Abstract
Quantitative measures of cartilage morphology (“cartilage morphometry”) extracted from high resolution 3D magnetic resonance imaging (MRI) sequences have been shown to be sensitive to osteoarthritis (OA)-related change and also to treatment interventions. Cartilage morphometry is therefore nowadays widely used as outcome measure for observational studies and randomized interventional clinical trials. The objective of this narrative review is to summarize the current status of cartilage morphometry in OA research, to provide insights into aspects relevant for the design of future studies and clinical trials, and to give an outlook on future developments. It covers the aspects related to the acquisition of MRIs suitable for cartilage morphometry, the analysis techniques needed for deriving quantitative measures from the MRIs, the quality assurance required for providing reliable cartilage measures, and the appropriate participant recruitment criteria for the enrichment of study cohorts with knees likely to show structural progression. Finally, it provides an overview over recent clinical trials that relied on cartilage morphometry as a structural outcome measure for evaluating the efficacy of disease-modifying OA drugs (DMOAD).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis (OA) is a chronic disease and a leading cause of disability [1] that is characterized by alterations of all joint tissues, which eventually lead to joint failure and need for surgical joint replacement. The pathogenesis of OA involves all joint tissues, including cartilage, subchondral bone, and fibrocartilage such as menisci and labrum (depending on joint), joint capsule, ligaments, and surrounding muscles. Structural tissue damage results in illness perceived by the patient as pain, stiffness, and functional limitations [2, 3], with the knee being the most commonly affected joint [2, 4]. Current treatment guidelines focus on the management of symptoms [5,6,7,8], as no disease-modifying OA drug (DMOAD) has been approved by regulatory authorities yet. Since cartilage loss is considered one of the hallmark features of the disease, most DMOAD candidates aim to stop or slow cartilage loss or to stimulate cartilage growth [9].
Clinical trials evaluating DMOAD efficacy traditionally relied on quantitatively measured radiographic joint space width (JSW), considered a surrogate for cartilage loss and integrity. Radiography is, however, not able to directly depict the articular cartilage and radiographically measured JSW represents a composite measure as the joint space is maintained by both cartilage and meniscus [10, 11]. Magnetic resonance imaging (MRI), in contrast, provides a direct depiction of all tissues, including the articular cartilage, and is now widely used in OA research and clinical trials for pharmaceutical development [12].
Since Peterfy et al. reported that an accurate and reproducible volumetric quantification of articular cartilage in the knee is possible from 3D MRI in 1994 [13], numerous observational and interventional studies employed quantitative measurements of cartilage morphology [14, 15]. Developments in this field have been driven by the need for reliable and sensitive MRI-based imaging biomarkers suitable for replacing JSW as structural efficacy outcome measure in clinical trials. Important insights on feasibility, reliability, and validity of MRI have been made possible through its application in large longitudinal studies (e.g. progressive vs. non-progressive disease). One example is the Osteoarthritis Initiative (OAI), which provides a large variety of data for a total of 4796 participants, including high-resolution knee MRIs suitable for quantitative cartilage analyses [15].
The objective of this narrative review is to summarize the current status of quantitative cartilage morphology measurements (i.e., cartilage morphometry) in OA research, to provide insights into aspects relevant for the design of future studies and clinical trials, and to give an outlook on future developments. Since cartilage morphometry is mainly used in the context of knee OA, this review focuses on the knee. The methodologies used for cartilage morphometry can, however, also be translated to other joints.
Image acquisition
Cartilage morphometry requires high resolution, 3D gradient echo sequences that provide a sufficient contrast between the articular cartilage, the subchondral bone, the menisci, and intraarticular fluid. Earlier studies have validated MRI sequences such as T1-weighted spoiled gradient echo (SPGR, GE) MRI, fast low angle shot (FLASH, Siemens), fast field echo (FFE, Philips), or water selective cartilage (WATSc, Philips) MRI against external standards (e.g., water displacement or CT arthrography) and reported a high accuracy for 3D cartilage volume, thickness, and area measurements (Table 1) [13, 16,17,18,19,20,21,22]. In order to reduce chemical shift artefacts, all of these MRI sequences use selective water excitation as a means of fat suppression [13, 16,17,18,19,20,21,22]. These MRI sequences have been shown to allow reproducible assessment of cartilage morphology parameters and are therefore widely used in observational and interventional studies [14, 23, 24]. More recently, MRI sequences such as 3D double echo at steady state (DESS, Siemens) with water excitation (or comparable protocols from other vendors) became available [25,26,27], which additionally allow to estimate the cartilage T2 relaxation time as a measure of cartilage composition and to perform semi-quantitative assessments of some joint pathologies [28]. The magnetic field strength should be at least 1.5 T in order to ensure a sufficient signal-to-noise ratio and resolution at a reasonable scan time; precision errors have been reported to be smaller for 3 T MRI than for 1.5 T MRI [29]. In addition, scan times (i.e., burden on the patient) are reduced at 3 T MRI.
Most current cartilage morphometry studies employ an in-plane resolution of ~ 0.3 mm and a slice thickness between 1.0 and 1.5 mm, which lies within the range suggested in the OARSI clinical trial recommendations [23]. This resolution has been shown to provide a satisfactory accuracy and reproducibility and a high sensitivity to change [14]. Thinner slices have been associated with smaller precision errors [29] but were not observed to translate into a relevant improvement of the sensitivity to change in a study comparing the sensitivity to change between sagittal DESS MRIs with 0.7 mm vs. 1.4 mm slice thickness [30].
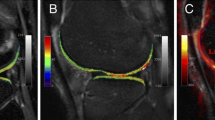
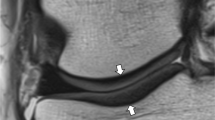
Because partial volume effects impair the precision and accuracy of quantitative cartilage morphology measurements, the slice orientation needs to be chosen perpendicular to the structures of interest. The sagittal orientation is the most versatile one, as it can be used for analyzing the cartilages in the whole tibiofemoral as well as the patellofemoral joint (Fig. 1). Coronal orientations provide a good depiction of the central, weight-bearing part of the tibiofemoral joint cartilages, but are not suitable for the patellofemoral joint or the posterior aspects of the femoral condyles (Fig. 1). These cartilages can, instead, be well analyzed from axial scans (Fig. 1). Isotropic or near-isotropic, high-resolution scans provide the advantage of having only small partial volume effects for all imaging planes. They require longer scan times or provide only a limited signal-to-noise ratio, but allow reducing the impact of partial-volume effects on cartilage morphometry when imaging spherical joints such as the hip. 3D fast spin-echo MRI protocols such as CAIPIRINHA (Controlled Aliasing in Parallel Imaging Results in Higher Acceleration) provide isotropic scans with reasonable signal-to-noise ratio at reasonable acquisition times due to higher acceleration factors [31,32,33,34]. The resolution of such scans is, however, typically not as high (≥ 0.5 mm) than that used for cartilage morphometry from gradient echo MRI (~ 0.3 mm) and the accuracy and precision of cartilage morphometry based on such this or comparable fast spin-echo sequences still needs to be evaluated (e.g., against external standards or previously validated sequences).
