniscal extrusion and knee structural progression, alpha 0.05, two-sided significance. Participant characteristics were tabulated and compared among participants with grade 0, 1, and 2 medial meniscal extrusion using analysis of variance (ANOVA) and chi-square test, when appropriate. The differences in medial and lateral tibial cartilage volume at baseline or annual percentage change in medial and lateral tibial cartilage volume among participants with grade 0, 1, and 2 medial meniscal extrusion were examined using F-test (general linear model) with estimated marginal means. The analyses were adjusted for age, sex, BMI, and baseline tibial plateau bone area, with the analysis of annual percentage change in cartilage volume additionally adjusted for randomisation group allocation (atorvastatin/placebo). The associations between medial meniscal extrusion and the prevalence of medial and lateral tibiofemoral BMLs were examined using binary logistic regression, adjusting for age, sex, and BMI. The associations between medial meniscal extrusion and worsening of medial and lateral tibiofemoral BMLs were also examined using binary logistic regression, adjusting for age, sex, BMI, randomisation group allocation, and baseline BML score. Given the association between lateral meniscal lesion and BMLs in the lateral compartment [9], additional adjustment for lateral meniscal extrusion was performed in the analysis of the association between medial meniscal extrusion and BMLs in the lateral compartment. P-values of less than 0.05 were considered statistically significant. All analyses were performed using the SPSS statistical package (standard version 28, SPSS, USA).
Results
Characteristics of study participants are presented in Table 1. Medial meniscal extrusion was measured in 174 participants, but not measurable for 2 participants as no coronal images (Fig. 1). The current study included 174 participants, 81 (46.5%) with grade 0 meniscal extrusion, 41 (23.6%) with grade 1 and 52 (29.9%) with grade 2 meniscal extrusion. The prevalence of lateral tibiofemoral BMLs was different among the three groups, which was higher in participants with grade 2 medical extrusion compared with the other two groups. There were no significant differences among the three groups in other characteristics.
The associations between medial meniscal extrusion and knee structure at baseline are summarized in Table 2. There were no significant associations between medial meniscal extrusion grade and medial tibial cartilage volume or the prevalence of medial tibiofemoral BMLs in univariable or multivariable analyses. The univariable analysis showed a higher prevalence of lateral tibiofemoral BMLs in participants with grade 2 medial meniscal extrusion compared with those with grade 0 medial meniscal extrusion, which persisted in multivariable analysis adjusted for age, sex, and BMI (odds ratio (OR) 2.21, 95% confidence interval (CI) 1.06–4.61), or with additional adjustment for lateral meniscal extrusion (OR 2.26, 95% CI 1.08–4.74, p = 0.031). There was no significant association between medial meniscal extrusion grade and lateral tibial cartilage volume in univariable or multivariable analysis.
The associations between medial meniscal extrusion at baseline and changes in knee structure over 2 years are presented in Table 3. Worsening of BMLs was observed in 66/150 (44.0%) participants for the medial compartment and 34/150 (22.7%) participants for the lateral compartment. There was no significant association between medial meniscal extrusion grade and annual percentage change in medial tibial cartilage volume, annual percentage change in lateral tibial cartilage volume, or medial BML worsening, in either univariable or multivariable analyses. In univariable analysis, there was a higher likelihood of lateral BML worsening in participants with grade 1 medial meniscal extrusion compared with those with grade 0 medial meniscal extrusion, which persisted in multivariable analysis adjusted for age, sex, BMI, randomisation group allocation, and baseline BML score (OR 3.76, 95% CI 1.35–10.52), or with additional adjustment for lateral meniscal extrusion (OR 3.84, 95% CI 1.37–10.80, p = 0.011).
In terms of the change in medial meniscal extrusion, regression was observed in 14.2% of the participants, stable extrusion in 55.1%, and progression in 14.2% of the participants. The associations between changes in medial meniscal extrusion grade and changes in knee structure over 2 years are shown in Table 4. There was no significant association between change in medial meniscal extrusion grade and annual percentage change in medial tibial cartilage volume, annual percentage change in lateral tibial cartilage volume, or medial BML worsening, in either univariable or multivariable analyses. In the univariable analysis, there was a lower likelihood of lateral BML worsening in participants with stable medial meniscal extrusion compared with those with regressed medial meniscal extrusion. The significant association persisted in multivariable analysis adjusted for age, sex, BMI, randomisation group allocation, and baseline BML score (OR 0.20, 95% CI 0.07–0.56), or with additional adjustment for lateral meniscal extrusion (OR 0.15, 95% CI 0.05–0.47, p = 0.001).
