Abstract
Background
Angiolipomas are benign subcutaneous nodules that are commonly multifocal and easily overlooked by those not familiar with their appearance. The objective of this study was to identify the spectrum of the clinical and imaging features of this lesion, to include MR, CT, and US features.
Methods
A retrospective review of our institutional pathology database for biopsy-proven cases of angiolipoma between January 1, 2019, through December 31, 2021, was done. We identified 334 patients who underwent surgical resection of 788 individual lesions. MR imaging studies were available in 43 cases, CT in 39 cases, and ultrasound imaging in 72 cases. Clinical features (patient age, gender, surgical indication, number of lesions) were reviewed. Imaging feature analysis included the anatomic location, content of fat, vascularity, and modality-specific imaging features.
Results
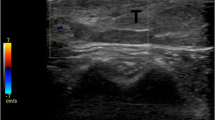
All 778 angiolipomas were located in the subcutaneous tissues (median size, 2.4 cm, range 0.4–7.7 cm), with over 51% located in the upper extremity. The most common presentation was a symptomatic mass or slowly growing symptomatic mass. Imaging showed a subcutaneous lesion with a lobulated bean shape, which typically abutted the skin. Intralesional fat was identified in 85% of lesions on CT and MRI. Vessels were commonly seen on CT and MR, with enhancement best seen on MR. On US, lesions were heterogeneous and mildly hyperechoic, most often with no identifiable vascularity.
Conclusion
Angiolipomas typically have characteristic imaging features. Awareness of this diagnosis and the spectrum of its imaging features is important and can facilitate a definitive diagnosis.












Similar content being viewed by others
References
Sciot R, Nielsen G. Angiolipoma. In: Lokuhetty D, White V, Cree I, editors. WHO classification of tumours, soft tissue and bone tumors. 5th ed. Lyon Cedex, France: International Agency for Research on Cancer (IARC); 2020. p. 23–4.
Goldblum JR, Folpe AL, Weiss S. Soft tussue tumors. 7th ed. Philadelphia, PA: Elsevier; 2020. p. 476–519.
Bowen JT. Multiple subcutaneous hemangiomas, together with multiple lipomas, occurring in enormous numbers in an otherwise healthy muscular subject. Am J Med Sci. 1912;114:189–92.
Klem KK. Multiple lipoma-angiolipomas. Acta Chir Scand. 1949;97(6):527–32.
Howard WR, Helwig EB. Angiolipoma. Arch Dermatol. 1960;82:924–31.
Hofvander J, Arbajian E, Stenkula KG, Lindkvist-Petersson K, Larsson M, Nilsson J, et al. Frequent low-level mutations of protein kinase D2 in angiolipoma. J Pathol. 2017;241(5):578–82.
Saggini A, Santonja C, Najera L, Palmedo G, Kutzner H. Frequent activating PIK3CA mutations in sporadic angiolipoma. J Cutan Pathol. 2021;48(2):211–6.
Sheng W, Lu L, Wang J. Cellular angiolipoma: a clinicopathological and immunohistochemical study of 12 cases. Am J Dermatopathol. 2013;35(2):220–5.
Gonzalez-Crussi F, Enneking WF, Arean VM. Infiltrating angiolipoma. J Bone Joint Surg Am. 1966;48(6):1111–24.
Calonje JE. Intramuscular angioma. In: Lokuhetty D, White V, Cree I, editors. WHO classification of tumours, soft tissue and bone tumors. 5th ed. France International Agency for Research on Cancer IARC: Lyon Cedex; 2020. p. 145–6.
Bang M, Kang BS, Hwang JC, Weon YC, Choi SH, Shin SH, et al. Ultrasonographic analysis of subcutaneous angiolipoma. Skeletal Radiol. 2012;41(9):1055–9.
Shin YS, Kim YJ, Park IS, Chu YC, Kim JH, Lee HY, et al. Sonographic differentiation between angiolipomas and superficial lipomas. J Ultrasound Med. 2016;35(11):2421–9.
Grivas TB, Savvidou OD, Psarakis SA, Liapi G, Triantafyllopoulos G, Kovanis I, et al. Forefoot plantar multilobular noninfiltrating angiolipoma: a case report and review of the literature. World J Surg Oncol. 2008;6:11.
MG Karaali AK Polat AE Koku Aksu C Leblebici MS Gurel Solitary noninfiltrating angiolipoma on the finger an unusual localization Dermatol Online J 2019 25 2
Morris RW, Al Hmada Y, Chaudry JR, Nutter KM, Reed CD. Multiple bilateral forearm nodules. Skeletal Radiol. 2020;49(4):657–8.
Morris RW, Al Hmada Y, Chaudry JR, Nutter KM, Reed CD. Multiple bilateral forearm nodules. Skeletal Radiol. 2020;49(4):641–3.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kransdorf, M.J., Larsen, B.T., Goulding, K.A. et al. Angiolipoma: a review of 778 lesions in 344 patients. Skeletal Radiol 52, 541–552 (2023). https://doi.org/10.1007/s00256-022-04075-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-022-04075-9