Illustration showing the MRI orientations and the cartilages that can be analyzed from these orientations. a Sagittal MRI slice through the medial compartment, b sagittal MRI slice through the lateral compartment, c coronal MRI slice, d axial MRI slice (P: patella, TrF: trochlea of the femur, MF: medial femur, LF: lateral femur, MT: medial tibia, LT: lateral tibia). The double echo at steady state (DESS) MRIs were provided by the Osteoarthritis Initiative image data base
In longitudinal studies, the scan parameters (e.g., MRI system, coils) need to remain consistent for all time points of the same subject, because a change of equipment during a study typically results in a systematic offset that may exceed the longitudinal change [27, 29, 35]. Multi-center studies relying on equipment from different vendors at different sites have shown consistent cartilage thickness values and precision errors [27, 36], e.g. by the application of phantoms and cross-validation of the acquired images [37]. Such trials have used different, but comparable 3D sequences that allow for cartilage quantification such as FLASH/VIBE/SPGR/T1-FFE/WATSc protocols and DESS-like protocols, which have been shown to provide a comparable sensitivity to change [30]. Current clinical trials recruit patients at multiple centers using MRI protocols that are tailored to the equipment available at the respective site [31]. Before the scanning of subjects starts, all centers need to be qualified and the image quality approved to ensure a sufficient quality of the scans.
Cartilage morphometry depends heavily on the standardization and quality of the MRIs. Studies using cartilage morphometry as an outcome measure should therefore prepare detailed, standardized imaging protocols addressing all imaging-related aspects. The OAI Imaging protocol can serve as reference when developing the imaging protocol for current studies (see https://nda.nih.gov/static/docs/StudyDesignProtocolAndAppendices.pdf) [26]. In addition, for randomized clinical DMOAD trials, an imaging charter is required (https://www.fda.gov/regulatory-information/search-fda-guidance-documents/clinical-trial-imaging-endpoint-process-standards-guidance-industry) [39]. As repetitions of unsuitable/inappropriate scans may be difficult or even impossible (e.g., pre-treatment baseline scans cannot be repeated after the start of the treatment), a timely quality check of the scans is of great importance for clinical trials. Aspects that should be covered during the quality assurance process include:
-
Complete coverage of the whole joint
-
Adequate orientation of the scans
-
Absence of artefacts (e.g., motion, metal) in the region(s) of interest
-
Overall image quality (e.g., image contrast, signal-to-noise ratio)
-
Imaging parameters consistent with the imaging protocol
-
Correct joint imaged across visits
Image analysis
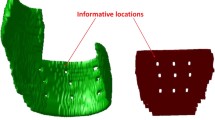
Cartilage morphometry requires segmentation of the articular cartilage as a basis for calculating quantitative measures (e.g., thickness, volume, or area, Table 2, Fig. 2). The manual segmentation of cartilage by expert readers is still considered the gold standard [40]. It has been employed as an outcome measure in observational studies and clinical trials [14, 15, 38, 41] and has also been used for training automated segmentation techniques as well as a reference for evaluating the performance of automated methods [42,43,44,45,46,47]. Numerous semi- and fully automated segmentation methodologies have been proposed over the last 2 decades for automatically segmenting the articular cartilages, ranging from b-spline snakes [48], edge-tracking [49], or local area cartilage segmentation [50] over shape-based methods [45] and clustering approaches [51] to deep learning-based techniques [46]. Ebrahimkani et al. recently published a review on segmentation techniques used in OA research [47]. All segmentation techniques, automated and manual, should be thoroughly validated to ensure the reliability and accuracy of the results. A centralized quality control of all segmentations is recommendable for manual cartilage segmentations and has recently been suggested to also improve the sensitivity to change when applied to deep learning-based cartilage segmentations [52].
In addition to high quality segmentation, appropriate and validated software is required for computing quantitative 3D cartilage measures. Simplistic measures (e.g., cartilage volume) can be derived from cartilage segmentations using off-the-shelf software (e.g., ImageJ), whereas the computation of more specialized measures (e.g., cartilage thickness over the total area of subchondral bone) typically requires dedicated and validated software solutions. An overview over the variety of measures (e.g., cartilage thickness, volume, total area of subchondral bone, cartilage surface area) that can be derived from cartilage segmentation has been published [53] (Table 2, Fig. 2). Several recent clinical trials used cartilage thickness measures as primary or secondary outcomes [38, 41, 54, 55], while others still rely on cartilage volume as an outcome measure [56, 57].
Cartilage morphometry can be derived from individual cartilage plates but also from aggregate regions (e.g., medial femorotibial compartment), defined regions of interest (e.g., weight-bearing, central part of the medial femoral condyle), or for cartilage subregions (Fig. 3) [53, 58]. Larger regions of interest (e.g., medial femorotibial compartment) have been reported to show a smaller variability of the longitudinal change in morphometric measures than smaller regions of interest (e.g., central subregion of the medial tibia) [59]. Smaller regions of interest may, instead, be advantageous in case of risk factors for progression, that are expected to specifically affect defined regions of interest (e.g., meniscus extrusion [60] or tears [61]). The decision on a specific region of interest selected for measuring the outcome should generally be aligned with the enrollment criteria, in order to avoid too broad or too narrow regions of interest (e.g., medial instead of total femorotibial joint cartilage thickness as outcome measure when selecting knees with medial joint space narrowing only).
3D reconstruction of the total area of subchondral bone showing the femorotibial cartilage regions and the 16 femorotibial cartilage subregions (prefix a/c/e/i/p: anterior/central/external/internal/posterior subregion of the respective cartilage plate, e.g., cMT: central subregion of MT). a—Shows the tibial cartilage subregions, b—shows the weight-bearing, central femoral cartilage subregions, c—shows the medial and the lateral femorotibial compartment
Location-independent measures of change in cartilage morphology such as ordered values of subregional change [62,63,64] or thinning and thickening scores [65, 66] have been developed to remove the link between the magnitude of change and the location of change and to thereby focus on the regions with the greatest magnitude of thickness loss or gain, wherever it is located within the joint. Ordered values of subregional change can be computed by ordering the change observed in each of the 16 subregions within each knee in ascending order, whereas thinning or thickening scores can be computed by summing all negative or positive changes within each knee [66]. Location-independent measures have been shown to be highly sensitive to differences of change between groups and also to be sensitive to treatment effects induced by DMOAD candidates [64, 67, 68]. Moreover, they allow separate assessments of the efficacy of DMOAD candidates for reducing cartilage thickness loss (thinning score) and for stimulating cartilage growth (thickening score).
