Abstract
Objective
To perform a meta-analysis comparing the MRI features of tuberculous and pyogenic spondylitis, using histopathological results and/or blood culture as the standard reference.
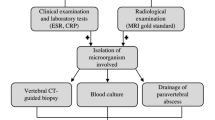
Materials and methods
PubMed, Embase, Web of Science, and Cochrane Library were searched for English-language studies on the MRI features of tuberculous and pyogenic spondylitis published between January 2010 and February 2023. Risk for bias and concerns regarding applicability were assessed using the Quality Assessment of Diagnostic Accuracy Studies-2 tool. Pooled MRI features’ proportions were calculated using a bivariate random-effects model.
Results
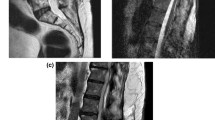
Thirty-two studies met the inclusion criteria: 21 for tuberculous spondylitis, three for pyogenic spondylitis, and eight for both. Of the nine informative MRI features comparing tuberculous spondylitis to pyogenic spondylitis, involvement of ≥ 2 vertebral bodies (92% vs. 88%, P = .004), epidural extension (77% vs. 25%, P < .001), paravertebral collection (91% vs. 84%, P < .001), subligamentous spread (93% vs. 24%, P < .001), thin and regular abscess wall (94% vs. 18%, P < .001), vertebral collapse (68% vs. 24%, P < .001), and kyphosis (39% vs. 3%, P < .01) were more suggestive of tuberculous spondylitis, while disc signal change (82% vs. 95%, P < .001) and disc height loss (22% vs. 59%, P < .001) were more suggestive of pyogenic spondylitis.
Conclusion
Involvement of ≥ 2 vertebral vertebral bodies, soft tissue attribution, thin and regular abscess wall, vertebral collapse, and kyphosis were MRI features more common in tuberculous spondylitis, while disc signal change and height loss were more common in pyogenic spondylitis.





Similar content being viewed by others
Abbreviations
- TbS:
-
Tuberculous Spondylitis
- PyS:
-
Pyogenic Spondylitis
- CI:
-
Confidence interval
- QUADAS:
-
Quality Assessment of Diagnostic Accuracy Studies
- I2 :
-
Inconsistency index
References
Skaf GS, Kanafani ZA, Araj GF, Kanj SS. Non-pyogenic infections of the spine. Int J Antimicrob Agents. 2010;36(2):99–105.
Kumar Y, Gupta N, Chhabra A, Fukuda T, Soni N, Hayashi D. Magnetic resonance imaging of bacterial and tuberculous spondylodiscitis with associated complications and non-infectious spinal pathology mimicking infections: a pictorial review. BMC Musculoskelet Disord. 2017;18(1):244.
Li T, Li W, Du Y, Gao M, Liu YX, Wang GD, et al. Discrimination of pyogenic spondylitis from brucellar spondylitis on MRI. Medicine (Baltimore). 2018;97:e11195.
Lee KY. Comparison of pyogenic spondylitis and tuberculous spondylitis. Asian spine J. 2014;8(2):216–23.
Garg RK, Somvanshi DS. Spinal tuberculosis: a review. J Spinal Cord Med. 2011;34(5):440–54.
Koubaa M, Maaloul I, Marrakchi C, Lahiani D, Hammami B, Mnif Z, et al. Spinal brucellosis in South of Tunisia: review of 32 cases. Spine J. 2014;14(8):1538–44.
Mukherji SK. Spinal infections. Neuroimaging Clin N Am. 2015;25(2):xiii.
Khanna K, Sabharwal S. Spinal tuberculosis: a comprehensive review for the modern spine surgeon. Spine J. 2019;19(11):1858e1870.
Nagashima H, Tanishima S, Tanida A. Diagnosis and management of spinal infections. J Orthop Sci. 2018;23(1):8–13.
Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155(8):529–36.
Altman DG, Bland JM. Interaction revisited: the difference between two estimates. BMJ. 2003;326(7382):219.
Zaidi H, Akram MH, Wala MS. Frequency and magnetic resonance imaging patterns of tuberculous spondylitis lesions in adults. J Coll Physicians Surg Pak. 2010;20(5):303–6.