Discussion
Our prospective cohort study showed associations between medial meniscal extrusion and BMLs in the lateral tibiofemoral compartment in individuals with symptomatic knee OA. Cross-sectionally, participants with severe medial meniscal extrusion (grade 2, ≥ 3 mm) had a higher prevalence of lateral tibiofemoral BMLs compared with those with grade 0 extrusion (< 2 mm) at baseline. Longitudinally, a higher likelihood of lateral BML worsening over 2 years was observed in participants with grade 1 medial meniscal extrusion (2–3 mm) compared with those with grade 0 extrusion at baseline. Moreover, participants with stable medial meniscal extrusion over 2 years had a lower likelihood of lateral BML worsening over 2 years compared with those with regressed medial meniscal extrusion.
The associations between medial meniscal extrusion and the development and progression of knee OA, as well as structural progression in the medial compartment, have been examined, showing consistent results [9,10,11]. In the current study, we found associations between baseline medial meniscal extrusion and the prevalence and worsening of BMLs in the lateral tibiofemoral compartment, with no significant associations observed for BMLs in the medial compartment. BMLs are commonly associated with knee OA, being associated with knee pain and cartilage loss, and predictive of total knee replacement [25,26,27]. BMLs are affected by joint loading and the response of joint tissues to this abnormal biomechanical stress, as well as systematic factors [28, 29]. BML is not a static phenomenon but changes over time, and the natural history of BMLs varies in individuals with knee OA [30,31,32]. In our study, worsening of BMLs in the medial and lateral compartment over 2 years was observed in 44.0% and 22.7% of participants, respectively. An increase in BML size has been shown to be associated with increased knee pain and progressive cartilage loss [33, 34]. Previous studies have shown the relationship between medial meniscal extrusion and BMLs in the medial tibiofemoral compartment [9, 10] with no studies examining whether there is a link between medial meniscal extrusion and lateral BMLs. Biomechanical analysis has demonstrated increased deformation and stress on the lateral meniscus as a result of damage to the medial meniscus, which increased the stress on the cartilage and bone of the lateral compartment [12]. It is biologically plausible that medial meniscal extrusion would lead to structural damage in the lateral tibiofemoral compartment. To our knowledge, our study is the first to report consistent associations between medial meniscal extrusion and the prevalence and worsening of lateral tibiofemoral BMLs in both cross-sectional and longitudinal analyses. Our study also adds to the existing literature by exploring the association between changes in medial meniscal extrusion and changes in knee structural outcomes over 2 years, showing an increased likelihood of lateral BML worsening in participants with regressed medial meniscal extrusion compared with those with stable meniscal extrusion. The potential mechanism behind this link is unknown but may relate to the altered biomechanics and increased contact pressure on the lateral tibiofemoral joint surfaces attributable to the severity and/or change in medial meniscal extrusion, which may cause BMLs. Compared with stable medial meniscal extrusion over 2 years, regression in medial meniscal extrusion may cause varus thrust with tibial spine impingement on the lateral femoral condyle under axial load, which might change the biomechanics of the lateral compartment and provide a potential explanation for the increased likelihood of BML worsening in that compartment. The relationship between meniscal extrusion and structural progression in the contralateral compartment warrants further investigation.
In contrast to previous studies [7, 11], our study found no association between medial meniscal extrusion and medial tibial cartilage volume or medial tibiofemoral BMLs. This might be due to different study populations or different methods for assessment of meniscal extrusion. It might suggest that the potential mechanism behind these structural changes in knee OA may not be directly related to medial meniscal extrusion. It may be that the effect of meniscal extrusion is less apparent in more severe OA. As participants in this study tended to have more severe OA in the medial than the lateral compartment, it may be that other factors including other biomechanical factors play a more significant role in the structural progression of the medial compartment. Further research is needed to better understand the complex interplay of biomechanical and systemic factors that contribute to the structural progression of knee OA.