Sensitivity of cartilage morphometry
Cartilage morphometry has been shown to be sensitive to OA-related change in longitudinal studies [14]. The sensitivity to change has been reported to depend on the participant selection criteria, the length of the follow-up period, and on the outcome measure [14, 69,70,71,72] and has also been suggested to be greater for cartilage morphometry than for radiographic JSW measurements [14, 73, 74]. The standardized response mean (SRM, i.e., the ratio between the magnitude of change and the standard deviation of change) is frequently used as a measure of the sensitivity to change in knee OA studies. Furthermore, cartilage morphometry has been shown to be sensitive to differences in change between groups, e.g., in observational studies evaluating the impact of risk factors for progression [71, 75,76,77,78,79,80]. More recently, quantitative cartilage morphology measures have been reported to be sensitive to treatment-related effects, by demonstrating a dose–response effect of femorotibial cartilage thickness change in the Sprifermin phase 2 trial over 2 and 5 years [41, 81, 82].
Predictors of structural progression
Cartilage morphometry is widely used in longitudinal studies to evaluate the impact of risk factors on cartilage loss [75,76,77,78, 80], to characterize the magnitude and the pattern of cartilage loss in different cohorts [15, 76, 83, 84], and to study the efficacy of treatment interventions on slowing or stopping cartilage loss or on stimulating cartilage growth [38, 41, 54,55,56]. Because early stages of OA are not characterized by substantial cartilage loss but by alterations of the cartilage composition and matrix integrity [85], cartilage morphometry is mainly used in cohorts with definite signs of radiographic OA (e.g., osteophytes, joint space narrowing).
Kellgren and Lawrence grades are typically used to distinguish between knees with (KLG 2–4) vs. without (KLG 0–1) definite radiographic OA [86]. But even in knees with definite radiographic OA (KLG 2–4), cartilage tissue loss is a slow process [79], in particular in knees with KLG 2, in which not only thinning (i.e. cartilage degradation) but also thickening of cartilage (i.e. cartilage swelling and/or potential anabolic tissue response) has been observed to take place simultaneously [87]. Numerous studies and projects therefore investigated factors predictive of subsequent progression that would allow enriching clinical trials with knees likely to exhibit accelerated structural progression and that are therefore in need of a structure-modifying treatment. The FNIH-funded “Osteoarthritis Biomarkers” (https://fnih.org/our-programs/biomarkers-consortium/osteoarthritis-project) and “PROGRESS OA” (https://fnih.org/our-programs/biomarkers-consortium/programs/progress-oa) projects aimed for the identification and the regulatory approval of prognostic biomarkers for structural and/or symptomatic OA disease progression [88]. IMI-APPROACH (https://www.approachproject.eu/), a 2-year, European, prospective follow-up cohort project, collected conventional and novel clinical, imaging, and biochemical (bio)markers to validate and refine predictive machine-learning models for pre-identified and new progressor phenotypes based on these markers [89].
Radiography is traditionally used for the selection of participants for OA studies and KL grades have been shown to perform well as predictors of cartilage thickness loss [79]. Cartilage thickness changes in the medial/lateral femorotibial compartment have been reported to amount to + 0.1%/ + 0.2% in KLG 0 knees without risk factors for developing OA (healthy reference group), to − 0.3%/ − 0.2% in KLG 2 knees, to − 1.2%/ − 0.8% in KLG 3 knees, and to − 2.0%/ − 1.5% in KLG 4 knees over one year [79]. Knees with KLG 3 or 4 were reported to show more cartilage thickness loss than KLG 0 knees in this study [79], but these changes were still below the magnitude of intra- and inter-reader precision errors determined in a meta-analysis (coefficient of variation for both: 3%) [90]. This may be explained by the fact that KL grades are composite scores that take several OA-related radiographic features into account and do not allow a selection based on the predominantly affected compartment. Furthermore, recent studies reported that knees with KLG 2, which are typically included in treatment trials, not necessarily have cartilage damage [91]. This may be the case in up to one third of the KL2 knees included [92]. Inclusion of patients without cartilage damage in DMOAD trials assessing efficacy of a cartilage-anabolic compound is, however, not recommended, because there is neither an actual need for cartilage treatment nor are they likely to develop cartilage loss over the course of the trial.
Radiographic JSN scores [93] have been reported to be a strong predictor of cartilage loss in the narrowed compartment [94]. They have recently been successfully used in combination with KL grades to enrich the population of the ROCCELLA trial with knees likely to show medial compartment progression [38, 95], but are not only affected by cartilage status but also by meniscus integrity and extrusion [10].
MRI-based ordinal expert scoring such as ROAMES and MOAKS not only allows to identify knees that should not be included in clinical trials (e.g., because of subchondral insufficiency fracture) [96], but also to specifically select knees likely to show subsequent cartilage thickness loss (e.g., based on size and depth of cartilage damage or presence of inflammation) [97]. Besides selecting knees with a high likelihood of showing cartilage loss, it is crucial for clinical trials to consider the mode-of-action of the respective compound, in order to ensure that the DMOAD candidate is effective in the knees included in the cohort. MRI-based scorings may allow to select knees likely to be susceptible for treatment effects of a DMOAD candidate more specifically than radiographic measures (e.g. based on MRI-based extent of cartilage damage instead of radiographic JSN), but also to exclude knees, in which a treatment effect seems unlikely because of strong biomechanical factors (e.g., meniscus root tears) or because of too severe cartilage damage.
A detailed overview reporting the magnitude of change and the sensitivity to change in different cohorts with various selection criteria and observation period lengths has been published [14]. Short-term studies (e.g., 3 or 6 months) have been reported to be at high risk of failure because of insufficient longitudinal change [70]. Most studies therefore choose observation periods of 12 months or longer [14].
Overview over recent clinical trials
Several recent clinical trials included cartilage morphometry as an outcome measure. The FORWARD study, a phase 2 trial evaluating the efficacy and safety of Sprifermin as DMOAD in 549 patients with tibiofemoral OA, relied on manual, quality-controlled cartilage segmentations from coronal gradient echo MRI that were acquired using 1.5 T or 3 T MRI scanners from different manufacturers (slice thickness: 1.5 mm, in-plane resolution: ~ 0.3 mm) for assessing the structural efficacy [41, 82]. This trial reported statistically significant, dose-dependent increases in the total femorotibial cartilage thickness over 2 and 5 years when compared against placebo (difference vs. placebo in highest dose group: 0.05 mm, 95% CI: [0.03, 0.07]mm) [41, 82]. Statistically significant dose–response effects were also observed for medial and lateral femorotibial cartilage thickness using cartilage morphometry, while radiographic JSW showed such effects only in the lateral but not in the medial compartment. A post hoc analysis reported a dose–response effect from automated cartilage segmentations that was consistent with the dose–response effect observed in the primary analysis [81]. Despite the structural efficacy, the FORWARD trial was not able to demonstrate clinical translation of Sprifermin in the full cohort (i.e., pain reduction). A recent post hoc analysis of a subset of FORWARD participants with severe OA (severe pain and low JSW) at baseline suggested, however, that Sprifermin may not only have structure-modifying but also symptom modifying efficacy, indicating that future studies evaluating Sprifermin should potentially focus on more advanced stages of OA [98].