Wang Q, Babyn P, Branson H, Tran D, Davila J, Mueller EL. Utility of MRI in the follow-up of pyogenic spinal infection in children. Pediatr Radiol. 2010;40(1):118–30.
Khalid M, Siddiqui MA, Qaseem SMD, Mittal S, Iraqi AA, Rizvi SAA. Role of magnetic resonance imaging in evaluation of tubercular spondylitis: pattern of disease in 100 patients with review of literature. JNMA J Nepal Med Assoc. 2011;51(183):116–21.
Park JH, Shin HS, Park JT, Kim TY, Eom KS. Differentiation between tuberculous spondylitis and pyogenic spondylitis on MR imaging. Korean J Spine. 2011;8(4):283–7.
Gehlot PS, Chaturvedi S, Kashyap R, Singh V. Pott’s spine: retrospective analysis of MRI scans of 70 cases. J Clin Diagn Res. 2012;6(9):1534–8.
Jain AK, Sreenivasan R, Saini NS, Kumar S, Jain S, Dhammi IK. Magnetic resonance evaluation of tubercular lesion in spine. Int Orthop. 2012;36(2):261–9.
Sureka J, Samuel S, Keshava SN, Venkatesh K, Sundararaj GD. MRI in patients with tuberculous spondylitis presenting as vertebra plana: a retrospective analysis and review of literature. Clin Radiol. 2013;68(1):e36-42.
Lee SW, Lee SH, Chung HW, Kim MJ, Seo MJ, Shin MJ. Candida spondylitis: comparison of MRI findings with bacterial and tuberculous causes. AJR Am J Roentgenol. 2013;201(4):872–7.
Thammaroj J, Kitkhuandee A, Sawanyawisuth K, Chowchuan P, Promon K. MR findings in spinal tuberculosis in an endemic country. J Med Imaging Radiat. 2014;58(3):267–76.
Hasan NMA. Pedicle involvement in tuberculous spondylitis and pyogenic spondylitis: comparative magnetic resonance imaging study. Egypt J Radiol Nucl Med. 2014;45:455–60.
Thammaroj J, Kitkuandee A, Sawanyawisuth K. Differences of MRI features between tuberculous and bacterial spondylitis in a TB-endemic area. Southeast Asian J Trop Med Public Health. 2015;46(1):71–9.
Galhotra RD, Jain T, Sandhu P, Galhotra V. Utility of magnetic resonance imaging in the differential diagnosis of tubercular and pyogenic spondylodiscitis. J Nat Sci Biol Med. 2015;6(2):388–93.
Sivalingam J, Kumar A. Spinal tuberculosis resembling neoplastic lesions on MRI. J Clin Diagn Res. 2015;9(11):TC01-3.
Li T, Liu T, Jiang Z, Cui X, Sun J. Diagnosing pyogenic, brucella and tuberculous spondylitis using histopathology and MRI: a retrospective study. Exp Ther Med. 2016;12(4):2069–77.
Gao M, Sun JM, Jiang ZS, Cui XG, Liu XY, Wang GD, et al. Comparison of tuberculous and brucellar spondylitis on MRI images. Spine. 2017;42(2):113–21.
Pallewatte AS, Wickramasinghe NA. Magnetic resonance imaging findings of patients with suspected tuberculosis from a tertiary care Centre in Sri Lanka. Ceylon Med J. 2016;61(4):185–8.
Tabassum S, Haider S. Frequency of magnetic resonance imaging patterns of tuberculous spondylitis in a public sector hospital. Pak J Med Sci. 2016;32(1):171–5.
Maurya VK, Sharma P, Ravikumar R, et al. Tubercular spondylitis: a review of MRI findings in 80 cases. Med J Armed Forces India. 2018;74(1):11–7.
Frel M, Białecki J, Wieczorek J, Paluch L, Dąbrowska-Thing A, Walecki J. Magnetic resonance imaging in differentatial diagnosis of pyogenic spondylodiscitis and tuberculous spondylodiscitis. Pol J Radiol. 2017;82:71–87.