There are some limitations that should be considered. Firstly, meniscal extrusion might be underestimated on supine MRI scans [35], which may not accurately reflect the prevalence of meniscal extrusion during usual activities. Most of the participants in our study had mild to moderate knee OA [13], so the findings may not be generalisable to healthy individuals without knee OA or patients with severe disease. We examined changes in meniscal extrusion, cartilage volume, and BMLs over a 2-year period. It is unclear whether changes in meniscal extrusion cause changes in cartilage and BMLs, or vice versa, which limits the ability to establish causality. The relationship between these variables is complex and requires further investigation to establish causality. Femorotibial alignment, which might be a covariate for the association between meniscal extrusion and structural progression, in particular BMLs, was not measured in the current study. Meniscal root tear, which is associated with meniscal extrusion and structural progression in knee OA, was not measured in our study. Whether the association between meniscal extrusion and structural progression is mediated by meniscal tears warrants further investigation. Further studies of larger sample size and/or with longer follow-up are needed to better understand the relationship between meniscal extrusion and structural progression in knee OA. The strength of the study was the investigation of association between medial meniscal extrusion and structural progression in the medial and lateral tibiofemoral compartment separately and the examination of changes in meniscal extrusion over 2 years. There were consistent associations between medial meniscal extrusion and lateral tibiofemoral BMLs in both cross-sectional and longitudinal analyses, strengthening our findings. Since knee OA is a progressive disease, understanding the role of modifiable factors, such as meniscal extrusion, in structural progression may have the potential to inform therapeutic strategies.
Conclusions
Our study demonstrated associations between medial meniscal extrusion and baseline prevalence and worsening over 2 years of BMLs in the lateral tibiofemoral compartment in individuals with symptomatic knee OA. The results suggest that medial meniscal extrusion may be a predictor of structural progression in knee OA, in particular worsening of BMLs in the lateral tibiofemoral compartment. These findings have implications for better understanding the pathogenesis of knee OA and identifying potential targets for disease prevention and treatment.
Data availability
The data generated from this study will not be deposited in a public repository due to privacy and consent restrictions. Deidentified data can be made available from the corresponding author on reasonable request, subject to a data-sharing agreement.
References
Al-Mhanna SB, Mohamed M, Mohd Noor N, Aldhahi MI, Afolabi HA, Mutalub YB, et al. Effects of circuit training on patients with knee osteoarthritis: a systematic review and meta-analysis. Healthcare (Basel). 2022;10(10):2041.
He Y, Li Z, Alexander PG, Ocasio-Nieves BD, Yocum L, Lin H, et al. Pathogenesis of osteoarthritis: risk factors, regulatory pathways in chondrocytes, and experimental models. Biology (Basel). 2020;9(8):194.
Walker PS, Erkman MJ. The role of the menisci in force transmission across the knee. Clin Orthop Relat Res. 1975;109:184–92.
Papalia GF, Za P, Saccone L, Franceschetti E, Zampogna B, Vasta S, et al. Meniscal extrusion: risk factors and diagnostic tools to predict early osteoarthritis. Orthop Rev (Pavia). 2023;15:74881.
Xu D, van der Voet J, Waarsing JH, Oei EH, Klein S, Englund M, et al. Are changes in meniscus volume and extrusion associated to knee osteoarthritis development? A structural equation model. Osteoarthritis Cartilage / OARS Osteoarthr Res Soc. 2021;29(10):1426–31.
Hunter DJ, Zhang YQ, Niu JB, Tu X, Amin S, Clancy M, et al. The association of meniscal pathologic changes with cartilage loss in symptomatic knee osteoarthritis. Arthritis Rheum. 2006;54(3):795–801.
Antony B, Driban JB, Price LL, Lo GH, Ward RJ, Nevitt M, et al. The relationship between meniscal pathology and osteoarthritis depends on the type of meniscal damage visible on magnetic resonance images: data from the Osteoarthritis Initiative. Osteoarthritis Cartilage. 2017;25(1):76–84.
Englund M, Guermazi A, Roemer FW, Aliabadi P, Yang M, Lewis CE, et al. Meniscal tear in knees without surgery and the development of radiographic osteoarthritis among middle-aged and elderly persons: the multicenter osteoarthritis study. Arthritis Rheum. 2009;60(3):831–9.