The TPX-100–5 study used sagittal gradient echo MRIs acquired on 1.5 T MRI scanners from different manufacturers (slice thickness: 1.5 mm, in-plane resolution: ~ 0.3 mm) for evaluating the structural efficacy of intraarticular TPX-100 as potential DMOAD in knees with patellofemoral cartilage defects. The TPX-100–5 study reported clinically meaningful functional benefits over 1 year, while no effects on cartilage thickness from manual, quality-controlled segmentations could be observed [99]. This was explained by the limited magnitude of cartilage loss observed in the 93 subjects. A post hoc analysis performed in 78 of the 93 knees reported, however, a weak correlation between cartilage thickness change and changes in bone shape in the medial femoral condyle of knees treated with TPX-100 [55].
The efficacy and safety of MIV-711 as a potential DMOAD was evaluated over 26 weeks in 244 participants with primary knee OA [54]. When compared to placebo, the study observed no efficacy with regard to pain, but reported a significant reduction of central femoral cartilage thickness loss for the lower-dose group (100 mg MIV-711) as well as a treatment effect on bone shape for both treatment groups (100 mg & 200 mg MIV-711). The change in the central femoral cartilage thickness observed in the MIV-711, 200 mg group as well as the change observed in the central medial tibial cartilage thickness did, however, not differ from that observed for the placebo group. This study utilized statistical shape modelling methods for assessing cartilage loss, which were applied to spin-echo MRIs acquired using 1.5 T or 3 T MRI scanners from different manufacturers (slice thickness and resolution not reported).
ROCCELLA was a 52-week, randomized, double-blind phase 2 study that evaluated the efficacy and safety of s201086/GLPG1972 as a potential DMOAD in 932 knee OA patients [38, 95]. By enrolling patients with KLG 2 or 3 in combination with the presence of medial JSN 1 or 2, the study successfully enrolled knees with a sufficient loss in cartilage thickness to enable assessment of a structural benefit of s201086/GLPG1972 vs. placebo over 52 weeks. Still, ROCCELLA showed no effect on change from baseline to week 52 in the central medial femorotibial cartilage thickness (primary endpoint, based on manual, quality-controlled cartilage segmentations from sagittal gradient echo scans acquired using 1.5 T or 3 T scanners from different manufacturers, slice thickness: 1.5 mm, in-plane resolution: ~ 0.3 mm) or other outcomes (including pain measures and radiographic JSW). The selection criteria used for ROCCELLA may, however, be helpful for future clinical trials.
Several clinical trials evaluated the safety and efficacy of the injection of platelet-rich plasma (PRP) as a potential OA treatment, but only one of these trials assessed the potential structural efficacy using cartilage morphometry. The RESTORE trial evaluated the effects of intra-articular PRP injections in patients with symptomatic mild to moderate radiographic medial knee OA in 288 patients over 12 months [56]. When compared to placebo, the RESTORE trial found no significant differences in symptoms or change in medial tibial cartilage volume, which was measured manually from gradient echo MRI acquired on 3 T Philips or Siemens scanners (slice thickness: 0.5–0.6 mm, in-plane resolution: 0.5 × 0.5 to 0.66 × 0.63 mm).
Although these recent clinical trials employing quantitative cartilage morphology measurements as outcome were well designed and conducted, only two of the trials were able to demonstrate structural benefits based on different MRI protocols and different image analysis techniques and only one of these trials was able to demonstrate a dose–response effect on structural progression until today.
Based on the observation that cartilage thickness loss is only weakly associated with worsening of knee pain, a recent study raised the question, whether pain reduction can actually be achieved by chondroprotection [100]. This weak association may, however, be due to the relatively low baseline WOMAC pain severity in this cohort (average: 2.4 ± 3.1, scale 0…20), which also increased only slightly over 2 years (0.62 ± 3.4). In contrast to this study, the results from the Sprifermin subgroup at risk of progression demonstrated that pain reduction and structural benefits can be achieved by successfully stopping or even reverting cartilage loss in patients with severe baseline pain (median: 54, scale 0…100) [98]. Future studies aiming for the translation of a structural treatment effect into a clinical benefit should therefore most likely focus on knees with severe pain.
Future directions
MRI and cartilage morphometry are still not accepted as primary outcome measures by regulatory agencies (FDA and EMA) for approval of cartilage-targeting molecules. Therefore, the qualification of MRI-based, direct measures of change in cartilage morphology as outcome measure for clinical trials is of great importance. This would allow to overcome the limitations of using radiographic JSW loss (e.g., impact of meniscus integrity and extrusion [10, 11] or the impact of knee positioning and x-ray beam alignment) as an indirect measure of cartilage loss.
Machine-learning techniques are increasingly used in OA research [46, 101] and have been used to identify predictors for structural OA progression [46, 101,102,103]. However, most of these studies relied on radiographic inclusion criteria of patients and radiographic instead of MRI-based measures of progression as outcome. More sophisticated machine learning models are likely to emerge, that may be able to provide reliable predictions of structural progression. Such prediction models will be valuable for enrolling patients likely to show symptom worsening and sufficient cartilage loss over the course of a trial. Future studies should also aim for directly predicting MRI-based cartilage loss instead of worsening of radiographic outcomes. After successful development and approval of a therapy with disease-modifying properties, automated segmentation techniques based on machine-learning may eventually allow the application of quantitative cartilage morphometry for treatment monitoring in individual OA patients. Cartilage morphometry is currently mostly used in knees with definite radiographic OA, with the presence of definite radiographic OA being the most widely used selection criterion for compiling cohorts likely to show structural progression [14, 79, 94]. More recently, prevalent MRI-based baseline cartilage damage has been shown to be predictive of subsequent further cartilage loss [104, 105] and has also been reported to occur in knees without definite radiographic OA [106]. More sophisticated selection criteria, such as simplified and less time-consuming MRI-based assessment of joint pathologies, machine-learning-based models, or dedicated early OA models such as the presence of radiographic OA in the contralateral knee [107], may allow to eventually also apply cartilage morphometry in the context of early OA or preventive studies.
Summary
MRI-based cartilage morphometry has been demonstrated to be sensitive to OA-related change and also to treatment interventions and is nowadays widely used as an outcome measure in observational studies as well as interventional trials. Suitable imaging sequences are available for most of the 1.5 T and 3 T scanners currently used in clinical routine and have been validated to provide a high accuracy and reproducibility. Currently established predictors allow the selection of knees likely to show subsequent progression over the course of a clinical trial. Still, only few of the DMOAD trials were able to demonstrate structure modification of the drug candidates and no DMOAD has been approved by regulatory authorities yet. Lessons learned from previous trials and more sophisticated participant selection criteria (potentially based on machine-learning models) are likely to provide valuable guidance for future clinical trials relying on MRI-based cartilage morphometry as structural outcome measure.
References
Vos T, Abajobir AA, Abbafati C, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1211–59.
