Abstract
Objective
To establish reference values of rotator cuff (RC) cross sectional area (CSA) in males.
Materials and methods
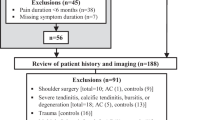
We retrospectively analyzed shoulder MRIs from 500 patients aged 13-78 years, grouped as follows (N=100 in each): <20, 20-30, 30-40, 40-50, >50 years. All examinations were reviewed to exclude prior surgery, tears, or significant RC pathology. We segmented a standardized T1 sagittal MR image in each case to obtain CSA of supraspinatus (SUP), infraspinatus/teres minor (INF), and subscapularis (SUB) muscles. Across age groups, we recorded individual and total muscle CSA. We also performed ratios between individual muscle CSA and total CSA to examine total muscle mass contribution over age groups. We tested for differences between age groups controlled for BMI.
Results
CSAs for SUP, INF, SUB, and total RC CSA were lower in subjects >50 years compared to all other groups (P<0.003 for all comparisons), persisting after controlling for BMI (P<0.03). Relative contribution of SUP CSA to total RC CSA was stable across age groups (P>0.32). INF CSA relative to total RC CSA increased with age, whereas SUB decreased (P<0.005). Subjects >50 years showed lower SUP (-15%), INF (-6%), and SUB (-21%) CSA, when compared to mean CSAs of all subjects <50 years. Total RC CSA significantly correlated with age (r=-0.34, P<0.001), persisting after controlling for BMI (r=-0.42, P<0.001).
Conclusion
RC muscles in male subjects with no tears on MRI show decreasing CSA with age, independent of BMI.





Similar content being viewed by others
Abbreviations
- CSA:
-
cross-sectional area
- INF:
-
infraspinatus / teres minor
- RC:
-
rotator cuff
- SUB:
-
subscapularis
- SUP:
-
supraspinatus
References
Zhao J, Luo M, Pan J, Liang G, Feng W, Zeng L, et al. Risk factors affecting rotator cuff retear after arthroscopic repair: a meta-analysis and systematic review. J Shoulder Elbow Surg. 2021;30:2660–70.
Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994;304:78–83.
Zanetti M, Gerber C, Hodler J. Quantitative assessment of the muscles of the rotator cuff with magnetic resonance imaging. Investig Radiol. 1998;33:163–70.
Yanagisawa O, Okumura K, Torii S. Comparison of the morphology of the rotator cuff muscles across age groups. Clin Anat. 2014;27:365–9.
Aleem AW, Chalmers PN, Bechtold D, Khan AZ, Tashjian RZ, Keener JD. Association Between Rotator Cuff Muscle Size and Glenoid Deformity in Primary Glenohumeral Osteoarthritis. J Bone Joint Surg Am. 2019;101:1912–20.
Medina G, Buckless CG, Thomasson E, Oh LS, Torriani M. Deep learning method for segmentation of rotator cuff muscles on MR images. Skelet Radiol. 2021;50:683–92.
Cameron J, McPhee JS, Jones DA, Degens H. Five-year longitudinal changes in thigh muscle mass of septuagenarian men and women assessed with DXA and MRI. Aging Clin Exp Res. 2020;32:617–24.
Peng X, Li X, Xu Z, Wang L, Cai W, Yang S, et al. Age-related fatty infiltration of lumbar paraspinal muscles: a normative reference database study in 516 Chinese females. Quant Imaging Med Surg. 2020;10:1590–601.
Ulbrich EJ, Nanz D, Leinhard OD, Marcon M, Fischer MA. Whole-body adipose tissue and lean muscle volumes and their distribution across gender and age: MR-derived normative values in a normal-weight Swiss population. Magn Reson Med. 2018;79:449–58.
Wieser K, Joshy J, Filli L, Kriechling P, Sutter R, Fürnstahl P, et al. Changes of Supraspinatus Muscle Volume and Fat Fraction After Successful or Failed Arthroscopic Rotator Cuff Repair. Am J Sports Med. 2019;47:3080–8.
Kolk A, van der Zwaal P, Thomassen BJW, van de Kamp EWC, Stijnen T, de Groot JH, et al. The presence of a rotator cuff tear interferes with age-dependent muscle atrophy of intact shoulder muscles. An MRI study with 3 years’ follow-up. Hum Mov Sci. 2018;62:161–8.
Gladstone JN, Bishop JY, Lo IKY, Flatow EL. Fatty infiltration and atrophy of the rotator cuff do not improve after rotator cuff repair and correlate with poor functional outcome. Am J Sports Med. 2007;35:719–28.
Plate JF, Bates CM, Mannava S, Smith TL, Jorgensen MJ, Register TC, et al. Age-related degenerative functional, radiographic, and histological changes of the shoulder in nonhuman primates. J Shoulder Elb Surg. 2013;22:1019–29.
Giri A, Freeman TH, Kim P, Kuhn JE, Garriga GA, Khazzam M, et al. Obesity and sex influence fatty infiltration of the rotator cuff: the Rotator Cuff Outcomes Workgroup (ROW) and Multicenter Orthopaedic Outcomes Network (MOON) cohorts. J Shoulder Elb Surg. 2022;31:726–35.
Scheibel M, Nikulka C, Dick A, Schroeder RJ, Popp AG, Haas NP. Structural integrity and clinical function of the subscapularis musculotendinous unit after arthroscopic and open shoulder stabilization. Am J Sports Med. 2007;35:1153–61.
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48:601.
Takeuchi Y, Sugaya H, Takahashi N, Matsuki K, Tokai M, Morioka T, et al. Incidence of teres minor muscle atrophy in young and middle-aged populations. JSES Int. 2022;6:459–62.
Funding
This study has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Marilyn E. Galdamez and Florian A. Huber shared first authorship.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Galdamez, M.E., Huber, F.A., Buckless, C.G. et al. Cross-sectional areas of rotator cuff muscles in males without tears on shoulder MRI. Skeletal Radiol 53, 285–291 (2024). https://doi.org/10.1007/s00256-023-04400-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-023-04400-w