Yueniwati Y, Christina E. The challenges in differentiating tuberculous from pyogenic spondylitis using magnetic resonance imaging. Rep Med imaging. 2017;10:37–43.
Lee Y, Kim BJ, Kim SH, Lee SH, Kim WH, Jin SW. Comparative analysis of spontaneous infectious spondylitis: pyogenic versus tuberculous. J Korean Neurosurg Soc. 2018;61(1):81–8.
Aslam M, Mehmood A, Rehman M, et al. Comparative study on the role of MRI in spinal tuberculosis. Indo Am J P Sci. 2018;05(11):11516–9.
Kanna RM, Babu N, Kannan M, Shetty AP, Rajasekaran S. Diagnostic accuracy of whole spine magnetic resonance imaging in spinal tuberculosis validated through tissue studies. Eur Spine J. 2019;28(12):3003–10.
Zhang N, Zeng X, He L, Liu Z, Liu J, Zhang Z, et al. The value of MR imaging in comparative analysis of spinal infection in adults: pyogenic versus tuberculous. World Neurosurg. 2019;128:e806–13.
Misra UK, Warrier S, Kalita J, Kumar S. MRI findings in Pott’s spine and correlating clinical progress with radiological findings. Neuroradiology. 2020;62(7):825–32.
Boruah DK, Gogoi BB, Prakash A, Lal NR, Hazarika K, Borah KK. Magnetic resonance imaging evaluation of posterior spinal tuberculosis: a cross-sectional study. Acta Radiol. 2021;62(8):1035–44.
Guo H, Lan S, He Y, Tiheiran M, Liu W. Differentiating brucella spondylitis from tuberculous spondylitis by the conventional MRI and MR T2 mapping: a prospective study. Eur J Med Res. 2021;26(1):125.
Kaya S, Kaya S, Kavak S, Comoglu S. A disease that is difficult to diagnose and treat: evaluation of 343 spondylodiscitis cases. J Int Med Res. 2021;49(11):3000605211060197.
Naselli N, Facchini G, Lima GM, Evangelisti G, Ponti F, Miceli M, et al. MRI in differential diagnosis between tuberculous and pyogenic spondylodiscitis. Eur Spine J. 2022;31(2):431–41.
Rasheed B, Qamari AN, Farhan N, Murtaza G, Swaleh A. Complications of tuberculosis spondylitis detected by magnetic resonance imaging (MRI): a low income country perspective. Rawal Med J. 2021;46(4):826–9.
Singh KS, Robindro P, Devi OP, Lilavati N. MRI evaluation of spinal TB: a cross-sectional study. Eur J Mol Clin Med (Baltimore). 2022;9(1):354–8.
Cheung WY, Luk KDK. Pyogenic spondylitis. Int Orthop. 2012;36(2):397–404.
Backer DAI, Mortelé KJ, Vanschoubroeck IJ, Deeren D, Vanhoenacker FM, De Keulenaer BL, et al. Tuberculosis of the spine: CT and MR imaging features. JBR-BTR. 2005;88(2):92–7.
Lew DP, Waldvogel FA. Osteomyelitis. Lancet. 2004;364(9431):369–79.
Babic M, Simpfendorfer CS. Infections of the spine. Infect Dis Clin North Am. 2017;31(2):279–97.
Cordero M, Sánchez I. Brucellar and tuberculous spondylitis. A comparative study of their clinical features. J Bone Joint Surg Br. 1991;73(1):100–3.
Jinkins JR, Bazan C 3rd, Xiong L. MR of disc protrusion engendered by infectious spondylitis. J Comput Assist Tomogr. 1996;20(5):715–8.
von Hippel PT. The heterogeneity statistic I(2) can be biased in small meta-analyses. BMC Med Res Methodol. 2015;14(15):35.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Ethical approval
This paper does not contain any studies with human or animal participants performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ling-Shan, C., Zheng-Qiu, Z., Jing, L. et al. Magnetic resonance imaging features for differentiating tuberculous from pyogenic spondylitis: a meta-analysis. Skeletal Radiol 53, 697–707 (2024). https://doi.org/10.1007/s00256-023-04459-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-023-04459-5