Hunter DJ, Bierma-Zeinstra S. Osteoarthritis. Lancet. 2019;393(10182):1745–59.
Kraus VB, Blanco FJ, Englund M, Karsdal MA, Lohmander LS. Call for standardized definitions of osteoarthritis and risk stratification for clinical trials and clinical use. Osteoarthr Cartil. 2015;23(8):1233–41.
Prieto-Alhambra D, Judge A, Javaid MK, Cooper C, Diez-Perez A, Arden NK. Incidence and risk factors for clinically diagnosed knee, hip and hand osteoarthritis: influences of age, gender and osteoarthritis affecting other joints. Ann Rheum Dis. 2014;73(9):1659–64.
Katz JN, Arant KR, Loeser RF. Diagnosis and treatment of hip and knee osteoarthritis: a review. JAMA - J Am Med Assoc. 2021;325(6):568–78.
Bannuru RR, Osani MC, Vaysbrot EE et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthr Cartil
Kolasinski SL, Neogi T, Hochberg MC, et al. 2019 American College of Rheumatology/Arthritis Foundation guideline for the management of osteoarthritis of the hand, hip, and knee. Arthritis Rheumatol. 2020;72(2):220–33.
Overton C, Nelson AE, Neogi T. Osteoarthritis treatment guidelines from six professional societies: similarities and differences. Rheum Dis Clin North Am. 2022;48(3):637–57.
Cho Y, Jeong S, Kim H, et al. Disease-modifying therapeutic strategies in osteoarthritis: current status and future directions. Exp Mol Med. 2021;53(11):1689–96.
Hunter DJ, Zhang YQ, Tu X, et al. Change in joint space width: hyaline articular cartilage loss or alteration in meniscus? Arthritis Rheum. 2006;54(8):2488–95.
Roth M, Wirth W, Emmanuel K, Culvenor AG, Eckstein F. The contribution of 3D quantitative meniscal and cartilage measures to variation in normal radiographic joint space width—data from the Osteoarthritis Initiative healthy reference cohort. Eur J Radiol. 2017;87:90–8.
Roemer FW, Guermazi A, Demehri S, Wirth W, Kijowski R. Imaging in osteoarthritis. Osteoarthr Cartil. 2021;30(7):913–34.
Peterfy CG, van Dijke CF, Janzen DL, et al. Quantification of articular cartilage in the knee with pulsed saturation transfer subtraction and fat-suppressed MR imaging: optimization and validation. Radiology. 1994;192(0033–8419):485–91.
Eckstein F, Guermazi A, Gold G, et al. Imaging of cartilage and bone: promises and pitfalls in clinical trials of osteoarthritis. Osteoarthr Cartil. 2014;22(10):1516–32.
Eckstein F, Wirth W, Nevitt MC. Recent advances in osteoarthritis imaging-the Osteoarthritis Initiative. Nat Rev Rheumatol. 2012;8(10):622–30.
Graichen H, Eisenhart-Rothe RV, Vogl T, Englmeier KH, Eckstein F. Quantitative assessment of cartilage status in osteoarthritis by quantitative magnetic resonance imaging: technical validation for use in analysis of cartilage volume and further morphologic parameters. Arthritis Rheum. 2004;50(0004–3591):811–6.
Burgkart R, Glaser C, Hyhlik-Dürr A, et al. Magnetic resonance imaging-based assessment of cartilage loss in severe osteoarthritis: accuracy, precision, and diagnostic value. Arthritis Rheum. 2001;44(0004–3591):2072–7.
Schnier M, Eckstein F, Priebsch J, et al. Three-dimensional thickness and volume measurements of the knee joint cartilage using MRI: validation in an anatomical specimen by CT arthrography. Rofo. 1997;167(5):521–6.
Dupuy DE, Spillane RM, Rosol MS, et al. Quantification of articular cartilage in the knee with three-dimensional MR imaging. AcadRadiol. 1996;3(1076–6332):919–24.
Kornaat PR, Doornbos J, van der Molen AJ, et al. Magnetic resonance imaging of knee cartilage using a water selective balanced steady-state free precession sequence. JMagn Reson. 2004;20(5):850–6.
Cohen ZA, McCarthy DM, Kwak SD, et al. Knee cartilage topography, thickness, and contact areas from MRI: in-vitro calibration and in-vivo measurements. Osteoarthr Cartil. 1999;7(1063–4584):95–109.
Haubner M, Eckstein F, Schnier M, et al. A non-invasive technique for 3-dimensional assessment of articular cartilage thickness based on MRI. Part 2: validation using CT arthrography. Magn Reson. 1997;15(0730–725X):805–13.
Hunter DJ, Altman RD, Cicuttini F, et al. OARSI clinical trials recommendations: knee imaging in clinical trials in osteoarthritis. Osteoarthr Cart. 2015;23(5):698–715.
Eckstein F, Bernard K, Deckx H, et al. Test-retest reliability and smallest detectable change (SDC) of MRI-based cartilage thickness analysis in a large multicenter randomized controlled clinical trial of knee osteoarthritis. Osteoarthr Cartil. 2021;29:S327–8.
Eckstein F, Hudelmaier M, Wirth W, et al. Double echo steady state magnetic resonance imaging of knee articular cartilage at 3 Tesla: a pilot study for the Osteoarthritis Initiative. Ann Rheum Dis. 2006;65(4):433–41.
Peterfy CG, Schneider E, Nevitt M. The osteoarthritis initiative: report on the design rationale for the magnetic resonance imaging protocol for the knee. Osteoarthr Cartil. 2008;16(12):1433–41.
Balamoody S, Williams TG, Waterton JC, et al. Comparison of 3T MR scanners in regional cartilage-thickness analysis in osteoarthritis: a cross-sectional multicenter, multivendor study. Arthritis ResTher. 2010;12(5):R202.
Chaudhari AS, Black MS, Eijgenraam S, et al. Five-minute knee MRI for simultaneous morphometry and T2 relaxometry of cartilage and meniscus and for semiquantitative radiological assessment using double-echo in steady-state at 3T. J Magn Reson Imaging. 2018;47(5):1328–41.
Eckstein F, Charles HC, Buck RJ, et al. Accuracy and precision of quantitative assessment of cartilage morphology by magnetic resonance imaging at 3.0T. Arthritis Rheum. 2005;52(10):3132–6.
Wirth W, Nevitt M, Hellio Le Graverand MP, et al. Sensitivity to change of cartilage morphometry using coronal FLASH, sagittal DESS, and coronal MPR DESS protocols--comparative data from the Osteoarthritis Initiative (OAI). Osteoarthr Cartil. 2010;18(4):547–54.
Altahawi F, Pierce J, Aslan M, Li X, Winalski CS, Subhas N. 3D MRI of the Knee. Semin Musculoskelet Radiol. 2021;25(3):455–67.