Englund M, Guermazi A, Roemer FW, Yang M, Zhang Y, Nevitt MC, et al. Meniscal pathology on MRI increases the risk for both incident and enlarging subchondral bone marrow lesions of the knee: the MOST Study. Ann Rheum Dis. 2010;69(10):1796–802.
Roubille C, Martel-Pelletier J, Raynauld JP, Abram F, Dorais M, Delorme P, et al. Meniscal extrusion promotes knee osteoarthritis structural progression: protective effect of strontium ranelate treatment in a phase III clinical trial. Arthritis Res Ther. 2015;17(1):82.
Wang Y, Wluka AE, Pelletier JP, Martel-Pelletier J, Abram F, Ding C, et al. Meniscal extrusion predicts increases in subchondral bone marrow lesions and bone cysts and expansion of subchondral bone in osteoarthritic knees. Rheumatology (Oxford). 2010;49(5):997–1004.
Li L, Yang X, Yang L, Zhang K, Shi J, Zhu L, et al. Biomechanical analysis of the effect of medial meniscus degenerative and traumatic lesions on the knee joint. Am J Transl Res. 2019;11(2):542–56.
Wang Y, Jones G, Hill C, Wluka AE, Forbes AB, Tonkin A, et al. Effect of atorvastatin on knee cartilage volume in patients with symptomatic knee osteoarthritis: results from a randomized placebo-controlled trial. Arthritis Rheumatol (Hoboken, NJ). 2021;73(11):2035–43.
Wang Y, Tonkin A, Jones G, Hill C, Ding C, Wluka AE, et al. Does statin use have a disease modifying effect in symptomatic knee osteoarthritis? Study protocol for a randomised controlled trial. Trials. 2015;16:584.
Altman R, Asch E, Bloch D, Bole G, Borenstein D, Brandt K, et al. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheum. 1986;29(8):1039–49.
Altman RD, Hochberg M, Murphy WA Jr, Wolfe F, Lequesne M. Atlas of individual radiographic features in osteoarthritis. Osteoarthritis Cartilage / OARS Osteoarthr Res Soc. 1995;3(Suppl A):3–70.
Swamy N, Wadhwa V, Bajaj G, Chhabra A, Pandey T. Medial meniscal extrusion: detection, evaluation and clinical implications. Eur J Radiol. 2018;102:115–24.
Bruns K, Svensson F, Turkiewicz A, Wirth W, Guermazi A, Eckstein F, et al. Meniscus body position and its change over four years in asymptomatic adults: a cohort study using data from the osteoarthritis initiative (OAI). BMC Musculoskelet Disord. 2014;15:32.
Costa CR, Morrison WB, Carrino JA. Medial meniscus extrusion on knee MRI: is extent associated with severity of degeneration or type of tear? AJR Am J Roentgenol. 2004;183(1):17–23.
Furumatsu T, Kintaka K, Higashihara N, Tamura M, Kawada K, Xue H, et al. Meniscus extrusion is a predisposing factor for determining arthroscopic treatments in partial medial meniscus posterior root tears. Knee Surg Relat Res. 2023;35(1):8.
Liu Y, Du G, Li X. Threshold for lateral meniscal body extrusion on MRI in middle-aged and elderly patients with symptomatic knee osteoarthritis. Diagn Interv Imaging. 2020;101(10):677–83.
McAlindon TE, Watt I, McCrae F, Goddard P, Dieppe PA. Magnetic resonance imaging in osteoarthritis of the knee: correlation with radiographic and scintigraphic findings. Ann Rheum Dis. 1991;50(1):14–9.
Hunter DJ, Guermazi A, Lo GH, Grainger AJ, Conaghan PG, Boudreau RM, et al. Evolution of semi-quantitative whole joint assessment of knee OA: MOAKS (MRI Osteoarthritis Knee Score). Osteoarthritis Cartilage. 2011;19(8):990–1002.
Wluka AE, Stuckey S, Snaddon J, Cicuttini FM. The determinants of change in tibial cartilage volume in osteoarthritic knees. Arthritis Rheum. 2002;46(8):2065–72.