Van Dyck P, Smekens C, Roelant E, Vande VT, Snoeckx A, De Smet E. 3D CAIPIRINHA SPACE versus standard 2D TSE for routine knee MRI: a large-scale interchangeability study. Eur Radiol. 2022;32(9):6456–67.
Fritz J, Fritz B, Thawait GG, Meyer H, Gilson WD, Raithel E. Three-dimensional CAIPIRINHA SPACE TSE for 5-minute high-resolution MRI of the knee. Invest Radiol. 2016;51(10):609–17.
Del GF, Delcogliano M, Guglielmi R, et al. Fully automated 10-minute 3D CAIPIRINHA SPACE TSE MRI of the knee in adults: a multicenter, multireader, multifield-strength validation study. Invest Radiol. 2018;53(11):689–97.
Eckstein F, Kunz M, Hudelmaier M, et al. Impact of coil design on the contrast-to-noise ratio, precision, and consistency of quantitative cartilage morphometry at 3 Tesla: a pilot study for the osteoarthritis initiative. Magn Reson Med. 2007;57(2):448–54.
Eckstein F, Buck RJ, Burstein D, et al. Precision of 3.0 Tesla quantitative magnetic resonance imaging of cartilage morphology in a multicentre clinical trial. Ann Rheum Dis. 2008;67(12):1683–8.
Schneider E, NessAiver M, White D, et al. The osteoarthritis initiative (OAI) magnetic resonance imaging quality assurance methods and results. Osteoarthr Cartil. 2008;16(9):994–1004.
Imbert O, Deckx H, Bernard K, et al. The design of a randomized, placebo-controlled, dose-ranging trial to investigate the efficacy and safety of the ADAMTS-5 inhibitor S201086/GLPG1972 in knee osteoarthritis. Osteoarthr Cartil Open. 2021;3(4):100209.
Alberich-Bayarri A, Sourbron S, Golay X, et al. ESR statement on the validation of imaging biomarkers. Insights Imaging
Chaudhari AS, Kogan F, Pedoia V, Majumdar S, Gold GE, Hargreaves BA. Rapid knee MRI acquisition and analysis techniques for imaging osteoarthritis. J Magn Reson Imaging. 2020;52(5):1321–39.
Hochberg MC, Guermazi A, Guehring H, et al. Effect of intra-articular sprifermin vs placebo on femorotibial joint cartilage thickness in patients with osteoarthritis. JAMA. 2019;322(14):1360.
Desai AD, Caliva F, Iriondo C, et al. The international workshop on osteoarthritis imaging knee mri segmentation challenge: a multi-institute evaluation and analysis framework on a standardized dataset. Radiol Artif Intell. 2021;3(3):1–13.
Wirth W, Eckstein F, Kemnitz J, et al. Accuracy and longitudinal reproducibility of quantitative femorotibial cartilage measures derived from automated U-Net-based segmentation of two different MRI contrasts: data from the osteoarthritis initiative healthy reference cohort. Magn Reson Mater Physics, Biol Med.
Ambellan F, Tack A, Ehlke M, Zachow S. Automated segmentation of knee bone and cartilage combining statistical shape knowledge and convolutional neural networks: data from the Osteoarthritis Initiative. Med Image Anal. 2019;52:109–18.
Williams TG, Holmes AP, Bowes M, et al. Measurement and visualisation of focal cartilage thickness change by MRI in a study of knee osteoarthritis using a novel image analysis tool. Br J Radiol. 2010;83(995):940–8.
Joseph GB, McCulloch CE, Sohn JH, Pedoia V, Majumdar S, Link TM. AI MSK clinical applications: cartilage and osteoarthritis. Skeletal Radiol. 2022;51(2):331–43.
Ebrahimkhani S, Jaward MH, Cicuttini FM, Dharmaratne A, Wang Y, de Herrera AGS. A review on segmentation of knee articular cartilage: from conventional methods towards deep learning. Artif Intell Med. 2020;106(February):101851.
Stammberger T, Eckstein F, Michaelis M, Englmeier KH, Reiser M. Interobserver reproducibility of quantitative cartilage measurements: comparison of b-spline snakes and manual segmentation. Magn Reson Imaging. 1999;17(7):1033–42.
Duryea J, Neumann G, Brem MH, et al. Novel fast semi-automated software to segment cartilage for knee MR acquisitions. Osteoarthr Cartil 2007;15(1063–4584 (Print)):487–492
Duryea J, Iranpour-Boroujeni T, Collins JE, et al. Local area cartilage segmentation: a semiautomated novel method of measuring cartilage loss in knee osteoarthritis. Arthritis Care Res. 2014;66(10):1560–5.
Folkesson J, Dam EB, Olsen OF, Pettersen PC, Christiansen C. Segmenting articular cartilage automatically using a voxel classification approach. IEEE Trans Med Imaging 2007;26(0278–0062 (Print)):106–115
Maschek S, Wisser A, Jansen M, et al. Do automated, U-net-based cartilage segmentations from Mri benefit from manual quality control and correction? Data from the Imi-approach project. Osteoarthr Imaging. 2022;2:100016.
Eckstein F, Ateshian G, Burgkart R, et al. Proposal for a nomenclature for magnetic resonance imaging based measures of articular cartilage in osteoarthritis. Osteoarthr Cartil. 2006;14(10):974–83.
Conaghan PG, Bowes MA, Kingsbury SR, et al. Disease-modifying effects of a novel cathepsin k inhibitor in osteoarthritis: a randomized controlled trial. Ann Intern Med. 2020;172(2):86–95.
McGuire D, Bowes M, Brett A, et al. Study TPX-100–5: intra-articular TPX-100 significantly delays pathological bone shape change and stabilizes cartilage in moderate to severe bilateral knee OA. Arthritis Res Ther. 2021;23(1):1–9.
Bennell KL, Paterson KL, Metcalf BR, et al. Effect of intra-articular platelet-rich plasma vs placebo injection on pain and medial tibial cartilage volume in patients with knee osteoarthritis: the RESTORE randomized clinical trial. JAMA - J Am Med Assoc. 2021;326(20):2021–30.
McAlindon TE, LaValley MP, Harvey WF, et al. Effect of intra-articular triamcinolone vs saline on knee cartilage volume and pain in patients with knee osteoarthritis a randomized clinical trial. JAMA - J Am Med Assoc. 2017;317(19):1967–75.
Wirth W, Eckstein F. A technique for regional analysis of femorotibial cartilage thickness based on quantitative magnetic resonance imaging. IEEE Trans Med Imaging. 2008;27(6):737–44.
Wirth W, Hellio Le Graverand MP, Wyman BT, et al. Regional analysis of femorotibial cartilage loss in a subsample from the Osteoarthritis Initiative progression subcohort. Osteoarthr Cartil. 2009;17(3):291–7.
Bloecker K, Wirth W, Guermazi A, et al. Relationship between medial meniscal extrusion and cartilage loss in specific femorotibial subregions: data from the osteoarthritis initiative. Arthritis Care Res (Hoboken). 2015;67(11):1545–52.
Chang A, Moisio K, Chmiel JS, et al. Subregional effects of meniscal tears on cartilage loss over 2 years in knee osteoarthritis. Ann Rheum Dis. 2011;70(1):74–9.
Buck RJ, Wyman BT, Le Graverand MP, Hudelmaier M, Wirth W, Eckstein F. Does the use of ordered values of subregional change in cartilage thickness improve the detection of disease progression in longitudinal studies of osteoarthritis? Arthritis Rheum. 2009;61(7):917–24.
Buck RJ, Wyman BT, Hellio Le Graverand MP, et al. Using ordered values of subregional cartilage thickness change incrleases sensitivity in detecting risk factors for osteoarthritis progression. Osteoarthr Cartil. 2011;19(3):302–8.
Wirth W, Buck R, Nevitt M, et al. MRI-based extended ordered values more efficiently differentiate cartilage loss in knees with and without joint space narrowing than region-specific approaches using MRI or radiography–data from the OA initiative. Osteoarthr Cartil. 2011;19(6):689–99.
Eckstein F, Wirth W, Lohmander LS, Hudelmaier MI, Frobell RB. Five-year followup of knee joint cartilage thickness changes after acute rupture of the anterior cruciate ligament. Arthritis Rheumatol. 2015;67(1):152–61.
Eckstein F, Buck R, Wirth W. Location-independent analysis of structural progression of osteoarthritis - taking it all apart, and putting the puzzle back together makes the difference. Semin Arthritis Rheum. 2017;46(4):404–10.
Eckstein F, Wax S, Aydemir A, Wirth W, Maschek S, Hochberg M. Intra-articular sprifermin reduces cartilage loss in addition to increasing cartilage gain independent of femorotibial location: a post-hoc analysis of a randomized, placebo-controlled phase ii clinical trial. Ann Rheum Dis. 2020;79(4):525–8.
Eckstein F, Wirth W, Guermazi A, Maschek S, Aydemir A. Intra-articular sprifermin not only increases cartilage thickness, but also reduces cartilage loss - location-independent post hoc analysis using MR imaging. Arthritis Rheumatol. 2015;67(11):2916–22.
Buck R, Hellio Le Graverand M-P, Hudelmaier M, Wirth W, Eckstein F. Detecting knee cartilage thickness change at three and six months. Osteoarthr Cartil. 2014;22(Supplement):S67.
Hunter DJ, Bowes MA, Eaton CB, et al. Can cartilage loss be detected in knee osteoarthritis (OA) patients with 3–6 months’ observation using advanced image analysis of 3T MRI? Osteoarthr Cartil. 2010;18(5):677–83.
Eckstein F, Mc Culloch CE, Lynch JA, et al. How do short-term rates of femorotibial cartilage change compare to long-term changes? Four year follow-up data from the osteoarthritis initiative. Osteoarthr Cartil. 2012;20(11):1250–7.
Buck RJ, Le Graverand MPH, Wirth W, Eckstein F. Choice of knee cartilage thickness change metric for different treatment goals in efficacy studies. Semin Arthritis Rheum. 2017;47(3):315–22.
Hunter DJ, Zhang W, Conaghan PG, et al. Systematic review of the concurrent and predictive validity of MRI biomarkers in OA. Osteoarthr Cartil. 2011;19(5):557–88.
Reichmann WM, Maillefert JF, Hunter DJ, Katz JN, Conaghan PG, Losina E (2011) Responsiveness to change and reliability of measurement of radiographic joint space width in osteoarthritis of the knee: a systematic review. Osteoarthr Cartil 19(1522–9653(Electronic)):550–556
Duryea J, Neumann G, Niu J, et al. Comparison of radiographic joint space width with magnetic resonance imaging cartilage morphometry: analysis of longitudinal data from the Osteoarthritis Initiative. Arthritis Care Res (Hoboken). 2010;62(7):932–7.
Eckstein F, Wirth W, Hudelmaier M, et al. Patterns of femorotibial cartilage loss in knees with neutral, varus, and valgus alignment. Arthritis Rheum. 2008;59(11):1563–70.
Eckstein F, Le Graverand MP, Charles HC, et al. Clinical, radiographic, molecular and MRI-based predictors of cartilage loss in knee osteoarthritis. Ann Rheum Dis. 2011;70(7):1223–30.
Pelletier JP, Raynauld JP, Berthiaume MJ, et al. Risk factors associated with the loss of cartilage volume on weight-bearing areas in knee osteoarthritis patients assessed by quantitative magnetic resonance imaging: a longitudinal study. Arthritis ResTher. 2007;9(4):R74.
Eckstein F, Nevitt M, Gimona A, et al. Rates of change and sensitivity to change in cartilage morphology in healthy knees and in knees with mild, moderate, and end-stage radiographic osteoarthritis : results from 831 participants from the osteoarthritis initiative. Arthritis Care Res (Hoboken). 2011;63(3):311–9.
Ding C, Martel-Pelletier J, Pelletier JP et al (2008) Two-year prospective longitudinal study exploring the factors associated with change in femoral cartilage volume in a cohort largely without knee radiographic osteoarthritis. Osteoarthr Cartil 16(1063–4584 (Print)):443–449
Brett A, Bowes MA, Conaghan PG, et al. Automated MRI assessment confirms cartilage thickness modification in patients with knee osteoarthritis: post-hoc analysis from a phase II sprifermin study. Osteoarthr Cartil. 2020;28(11):1432–6.
Eckstein F, Hochberg MC, Guehring H, et al. Long-term structural and symptomatic effects of intra-articular sprifermin in patients with knee osteoarthritis: 5-year results from the FORWARD study. Ann Rheum Dis. 2021;80(8):1062–9.
Wirth W, Benichou O, Kwoh CK, et al. Spatial patterns of cartilage loss in the medial femoral condyle in osteoarthritic knees: data from the Osteoarthritis Initiative. Magn Reson Med. 2010;63(3):574–81.
Buck RJ, Wirth W, Dreher D, Nevitt M, Eckstein F. Frequency and spatial distribution of cartilage thickness change in knee osteoarthritis and its relation to clinical and radiographic covariates - data from the osteoarthritis initiative. Osteoarthr Cartil. 2013;21(1):102–9.
Favero M, Ramonda R, Goldring MB, Goldring SR, Punzi L. Early knee osteoarthritis. RMD Open. 2015;1(Suppl 1):1–7.
Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502.
Buck RJ, Wyman BT, Le Graverand MP, Hudelmaier M, Wirth W, Eckstein F. Osteoarthritis may not be a one-way-road of cartilage loss - comparison of spatial patterns of cartilage change between osteoarthritic and healthy knees. Osteoarthr Cartil. 2010;18(3):329–35.