Davies-Tuck ML, Wluka AE, Forbes A, Wang Y, English DR, Giles GG, et al. Development of bone marrow lesions is associated with adverse effects on knee cartilage while resolution is associated with improvement–a potential target for prevention of knee osteoarthritis: a longitudinal study. Arthritis Res Ther. 2010;12(1):R10.
Tanamas SK, Wluka AE, Pelletier JP, Pelletier JM, Abram F, Berry PA, et al. Bone marrow lesions in people with knee osteoarthritis predict progression of disease and joint replacement: a longitudinal study. Rheumatology (Oxford). 2010;49(12):2413–9.
Crema MD, Roemer FW, Hayashi D, Guermazi A. Comment on: bone marrow lesions in people with knee osteoarthritis predict progression of disease and joint replacement: a longitudinal study. Rheumatology (Oxford). 2011;50(5):996–7 (author reply 997-999).
Shabestari M, Kise NJ, Landin MA, Sesseng S, Hellund JC, Reseland JE, et al. Enhanced angiogenesis and increased bone turnover characterize bone marrow lesions in osteoarthritis at the base of the thumb. Bone Joint Res. 2018;7(6):406–13.
Segal NA, Kern AM, Anderson DD, Niu J, Lynch J, Guermazi A, et al. Elevated tibiofemoral articular contact stress predicts risk for bone marrow lesions and cartilage damage at 30 months. Osteoarthritis Cartilage. 2012;20(10):1120–6.
Brem MH, Schlechtweg PM, Bhagwat J, Genovese M, Dillingham MF, Yoshioka H, et al. Longitudinal evaluation of the occurrence of MRI-detectable bone marrow edema in osteoarthritis of the knee. Acta Radiol. 2008;49(9):1031–7.
Roemer FW, Guermazi A, Javaid MK, Lynch JA, Niu J, Zhang Y, et al. Change in MRI-detected subchondral bone marrow lesions is associated with cartilage loss: the MOST Study. A longitudinal multicentre study of knee osteoarthritis. Ann Rheum Dis. 2009;68(9):1461–5.
Kornaat PR, Kloppenburg M, Sharma R, Botha-Scheepers SA, Le Graverand MP, Coene LN, et al. Bone marrow edema-like lesions change in volume in the majority of patients with osteoarthritis; associations with clinical features. Eur Radiol. 2007;17(12):3073–8.
Driban JB, Price L, Lo GH, Pang J, Hunter DJ, Miller E, et al. Evaluation of bone marrow lesion volume as a knee osteoarthritis biomarker–longitudinal relationships with pain and structural changes: data from the osteoarthritis initiative. Arthritis Res Ther. 2013;15(5):R112.
Hunter DJ, Zhang Y, Niu J, Goggins J, Amin S, LaValley MP, et al. Increase in bone marrow lesions associated with cartilage loss: a longitudinal magnetic resonance imaging study of knee osteoarthritis. Arthritis Rheum. 2006;54(5):1529–35.
Gajjar SM, Solanki KP, Shanmugasundaram S, Kambhampati SBS. Meniscal Extrusion: a narrative review. Orthop J Sports Med. 2021;9(11):23259671211043796.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. The study is funded by a project grant from the National Health and Medical Research Council of Australia (NHMRC, APP1048581). FMC is the recipient of the NHMRC Investigator Grant (APP1194829). AEW is the recipient of the Royal Australian College of Physicians Fellows Career Development Fellowship. GJ is the recipient of the NHMRC Practitioner Fellowship. The funder of the study had no role in the study design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This study was obtained from the Alfred Hospital Ethics Committee, Monash University Human Research Ethics Committee, Tasmania Health and Medical Human Research Ethics Committee, and The Queen Elizabeth Hospital Human Research Ethics Committee.
Conflict of interest
GJ received honoraria for talks from BMS, Roche, AbbVie, Amgen, Lilly, Novartis, and Janssen, and a grant for a clinical trial from Covance. The other authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zeng, M., Cicuttini, F.M., Wluka, A.E. et al. Association between medial meniscal extrusion and knee structural progression in adults with symptomatic knee osteoarthritis — a prospective cohort study. Skeletal Radiol (2024). https://doi.org/10.1007/s00256-024-04731-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00256-024-04731-2