Hunter DJ, Deveza LA, Collins JE et al. Multivariable modeling of biomarker data from the phase 1 Foundation for the NIH Osteoarthritis Biomarkers Consortium. Arthritis Care Res (Hoboken)
van Helvoort EM, van Spil WE, Jansen MP, et al. Cohort profile: The Applied Public-Private Research enabling OsteoArthritis Clinical Headway (IMI-APPROACH) study: a 2-year, European, cohort study to describe, validate and predict phenotypes of osteoarthritis using clinical, imaging and biochemical mark. BMJ Open. 2020;10(7):e035101.
Hunter DJ, Zhang W, Conaghan PG et al (2011) Responsiveness and reliability of MRI in knee osteoarthritis: a meta-analysis of published evidence. Osteoarthr Cartil 19(1522–9653 (Electronic)):589–605
Roemer FW, Felson DT, Stefanik JJ, et al. Heterogeneity of cartilage damage in Kellgren and Lawrence grade 2 and 3 knees: the MOST study. Osteoarthr Cartil. 2022;30(5):714–23.
Roemer FW, Collins JE, Hunter DJ, Demehri S, Guermazi A. Patterns of progression differ between Kellgren-Lawrence 2 and 3 knees fulfilling different definitions of a cartilage-meniscus phenotype in the Foundation for National Institutes of Health Osteoarthritis Biomarkers study (FNIH). Osteoarthr Cartil Open. 2022;4(3):100284.
Altman RD, Gold GE. Atlas of individual radiographic features in osteoarthritis, revised. Osteoarthr Cartil. 2007;15(Suppl A):A1-56.
Wirth W, Nevitt M, Hellio Le Graverand MP, et al. Lateral and medial joint space narrowing predict subsequent cartilage loss in the narrowed, but not in the non-narrowed femorotibial compartment - data from the osteoarthritis initiative. Osteoarthr Cartil. 2014;22(1):63–70.
Schnitzer TJ, Pueyo M, Deckx H, et al. Efficacy and safety of s201086/GLPG1972, an ADAMTS-5 inhibitor, in patients with knee osteoarthritis: roccella, a 52-week, randomized, double-blind, dose-ranging phase 2 study. Osteoarthr Cartil. 2021;29:S264.
Roemer FW, Collins J, Kwoh CK, et al. MRI-based screening for structural definition of eligibility in clinical DMOAD trials: Rapid OsteoArthritis MRI Eligibility Score (ROAMES). Osteoarthr Cartil. 2020;28(1):71–81.
Wirth W, Maschek S, Wisser A, et al. Mri-based semi-quantitative assessment allows targeted selection of knees with accelerated quantitative cartilage thickness loss: data from the Oai Fnih Biomarker Consortium. Osteoarthr Cartil. 2022;2022(30):S264–5.
Guehring H, Moreau F, Daelken B, et al. The effects of sprifermin on symptoms and structure in a subgroup at risk of progression in the FORWARD knee osteoarthritis trial. Semin Arthritis Rheum. 2021;51(2):450–6.
McGuire D, Lane N, Segal N, et al. TPX-100 leads to marked, sustained improvements in subjects with knee osteoarthritis: pre-clinical rationale and results of a controlled clinical trial. Osteoarthr Cartil. 2018;2018(26):S243.
Bacon K, Lavalley MP, Jafarzadeh SR, Felson D. Does cartilage loss cause pain in osteoarthritis and if so, how much? Ann Rheum Dis. 2020;79(8):1105–10.
Binvignat M, Pedoia V, Butte AJ, et al. Use of machine learning in osteoarthritis research: a systematic literature review. RMD Open. 2022;8(1):1–10.
Jamshidi A, Leclercq M, Labbe A, et al. Identification of the most important features of knee osteoarthritis structural progressors using machine learning methods. Ther Adv Musculoskelet Dis. 2020;12:1–12.
Guan B, Liu F, Haj-Mirzaian A, et al. Deep learning risk assessment models for predicting progression of radiographic medial joint space loss over a 48-MONTH follow-up period. Osteoarthr Cartil. 2020;28(4):428–37.
Guermazi A, Eckstein F, Hayashi D, et al. Baseline radiographic osteoarthritis and semi-quantitatively assessed meniscal damage and extrusion and cartilage damage on MRI is related to quantitatively defined cartilage thickness loss in knee osteoarthritis: the Multicenter Osteoarthritis Study. Osteoarthr Cartil. 2015;23(12):2191–8.
Maschek S, Roemer FW, Marijnissen AC, et al. Predictors of longitudinal Mri-based cartilage thickness change in the observational multicenter approach cohort. Osteoarthr Cartil. 2022;2022(30):S45–6.
Guermazi A, Niu J, Hayashi D, et al. Prevalence of abnormalities in knees detected by MRI in adults without knee osteoarthritis: population based observational study (Framingham Osteoarthritis Study). BMJ. 2012;345:e5339.
Eckstein F, Maschek S, Roemer FW, Duda GN, Sharma L, Wirth W. Cartilage loss in radiographically normal knees depends on radiographic status of the contralateral knee – data from the Osteoarthritis Initiative. Osteoarthr Cartil. 2019;27(2):273–7.
Funding
Open access funding provided by Paracelsus Medical University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Wolfgang Wirth: employee and shareholder of Chondrometrics GmbH. Susanne Maschek: employee and shareholder of Chondrometrics GmbH. Anna Wisser: employee of Chondrometrics GmbH. Felix Eckstein: CEO and shareholder of Chondrometrics GmbH and received personal fees from AbbVie, Galapagos NV, HealthLink, ICM, IRIS, Kolon TissueGene, Merck KGaA, Novartis, Roche and Samumed and grants from Foundation for the NIH, University of California, San Francisco, NIH/National Heart, Lung, and Blood Institute, Bioclinica, Galapagos NV, Novartis, TissueGene, Erlangen University Hospital, University of Sydney, CALIBR, University of Basel, University of Western Ontario, Stanford University, ICM Co., Ltd., UMC Utrecht, Federal Ministry of Education and Research, Germany. Christoph Ladel received personal fees from LinkHealth Wengzhou, ReumaNederland Amsterdam, UMC Utrecht, Charité Hospital Berlin. Frank Roemer: shareholder of Boston Imaging Core Lab. (BICL), LLC. He is consultant to Calibr and Grünenthal.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
• MRI-based cartilage morphometry is sensitive to osteoarthritis-related change and also to treatment interventions and is nowadays widely used as outcome measure in observational studies as well as randomized interventional trials
• Cartilage morphometry has been reported to be highly accurate and reproducible
• Imaging sequences suitable for cartilage morphometry are available for most of the currently installed 1.5 T and 3 T scanners but are not used in a clinical setting due to relatively long acquisition times
• Two of the recent interventional clinical trials relying on cartilage morphometry as structural outcome measure showed structural benefits and one of these trials showed a dose–response effect on structural progression.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wirth, W., Ladel, C., Maschek, S. et al. Quantitative measurement of cartilage morphology in osteoarthritis: current knowledge and future directions. Skeletal Radiol 52, 2107–2122 (2023). https://doi.org/10.1007/s00256-022-04228-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-022-04228-w